Abstract
Background/Objective
One of the most effective treatments for patients with obesity, albeit with some complications, is obesity surgery. The aim of this study was to develop a clinical decision support system (CDSS) to predict the early complications of one-anastomosis gastric bypass (OAGB) surgery.
Subjects/Methods
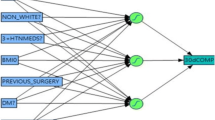
This study was conducted in Tehran, Iran on patients who underwent OAGB surgery in 2011–2014 in five hospitals. Initially, variables affecting the OAGB early complications were identified using the literature review. Patients’ data were extracted from an existing database of obesity surgery. Then, different artificial neural networks (ANNs) (multilayer perceptron (MLP) network) were developed and evaluated for prediction of 10-day, 1-month, and 3-month complications.
Results
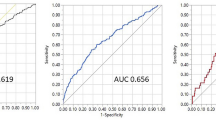
Factors including age, BMI, smoking status, intra-operative complications, comorbidities, laboratory tests, sonography results, and endoscopy results were considered important factors for predicting early complications of OAGB. A CDSS was developed with these variables. The accuracy, specificity, and sensitivity of the 10-day prediction system in the test data were 98.4%, 98.6%, and 98.3%, respectively. These figures for 1-month system were 96%, 93%, and 98.4% and for the 3-month system were 89.3%, 86.6%, and 91.5%, respectively.
Conclusions
Using the CDSS designed, we could accurately predict the early complications of OAGB surgery.




Similar content being viewed by others
References
Jafari-Adli S, Jouyandeh Z, Qorbani M, et al. Prevalence of obesity and overweight in adults and children in Iran; a systematic review. J Diabetes Metab Disord. 2014;13(1):121.
Chaim EA, Ramos AC, Cazzo E. Mini-gastric bypass: description of the technique and preliminary results. ABCD Arquivos Brasileiros de Cirurgia Digestiva (São Paulo). 2017;30(4):264–6.
Khurram M, Paracha SJ, Hamama-tul-Bushra Khar ZH. Obesity related complications in 100 obese subjects and their age matched controls. J Pak Med Assoc. 2006;56(50)
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Fazel I. Surgical treatment of morbid obesity. Iran J Surg. 2011;19(2):1–21.
Georgiadou D, Sergentanis TN, Nixon A, et al. Efficacy and safety of laparoscopic mini gastric bypass. A systematic review. Surg Obes Relat Dis. 2014;10(5):984–91.
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11(3):276–80.
Park HJ, Hong SS, Hwang J, et al. Mini-gastric bypass to control morbid obesity and diabetes mellitus: what radiologists need to know. Korean J Radiol. 2015;16(2):325–33.
Genser L, Carandina S, Tabbara M, et al. Presentation and surgical management of leaks after mini–gastric bypass for morbid obesity. Surg Obes Relat Dis. 2016;12(2):305–12.
Abraham A, Ikramuddin S, Jahansouz C, et al. Trends in bariatric surgery: procedure selection, revisional surgeries, and readmissions. Obes Surg. 2016;26(7):1371–7.
Arterburn DE, Courcoulas AP. Bariatric surgery for obesity and metabolic conditions in adults. BMJ. 2014;349:3961.
Lee CW, Kelly JJ, Wassef WY. Complications of bariatric surgery. Curr Opin Gastroenterol. 2007;23(6):636–43.
Chiappetta S, Stier C, Squillante S, et al. The importance of the Edmonton obesity staging system in predicting postoperative outcome and 30-day mortality after metabolic surgery. Surg Obes Relat Dis. 2016;12(10):1847–55.
Janik MR, Walędziak M, Brągoszewski J, et al. Prediction model for hemorrhagic complications after laparoscopic sleeve gastrectomy: development of sleeve bleed calculator. Obes Surg. 2017;27(4):968–72.
Gupta PK, Franck C, Miller WJ, et al. Development and validation of a bariatric surgery morbidity risk calculator using the prospective, multicenter NSQIP dataset. J Am Coll Surg. 2011;212(3):301–9.
Coblijn UK, Lagarde SM, de Raaff CA, et al. Evaluation of the obesity surgery mortality risk score for the prediction of postoperative complications after primary and revisional laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016;12(8):1504–12.
Omidian Z, Hadianfard A. The study of clinical decision support systems role in health care(1980-2010). Jundishapur J Health Res. 2011;2(3):1–13.
Paydar K, Kalhori SRN, Akbarian M, et al. A clinical decision support system for prediction of pregnancy outcome in pregnant women with systemic lupus erythematosus. Int J Med Inform. 2017;97:239–46.
Sadoughi F, Sheikhtaheri A. Applications of artificial intelligence in clinical decision making: opportunities and challenges. Health Information Management. 2011;8(19):440–5.
Han J, Pei J, Kamber M. Data mining: concepts and techniques: Elsevier; 2011.
Chawla NV, Bowyer KW, Hall LO, et al. SMOTE: synthetic minority over-sampling technique. J Artif Intell Res. 2002;16:321–57.
Pourshahriar H, Tabatabaiei KR, Khodapanahi MK, et al. Artificial neural networks: a model for prediction. Developmental Psychology (Journal of Iranian Psychologists). 2009;5(20):307–21.
Sheikhtaheri A, Sadoughi F, Dehaghi ZH. Developing and using expert systems and neural networks in medicine: a review on benefits and challenges. J Med Syst. 2014;38(9):110.
Rathore H. Mapping biological systems to network systems: Springer; 2016.
Bounds DG, Lloyd PJ, Mathew BG. A comparison of neural network and other pattern recognition approaches to the diagnosis of low back disorders. Neural Netw. 1990;3(5):583–91.
