Abstract
Purpose
To examine ovarian cancer survivors’ adherence to evidence-based guidelines for preventive health care.
Methods
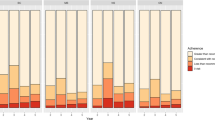
A case-control, retrospective study of Medicare fee-for-service beneficiaries diagnosed with stage I, II, or III epithelial ovarian cancer from 2001 to 2010 using the Surveillance, Epidemiology, and End Results-Medicare database. Survivors were matched 1:1 to non-cancer controls from the 5% Medicare Beneficiary file on age, race, state of residence, and follow-up time. Receipt of flu vaccination, mammography, and bone density tests were examined in accordance with national guidelines. Adherence was assessed starting 1 year after cancer diagnosis, across 2 years of claims. Interaction with the health care system, including outpatient and cancer surveillance visits, was tested as a potential mechanism for receipt of services.
Results
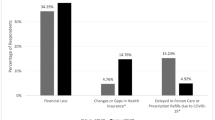
2437 survivors met the eligibility criteria (mean age, 75; 90% white). Ovarian cancer survivors were more likely to be adherent to flu vaccination (5 percentage points (pp); < 0.001) and mammography guidelines (10 pp.; < 0.001) compared to non-cancer controls, but no differences were found for bone density test guidelines (− 1 pp.; NS). Black women were less likely to be adherent to flu vaccination and bone density tests compared with white women. Women dually eligible for Medicare and Medicaid were less likely to be adherent compared to those without such support. Adherence was not influenced by measures of outpatient visits.
Conclusion
Ovarian cancer survivors are receiving preventive services with the same or better adherence than their matched counterparts. Minority and dual-eligible survivors received preventive services at a lower rate than white survivors and those with higher income. The number of outpatient visits was not associated with increased preventive health visits.
Implications for Cancer Survivors
Ovarian cancer survivors are receiving adequate follow-up care to be adherent to preventive health measures. Efforts to improve care coordination post-treatment may help reduce minority and low SES disparities.
Similar content being viewed by others
References
Society AC. Cancer treatment & survivorship facts & figures 2014–2015. Atlanta: American Cancer Society; 2014. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-treatment-and-survivorship-facts-and-figures/cancer-treatment-and-survivorship-facts-and-figures-2014-2015.pdf. Accessed Apr 2016.
Malvezzi M, Carioli G, Rodriguez T, Negri E, La Vecchia C. Global trends and predictions in ovarian cancer mortality. Ann Oncol. 2016;27:2017–25. https://doi.org/10.1093/annonc/mdw306.
Centers for Disease Control and Prevention AoA. Agency for healthcare research and quality, and centers for medicare and medicaid services. Enhancing use of clinical preventive services among older adults. Washington, DC: Centers for disease control and prevention, administration on aging, agency for healthcare research and quality, Centers for Medicare and Medicaid Services; 2011. https://www.cdc.gov/aging/pdf/clinical_preventive_services_closing_the_gap_report.pdf. Accessed Apr 2016.
Force USPST. Recommendation summary: breast cancer screening. In: Recommendations for primary care practice. 2009. http://www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/breast-cancer-screening. Accessed Apr 2016.
Force USPST. Recommendation summary: osteoporosis screening. In: Recommendations for primary care practice. 2011. http://www.uspreventiveservicestaskforce.org/uspstf/uspsoste.htm. Accessed Apr 2016.
Oncology SoG. Ovarian cancer treatment summary and survivorship care plan. Available from https://www.sgo.org/wp-content/uploads/2018/06/2018-Ovarian-Cancer-Survivorship-Plan-FWC-SGO.pdf. Accessed Jan 2019.
Khan NF, Carpenter L, Watson E, Rose PW. Cancer screening and preventative care among long-term cancer survivors in the United Kingdom. Br J Cancer. 2010;102(7):1085–90. https://doi.org/10.1038/sj.bjc.6605609.
Bellizzi KM, Rowland JH, Jeffery DD, McNeel T. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005;23(34):8884–93. https://doi.org/10.1200/JCO.2005.02.2343.
Duffy CM, Clark MA, Allsworth JE. Health maintenance and screening in breast cancer survivors in the United States. Cancer Detect Prev. 2006;30(1):52–7. https://doi.org/10.1016/j.cdp.2005.06.012.
Hudson SV, Hahn KA, Ohman-Strickland P, Cunningham RS, Miller SM, Crabtree BF. Breast, colorectal and prostate cancer screening for cancer survivors and non-cancer patients in community practices. J Gen Intern Med. 2009;24(Suppl 2):S487–90. https://doi.org/10.1007/s11606-009-1036-3.
