Abstract
Background and Aims
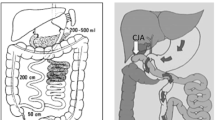
Bariatric surgeries such as gastric banding (LAGB), gastric bypass (RYGB), vertical banded gastroplasty (VBG), and sleeve gastrectomy (LSG) decrease body weight in morbid obesity, leading to the resolution of coexisting diabetes mellitus and arterial hypertension in the majority of cases as well as improvements of renal function and liver steatosis. BS (LAGB, RYGB, VBG, and LSG) also reduce incident cases of diabetes, of cardiovascular diseases, and of cancer; these therapeutic and preventive effects on comorbidities of obesity have not been analyzed for malabsorptive surgeries such as biliopancreatic diversion (BPD) or biliointestinal bypass (BIBP). The aim of this study was to analyze the incidence of comorbidities, i.e., diabetes, cardiovascular diseases, and cancer, in obese subjects undergoing BPD and BIBP, in comparison with standard medical treatment of obesity.
Patients and Methods
Medical records of 1983 obese patients (body mass index (BMI) > 35 kg/m2, aged 18–65 years, undergoing surgery (n = 472, of which 111 with diabetes) or medical treatment (n = 1511, of which 422 with diabetes), during the period 1999–2008 (visit 1)) were collected; incident cases of comorbidities were ascertained through December 31, 2016.
Results
Observation period was 12.0 ± 3.48 years (mean ± SD). Compared to non-surgical patients matched for age, body mass index, and blood pressure, malabsorptive surgeries were associated with reduced new incident cases of diabetes (p = 0.001), cardiovascular diseases (p = 0.001), hyperlipidemia (p = 0.001), oculopathy (p = 0.021), and cancer (p = 0.001). The preventive effect of BS was similar in both nondiabetic and diabetic patients for cardiovascular diseases and hyperlipidemia (both p = 0.001). The preventive effect was significant in nondiabetic subjects for coronary heart disease and for cancer, not significant in diabetic subjects.
Conclusion
Patients undergoing malabsorptive bariatric surgery show less incident cases of diabetes, cardiovascular diseases, hyperlipidemia, oculopathy, and cancer than controls receiving medical treatment.
Similar content being viewed by others
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–56.
Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65.
Ikramuddin S, Korner J, Lee WJ, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia. The Diabetes Surgery Study randomized clinical trial. JAMA. 2013;309:2240–9.
Eliasson B, Liakopoulos V, Franzén S, et al. Cardiovascular disease and mortality in patients with type 2 diabetes after bariatric surgery in Sweden: a nationwide, matched, observational cohort study. Lancet Diabetes Endocrinol. 2015;3:847–54.
Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery. An updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149:275–87.
Pontiroli AE, Zakaria AS, Mantegazza E, et al. Long-term mortality and incidence of cardiovascular diseases and type 2 diabetes in diabetic and nondiabetic obese patients undergoing gastric banding: a controlled study. Cardiovasc Diabetol. 2016;15:39.
Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377:1143–55.
Thereaux J, Lesuffleur T, Czernichow S, et al. Association between bariatric surgery and rates of continuation, discontinuation, or initiation of antidiabetes treatment 6 years later. JAMA Surg. 2018; https://doi.org/10.1001/jamasurg.2017.6163.
Benotti PN, Wood GC, Carey DJ, et al. Gastric bypass surgery produces a durable reduction in cardiovascular disease risk factors and reduces the long-term risks of congestive heart failure. J Am Heart Assoc. 2017;6:e005126.
Chang AR, Chen Y, Still C, et al. Bariatric surgery is associated with improvement in kidney outcomes. Kidney Int. 2016;90:164–71.
Folini L, Veronelli A, Benetti A, et al. Liver steatosis (LS) evaluated through chemical-shift magnetic resonance imaging liver enzymes in morbid obesity; effect of weight loss obtained with intragastric balloon gastric banding. Acta Diabetol. 2014;51:361–8.
Pontiroli AE, Morabito A. Long-term prevention of mortality in morbid obesity through bariatric surgery. A systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg. 2011;253:484–7.
Merlotti C, Morabito A, Pontiroli AE. Prevention of type 2 diabetes; a systematic review and meta-analysis of different intervention strategies. Diabetes Obes Metab. 2014;16:719–27.
Sjöström L, Peltonen M, Jacobson P, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014;311:2297–304.
Carlsson LMS, Sjöholm K, Karlsson C, et al. Long-term incidence of microvascular disease after bariatric surgery or usual care in patients with obesity, stratified by baseline glycaemic status: a post-hoc analysis of participants from the Swedish Obese Subjects study. Lancet Diabetes Endocrinol. 2017;5:271–9.