Li C, Zhi X, Ma J, et al. Performance comparison between logistic regression, decision trees, and multilayer perceptron in predicting peripheral neuropathy in type 2 diabetes mellitus. Chin Med J. 2012;125(5):851–7.
Raad A, Kalakech A, Ayache M. Breast cancer classification using neural network approach: MLP and RBF. Networks. 2012;7(8):9.
Zhu W, Zeng N, Wang N. Sensitivity, specificity, accuracy, associated confidence interval and ROC analysis with practical SAS implementations. NESUG proceedings: health care and life sciences, Baltimore, Maryland 2010:1–9.
Almulaifi AM, Ser KH, Lee WJ. Acute gastric remnant dilatation, a rare early complication of laparoscopic mini-gastric bypass. Asian J Endosc Surg. 2014;7(2):185–7.
Birkmeyer JD, Finks JF, O'Reilly A, et al. Surgical skill and complication rates after bariatric surgery. N Engl J Med. 2013;369(15):1434–42.
Bruzzi M, Voron T, Zinzindohoue F, et al. Revisional single-anastomosis gastric bypass for a failed restrictive procedure: 5-year results. Surg Obes Relat Dis. 2016;12(2):240–5.
Currò G, La Malfa G, Caizzone A, et al. Three-dimensional (3D) versus two-dimensional (2D) laparoscopic bariatric surgery: a single-surgeon prospective randomized comparative study. Obes Surg. 2015;25(11):2120–4.
Inabnet WB, Belle SH, Bessler M, et al. Comparison of 30-day outcomes after non-Lap Band primary and revisional bariatric surgical procedures from the longitudinal assessment of bariatric surgery study. Surg Obes Relat Dis. 2010;6(1):22–30.
Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-En-Y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg. 2016;26(5):926–32.
Kansou G, Lechaux D, Delarue J, et al. Laparoscopic sleeve gastrectomy versus laparoscopic mini gastric bypass: one year outcomes. Int J Surg. 2016;33:18–22.
Lee W-J, Ser K-H, Lee Y-C, et al. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22(12):1827–34.
Mason ME, Jalagani H, Vinik AI. Metabolic complications of bariatric surgery: diagnosis and management issues. Gastroenterol Clin N Am. 2005;34(1):25–33.
Musella M, Susa A, Greco F, et al. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multicenter review. Surg Endosc. 2014;28(1):156–63.
Noun R, Skaff J, Riachi E, et al. One thousand consecutive mini-gastric bypass: short- and long-term outcome. Obes Surg. 2012;22(5):697–703.
Padwal R, Klarenbach S, Wiebe N, et al. Bariatric surgery: a systematic review and network meta analysis of randomized trials. Obes Rev. 2011;12(8):602–21.
Parmar C, Mahawar K, Boyle M, et al. Mini gastric bypass: first report of 125 consecutive cases from United Kingdom. Clin Obes. 2016;6(1):61–7.
Piazza L, Di Stefano C, Ferrara F, et al. Revision of failed primary adjustable gastric banding to mini-gastric bypass: results in 48 consecutive patients. Updat Surg. 2015;67(4):433–7.
Salgado Jr W, De Queiroz Cunha F, Dos Santos JS, et al. Early identification of infectious complications in bariatric surgery by the determination of peritoneal and systemic cytokines. Obes Surg. 2009;19(7):867–72.
Stenberg E, Szabo E, Ågren G, et al. Early complications after laparoscopic gastric bypass surgery: results from the Scandinavian obesity surgery registry. Ann Surg. 2014;260(6):1040–7.
Tambasco D, D’ettorre M, Gentileschi S, et al. Postabdominoplasty wound dehiscence in bariatric patients: biliopancreatic diversion versus gastric bypass: a preliminary study. Ann Plast Surg. 2015;75(6):588–90.
Umemura A, Lee WJ, Sasaki A, et al. History and current status of bariatric and metabolic surgeries in East Asia. Asian J Endosc Surg. 2015;8(3):268–74.
Wrzesinski A, Correa JM, Fernandes TMB, et al. Complications requring hospital management after bariatric surgery. ABCD Arq Bras Cir Dig. 2015;28(Supl.1):3–6.
Yang P-J, Lee W-J, Tseng P-H, et al. Bariatric surgery decreased the serum level of an endotoxin-associated marker: lipopolysaccharide-binding protein. Surg Obes Relat Dis. 2014;10(6):1182–7.
Mahawar KK, Jennings N, Brown J, et al. “Mini” gastric bypass: systematic review of a controversial procedure. Obes Surg. 2013;23(11):1890–8.
Madah G, Shabahang H, Barband M, et al. Outcomes and complications of Roux-en-Y open gastric bypass in morbid obesity: a short report. Tehran Univ Med J. 2014;72(9):643–7.
Manassa EH, Hertl CH, Olbrisch R-R. Wound healing problems in smokers and nonsmokers after 132 abdominoplasties. Plast Reconstr Surg. 2003;111(6):2082–7.
Acknowledgements
This study is supported by Iran University of Medical Sciences, Tehran, Iran (IUMS/SHMIS-1395.9311304002). Additionally, we appreciate National Obesity Surgery Registry to provide data for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict(s) of interest.
Informed Consent
For this type of study, formal consent is not required.
Ethical Approval
The protocol of this study was reviewed and approved by the ethics committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.REC 1395.9311304002). All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Financial Support
This study did not receive any financial support.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sheikhtaheri, A., Orooji, A., Pazouki, A. et al. A Clinical Decision Support System for Predicting the Early Complications of One-Anastomosis Gastric Bypass Surgery. OBES SURG 29, 2276–2286 (2019). https://doi.org/10.1007/s11695-019-03849-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03849-w