Trask PC, Rabin C, Rogers ML, Whiteley J, Nash J, Frierson G, et al. Cancer screening practices among cancer survivors. Am J Prev Med. 2005;28(4):351–6. https://doi.org/10.1016/j.amepre.2005.01.005.
Earle CC, Burstein HJ, Winer EP, Weeks JC. Quality of non-breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol. 2003;21(8):1447–51. https://doi.org/10.1200/JCO.2003.03.060.
Earle CC, Neville BA. Under use of necessary care among cancer survivors. Cancer. 2004;101(8):1712–8. https://doi.org/10.1002/cncr.20560.
Yu X, McBean AM, Virnig BA. Physician visits, patient comorbidities, and mammography use among elderly colorectal cancer survivors. J Cancer Surviv. 2007;1(4):275–82. https://doi.org/10.1007/s11764-007-0037-7.
Snyder CF, Frick KD, Herbert RJ, Blackford AL, Neville BA, Carducci MA, et al. Preventive care in prostate cancer patients: following diagnosis and for five-year survivors. J Cancer Surviv. 2011;5(3):283–91. https://doi.org/10.1007/s11764-011-0181-y.
Baldwin L-M, Dobie SA, Cai Y, Saver BG, Green PK, Wang CY. Receipt of general medical care by colorectal cancer patients: a longitudinal study. J Am Board Fam Med. 2011;24(1):57–68. https://doi.org/10.3122/jabfm.2011.01.100080.
McBean AM, Yu X, Virnig BA. The use of preventive health services among elderly uterine cancer survivors. Am J Obstet Gynecol. 2008;198(1):86 e1–8. https://doi.org/10.1016/j.ajog.2007.05.036.
Uhlig A, Mei J, Baik I, Meyer C, Uhlig J. Screening utilization among cancer survivors: a meta-analysis. J Public Health. 2018;40(1):129–37. https://doi.org/10.1093/pubmed/fdx030.
Corkum M, Hayden JA, Kephart G, Urquhart R, Schlievert C, Porter G. Screening for new primary cancers in cancer survivors compared to non-cancer controls: a systematic review and meta-analysis. J Cancer Surviv. 2013;7(3):455–63. https://doi.org/10.1007/s11764-013-0278-6.
Bishop MM, Lee SJ, Beaumont JL, Andrykowski MA, Rizzo JD, Sobocinski KA, et al. The preventive health behaviors of long-term survivors of cancer and hematopoietic stem cell transplantation compared with matched controls. Biol Blood Marrow Transplant. 2010;16(2):207–14. https://doi.org/10.1016/j.bbmt.2009.09.015.
Breslau ES, Jeffery DD, Davis WW, Moser RP, McNeel TS, Hawley S. Cancer screening practices among racially and ethnically diverse breast cancer survivors: results from the 2001 and 2003 California health interview survey. J Cancer Surviv. 2010;4(1):1–14. https://doi.org/10.1007/s11764-009-0102-5.
Aparicio-Ting F, Ramirez AG. Breast and cervical cancer knowledge, attitudes, and screening practices of Hispanic women diagnosed with cancer. J Cancer Educ. 2003;18(4):230–6. https://doi.org/10.1207/s15430154jce1804_11.
Mayer DK, Terrin NC, Menon U, Kreps GL, McCance K, Parsons SK, et al. Screening practices in cancer survivors. J Cancer Surviv. 2007;1(1):17–26. https://doi.org/10.1007/s11764-007-0007-0.
Fairley TL, Hawk H, Pierre S. Health behaviors and quality of life of cancer survivors in Massachusetts, 2006: data use for comprehensive cancer control. Prev Chronic Dis. 2010;7(1):A09.
Snyder CF, Frick KD, Kantsiper ME, Peairs KS, Herbert RJ, Blackford AL, et al. Prevention, screening, and surveillance care for breast cancer survivors compared with controls: changes from 1998 to 2002. J Clin Oncol. 2009;27(7):1054–61. https://doi.org/10.1200/JCO.2008.18.0950.
Grunfeld E, Moineddin R, Gunraj N, Del Giudice ME, Hodgson DC, Kwon JS, et al. Cancer screening practices of cancer survivors population-based, longitudinal study. Can Fam Physician. 2012;58(9):980–6.
Lowenstein LM, Ouellet JA, Dale W, Fan L, Mohile SG. Preventive care in older cancer survivors. J Geriatr Oncol. 2015;6(2):85–92. https://doi.org/10.1016/j.jgo.2014.12.003.