Jakobsen GS, Småstuen MC, Sandbu R, et al. Association of bariatric surgery vs medical obesity treatment with long-term medical complications and obesity-related comorbidities. JAMA. 2018;319:291–301.
Sheng B, Truong K, Spitler H, et al. The long-term effects of bariatric surgery on type 2 diabetes remission, microvascular and macrovascular complications, and mortality: a systematic review and meta-analysis. Obes Surg. 2017;27:2724–32.
Merlotti C, Ceriani V, Morabito A, et al. Bariatric surgery and diabetic retinopathy: a systematic review and meta-analysis of controlled clinical studies. Obes Rev. 2017;18:309–16.
Christou NV, Lieberman M, Sampalis F, et al. Bariatric surgery reduces cancer risk in morbidly obese patients. Surg Obes Relat Dis. 2008;46:691–5.
Sjöström L, Gummesson A, Sjöström CD, et al. Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): a prospective, controlled intervention trial. Lancet Oncol. 2009;10:653–62.
Adams TD, Stroup AM, Gress RE, et al. Cancer incidence and mortality after gastric bypass surgery. Obesity. 2009;17:796–802.
Casagrande DS, Rosa DD, Umpierre D, et al. Incidence of cancer following bariatric surgery: systematic review and meta-analysis. Obes Surg. 2014;24:1499–509.
Afshar S, Kelly SB, Seymour K, et al. The effects of bariatric surgery on colorectal cancer risk: systematic review and meta-analysis. Obes Surg. 2014;24:1793–9.
Zhou X, Yu J, Li L, et al. Effects of bariatric surgery on mortality, cardiovascular events, and cancer outcomes in obese patients: systematic review and meta-analysis. Obes Surg. 2016;26:2590–601.
Anveden Å, Taube M, Peltonen M, et al. Long-term incidence of female-specific cancer after bariatric surgery or usual care in the Swedish Obese Subjects Study. Gynecol Oncol. 2017;145:224–9.
Scopinaro N, Adami GF, Marinari GM, et al. Biliopancreatic diversion. World J Surg. 1998;22:936–46.
Eriksson F. Biliointestinal bypass. Int J Obes. 1981;5:437–47.
Doldi SB, Lattuada E, Zappa MA, et al. Biliointestinal bypass: another surgical option. Obes Surg. 1998;8:566–9.
Del Genio G, Gagner M, Limongelli P, et al. Remission of type 2 diabetes in patients undergoing biliointestinal bypass for morbid obesity: a new surgical treatment. Surg Obes Relat Dis. 2016;12:815–21.
National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Obes Res. 1998;6(Suppl 2):51S–209S.
Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–54.
www.agenziafarmaco.it, www.epicentro.iss.it/farmaci. Rapporto OSMED 2011, first published 2012. Accessed 22.06.2015.
Corrao G, Ibrahim B, Nicotra F, et al. Statins and the risk of diabetes: evidence from a large population-based cohort study. Diabetes Care. 2014;37:2225–32.
Freedman LS. Tables of the number of patients required in clinical trials using the logrank test. Stat Med. 1982;1:121–9.
Schoenfeld DA. Sample-size formula for the proportional-hazards regression model. Biometrics. 1983;39:499–503.
Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4:e297.
Boido A, Ceriani V, Cetta F, et al. Bariatric surgery and prevention of cardiovascular events and mortality in morbid obesity: mechanisms of action and choice of surgery. Nutr Metab Cardiovasc Dis. 2015;25:437–43.
Moran CP, Shanahan F. Gut microbiota and obesity: role in aetiology and potential therapeutic target. Best Pract Res Clin Gastroenterol. 2014;28:585–97.
Afshar S, Malcomson F, Kelly SB, et al. Biomarkers of colorectal cancer risk decrease 6 months after Roux-en-Y gastric bypass surgery. Obes Surg. 2018;28:945–54.
Tromba L, Tartaglia F, Carbotta S, et al. The role of sleeve gastrectomy in reducing cardiovascular risk. Obes Surg. 2017;27:1145–51.
Ceriani V, Cetta F, Lodi T, et al. Clinical and metabolic effects of biliopancreatic diversion persist after reduction of the gastric pouch and elongation of the common alimentary tract. Preliminary report in a series of patients with a 10-year follow-up. Obes Surg. 2017;27:1493–500.
Pontiroli AE, Laneri M, Veronelli A, et al. Biliary pancreatic diversion and laparoscopic adjustable gastric banding in morbid obesity: their long-term effects on metabolic syndrome and on cardiovascular parameters. Cardiovasc Diabetol. 2009;8:37.