Lafata JE, Salloum RG, Fishman PA, Ritzwoller DP, O’Keeffe-Rosetti MC, Hornbrook MC. Preventive care receipt and office visit use among breast and colorectal cancer survivors relative to age-and gender-matched cancer-free controls. J Cancer Surviv. 2015;9(2):201–7. https://doi.org/10.1007/s11764-014-0401-3.
Homan SG, Kayani N, Yun S. Peer reviewed: risk factors, preventive practices, and health care among breast cancer survivors, United States, 2010. Prev Chronic Dis. 2016;13.
Pollack LA, Adamache W, Ryerson AB, Eheman CR, Richardson LC. Care of long-term cancer survivors: physicians seen by Medicare enrollees surviving longer than 5 years. Cancer. 2009;115(22):5284–95. https://doi.org/10.1002/cncr.24624.
Snyder CF, Earle CC, Herbert RJ, Neville BA, Blackford AL, Frick KD. Preventive care for colorectal cancer survivors: a 5-year longitudinal study. J Clin Oncol. 2008;26(7):1073–9. https://doi.org/10.1200/JCO.2007.11.9859.
Bristow ER, Chang RJ, Ziogas RA, Campos RB, Chavez RL, Anton-Culver RH. Sociodemographic disparities in advanced ovarian cancer survival and adherence to treatment guidelines. Obstet Gynecol. 2015;125(4):833–42. https://doi.org/10.1097/AOG.0000000000000643.
Bristow RE, Powell MA, Al-Hammadi N, Chen L, Miller JP, Roland PY, et al. Disparities in ovarian cancer care quality and survival according to race and socioeconomic status. J Natl Cancer Inst. 2013;105(11):823–32. https://doi.org/10.1093/jnci/djt065.
Institute NC. SEER-Medicare: Brief description of the SEER-Medicare database. National Cancer Institute. 2017. https://healthcaredelivery.cancer.gov/seermedicare/overview/. Accessed Apr 2016.
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40(8):IV3–IV18. https://doi.org/10.2307/3767919.
Institute NC. SEER-Medicare: About the data files. 2017. https://healthcaredelivery.cancer.gov/seermedicare/aboutdata/. Accessed Apr 2016.
Snyder CF, Frick KD, Peairs KS, Kantsiper ME, Herbert RJ, Blackford AL, et al. Comparing care for breast cancer survivors to non-cancer controls: a five-year longitudinal study. J Gen Intern Med. 2009;24(4):469–74. https://doi.org/10.1007/s11606-009-0903-2.
Oncology SoG. Self care plan: what you can do to stay healthy after treatment for cancer; 2016. https://www.sgo.org/wp-content/uploads/2016/08/Gynecologic-Cancer-Self-Care-Plan-FINAL.pdf. Accessed Apr 2016.
Jaen CR, Nutting PA, Stange KC. Competing demands of primary care: a model for the delivery of clinical preventive services. J Fam Pract. 1994;38(2).
Bach PB, Guadagnoli E, Schrag D, Schussler N, Warren JL. Patient demographic and socioeconomic characteristics in the SEER-Medicare database applications and limitations. Med Care. 2002;40(8 Suppl):IV-19–25. https://doi.org/10.1097/01.MLR.0000020934.40692.C0.
Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258–67. https://doi.org/10.1016/S0895-4356(00)00256-0.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51.
Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46(10):1075–9.
Charlson ME, Pompei P, Ales KA, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Institute NC. SEER-Medicare: Calculation of comorbidity weights. https://healthcaredelivery.cancer.gov/seermedicare/considerations/calculation.html. Accessed Apr 2016.
Prat J. Staging classification for cancer of the ovary, fallopian tube, and peritoneum. Int J Gynecol Obstet. 2014;124(1):1–5. https://doi.org/10.1016/j.ijgo.2013.10.001.
Prevention CfDCa. Cancer, the flu, and you. https://www.cdc.gov/cancer/flu/index.htm. Accessed Apr 2016.
Society AC. What are the risk factors for ovarian cancer? 2016. https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html. Accessed Apr 2016.
Martin JY, Schiff MA, Weiss NS, Urban RR. Racial disparities in the utilization of preventive health services among older women with early-stage endometrial cancer enrolled in Medicare. Cancer Med. 2017;6(9):2153–63. https://doi.org/10.1002/cam4.1141.
Austin S, Martin MY, Kim Y, Funkhouser EM, Partridge EE, Pisu M. Disparities in use of gynecologic oncologists for women with ovarian cancer in the United States. Health Serv Res. 2013;48(3):1135–53. https://doi.org/10.1111/1475-6773.12012.
Fairfield KM, Murray K, LaChance JA, Wierman HR, Earle CC, Trimble EL, et al. Intraperitoneal chemotherapy among women in the Medicare population with epithelial ovarian cancer. Gynecol Oncol. 2014;134(3):473–7. https://doi.org/10.1016/j.ygyno.2014.06.011.