Benetti A, Del Puppo M, Crosignani A, et al. Cholesterol metabolism after bariatric surgery in grade 3 obesity: differences between malabsorptive and restrictive procedures. Diabetes Care. 2013;36:1443–7.
Cazzo E, Pareja JC, Chaim EA, et al. Glucagon-like peptides 1 and 2 are involved in satiety modulation after modified biliopancreatic diversion: results of a pilot study. Obes Surg. 2018;28:506–12.
Adami GF, Gradaschi R, Andraghetti G, et al. Serum leptin and adiponectin concentration in type 2 diabetes patients in the short and long term following biliopancreatic diversion. Obes Surg. 2016;26(10):2442–8.
Cazzo E, Pareja JC, Geloneze B, et al. Biliopancreatic diversion decreases postprandial apolipoprotein A-IV levels in mildly obese individuals with type 2 diabetes mellitus: a prospective study. Obes Surg. 2017;27:1008–12.
Ferrannini E, Camastra S, Astiarraga B, et al. Increased bile acid synthesis and deconjugation after biliopancreatic diversion. Diabetes. 2015;64:3377–85.
Borbély YM, Osterwalder A, Kröll D, et al. Diarrhea after bariatric procedures: diagnosis and therapy. World J Gastroenterol. 2017;23:4689–700.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–36.
de la Matta-Martin M, Acosta-Martinez J, Morales-Conde S, et al. Perioperative morbi-mortality associated with bariatric surgery: from systematic biliopancreatic diversion to a tailored laparoscopic gastric bypass or sleeve gastrectomy approach. Obes Surg. 2012;22:1001–7.
Homan J, Schijns W, Aarts EO, et al. Treatment of vitamin and mineral deficiencies after biliopancreatic diversion with or without duodenal switch: a major challenge. Obes Surg. 2018;28:234–41.
Acknowledgements
The LAGB10 working group includes people from Ospedale San Paolo and Università degli Studi di Milano (Annamaria Veronelli, MD; Barbara Zecchini, BSc; Ahmed Zakaria, PhD; Francesca Frigè, BSc; Luca Rossetti, MD; Alberto Benetti, MD; Maurizio Cristina, MD; Ermanno Mantegazza, BSc; Marco Fanchini, BSc; Alberto Morabito, PhD; Franco Folli, MD; Antonio E. Pontiroli, MD); from IRCCS Policlinico (Enrico Mozzi, MD); from Ospedale San Raffaele (Alessandro Saibene, MD; Michele Paganelli, MD; Paola Vedani, MD); from Istituto Clinico Sant’Ambrogio (Giancarlo Micheletto, MD; Alessandro Giovanelli, MD); from Istituto Multimedica (Valerio Ceriani, Chiara Osio); from Ospedale Civile, Magenta (Giuliano Sarro, MD); from Istituto Humanitas Gavazzeni (Italo Nosari, MD); and from the Health Districts (Maria Grazia Angeletti, MD; Mariangela Autelitano, MD; Luca Cavalieri d’Oro, MD; Piergiorgio Berni, MD; Antonio G. Russo, MD).
The authors wish to thank Dr. Antonio G. Russo, Osservatorio Epidemiologico, ATS, Città Metropolitana di Milano, for the precious help in identifying causes of exemptions of patients in the study.
Funding
Università degli Studi di Milano, Ospedale San Paolo, Istituto Multimedica, Ospedale di Magenta, Istituto Humanitas Gavazzeni, INCO-Istituto Clinico Sant’Ambrogio. Grant “Ricerca Corrente” to Istituto Multimedica from Ministero della Salute (Ministry of Health), Italy
Author information
Authors and Affiliations
Consortia
Contributions
VC, GS, CO, GM, and AG performed all bariatric procedures, searched data, and contributed to discussion; ASZ, MF, IN, AMV, FF searched data, prepared the database, contributed to analysis, and contributed to discussion; AEP planned the research, contributed to discussion, and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The study protocol was approved by local Ethics Committees in 2015 (Coordinating Center: Ospedale San Paolo, Comitato Etico Interaziendale di Milano Area A, official approval SC: 2015 ST 125). Being a retrospective study, informed consent was obtained from all individual participants included in the study who could be reached by interview, phone, or letter.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Pontiroli, A.E., Ceriani, V., Sarro, G. et al. Incidence of Diabetes Mellitus, Cardiovascular Diseases, and Cancer in Patients Undergoing Malabsorptive Surgery (Biliopancreatic Diversion and Biliointestinal Bypass) vs Medical Treatment. OBES SURG 29, 935–942 (2019). https://doi.org/10.1007/s11695-018-3601-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3601-5