Fairfield KM, Lucas FL, Earle CC, Small L, Trimble EL, Warren JL. Regional variation in cancer-directed surgery and mortality among women with epithelial ovarian cancer in the Medicare population. Cancer. 2010;116(20):4840–8. https://doi.org/10.1002/cncr.25242.
Collins Y, Holcomb K, Chapman-Davis E, Khabele D, Farley JH. Gynecologic cancer disparities: a report from the health disparities taskforce of the Society of Gynecologic Oncology. Gynecol Oncol. 2014;133(2):353–61.
Chase DM, Fedewa S, Chou TS, Chen A, Ward E, Brewster WR. Disparities in the allocation of treatment in advanced ovarian cancer: are there certain patient characteristics associated with nonstandard therapy? Obstet Gynecol. 2012;119(1):68–77.
Terplan M, Schluterman N, McNamara EJ, Tracy JK, Temkin SM. Have racial disparities in ovarian cancer increased over time? An analysis of SEER data. Gynecol Oncol. 2012;125(1):19–24.
Gorin SS, Haggstrom D, Han PK, Fairfield KM, Krebs P, Clauser SB. Cancer care coordination: a systematic review and meta-analysis of over 30 years of empirical studies. Ann Behav Med. 2017;51(4):532–46. https://doi.org/10.1007/s12160-017-9876-2.
Natale-Pereira A, Enard KR, Nevarez L, Jones LA. The role of patient navigators in eliminating health disparities. Cancer. 2011;117(S15):3541–50.
Hewitt ME, Bamundo A, Day R, Harvey C. Perspectives on post-treatment cancer care: qualitative research with survivors, nurses, and physicians. J Clin Oncol. 2007;25(16):2270–3.
Society AC. Ovarian cancer detailed guide: ovarian cancer survival rates. In: Learn about cancer. 2014. http://www.cancer.org/cancer/ovariancancer/detailedguide/ovarian-cancer-survival-rates. Accessed Apr 2016.
Lockwood-Rayermann S. Survivorship issues in ovarian cancer: a review. Oncol Nurs Forum. 2006;33(3):9–562. https://doi.org/10.1188/06.ONF.553-562.
Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7(3):300–22. https://doi.org/10.1007/s11764-013-0272-z.
Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40(5):395–404.
Mojtabai R, Olfson M. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Aff. 2003;22(4):220–9.
Hwang S, Jayadevappa R, Zee J, Zivin K, Bogner HR, Raue PJ, et al. Concordance between clinical diagnosis and Medicare claims of depression among older primary care patients. Am J Geriatr Psychiatry. 2015;23(7):726–34. https://doi.org/10.1016/j.jagp.2014.08.009.
Watts S, Prescott P, Mason J, McLeod N, Lewith G. Depression and anxiety in ovarian cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open. 2015;5(11):e007618. https://doi.org/10.1136/bmjopen-2015-007618.
Zeng C, Wen W, Morgans AK, Pao W, Shu X-O, Zheng W. Disparities by race, age, and sex in the improvement of survival for major cancers: results from the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) Program in the United States, 1990 to 2010. JAMA Oncol. 2015;1(1):88–96.
Vargas RB, Ryan GW, Jackson CA, Rodriguez R, Freeman HP. Characteristics of the original patient navigation programs to reduce disparities in the diagnosis and treatment of breast cancer. Cancer. 2008;113(2):426–33. https://doi.org/10.1002/cncr.23547.
Temkin SM, Rimel B, Bruegl AS, Gunderson CC, Beavis AL, Doll KM. A contemporary framework of health equity applied to gynecologic cancer care: a Society of Gynecologic Oncology evidenced-based review. Gynecol Oncol. 2018;149(1):70–7.
Acknowledgments
The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Healthcare Delivery Research Program, National Cancer Institute; the Office of Research, Development, and Information, CMS; Information Management Services, Inc.; and the Surveillance, Epidemiology, and End Results (SEER) program tumor registries in the creation of the SEER-Medicare database. The authors thank Renjian Jiang for initial data compilation and for providing technical support for use of SEER-Medicare files.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study was approved by the Emory University Institutional Review Board (IRB). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
A complete waiver of HIPAA authorization and informed consent was reviewed and approved under 45 CFR 46.116(d) by the Emory University IRB.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Loomer, L., Ward, K.C., Reynolds, E.A. et al. Racial and socioeconomic disparities in adherence to preventive health services for ovarian cancer survivors. J Cancer Surviv 13, 512–522 (2019). https://doi.org/10.1007/s11764-019-00771-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-019-00771-z