Abstract
Introduction
Metabolic surgery is known to impact glucose tolerance but the exact mechanism is still unclear. Based on recently-published data, especially the role of the hindgut may require redefinition.
Methods
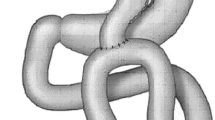
Either a loop duodeno-jejunostomy (DJOS) with exclusion of one third of total intestinal length, a loop duodeno-ileostomy (DiOS, exclusion of two thirds), or SHAM operation was performed in 9-week-old Zucker diabetic fatty rats. One, 3, and 6 months after surgery, an oral glucose tolerance test (OGTT) and glucose-stimulated hormone analyses were conducted. Body weight was documented weekly.
Results
DJOS and DiOS animals showed significantly better glucose control in all OGTTs than the SHAM group (two-way ANOVA p < 0.0001). Body weight developed largely parallel in both intervention groups; SHAM animals had gained significantly less weight after 6 months (Mann-Whitney DJOS/DiOS vs. SHAM p < 0.05, DJOS vs. DiOS p > 0.05). Operative interventions had no impact on GLP-1 and GIP levels at any time point (Mann-Whitney p > 0.05 for all). DJOS/DiOS operations could preserve insulin production up to 6 months, while there was already a sharp decline of insulin levels in the SHAM group (Mann-Whitney: DJOS/DiOS vs. SHAM p < 0.05 for all time points). Additionally, insulin sensitivity was improved significantly 1 month postoperative in both intervention groups compared to SHAM (Mann-Whitney DJOS/DiOS vs. SHAM p < 0.05).
Conclusion
The data of the current study demonstrate a sharp amelioration of glucose control after duodenal exclusion with unchanged levels of GLP-1 and GIP. Direct or delayed hindgut stimulation had no impact on glucose control in our model.






Similar content being viewed by others
References
WHO | Obesity and overweight [Internet]. WHO. [cited 2016 Apr 19]. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/
WHO | Diabetes [Internet]. WHO. [cited 2016 Apr 19]. Available from: http://www.who.int/mediacentre/factsheets/fs312/en/
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442.
Ribaric G, Buchwald JN, McGlennon TW. Diabetes and weight in comparative studies of bariatric surgery vs conventional medical therapy: a systematic review and meta-analysis. Obes Surg. 2014;24(3):437–55.
Maggard-Gibbons M, Maglione M, Livhits M, et al. Bariatric surgery for weight loss and glycemic control in nonmorbidly obese adults with diabetes: a systematic review. JAMA. 2013;309(21):2250.
Lee W-J, Hur KY, Lakadawala M, et al. Gastrointestinal metabolic surgery for the treatment of diabetic patients: a multi-institutional international study. J Gastrointest Surg. 2012;16(1):45–52.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2012;55(6):1577–96.
DePaula AL, Macedo ALV, Schraibman V, et al. Hormonal evaluation following laparoscopic treatment of type 2 diabetes mellitus patients with BMI 20–34. Surg Endosc. 2009;23(8):1724–32.
Horwitz D, Saunders JK, Ude-Welcome A, Marie Schmidt A, Dunn V, Leon Pachter H, et al. Three-year follow-up comparing metabolic surgery versus medical weight management in patients with type 2 diabetes and BMI 30–35. The role of sRAGE biomarker as predictor of satisfactory outcomes. Surg Obes Relat Dis [Internet]. 2016 Jan [cited 2016 May 9]; Available from: http://linkinghub.elsevier.com/retrieve/pii/S1550728916000216
Scopinaro N, Camerini G, Papadia F, Andraghetti G, Cordera R, Adami GF. Long-term clinical and functional impact of biliopancreatic diversion on type 2 diabetes in morbidly and non–morbidly obese patients. Surg Obes Relat Dis [Internet]. 2015; Available from: http://linkinghub.elsevier.com/retrieve/pii/S1550728915011016
The American Diabetes Association’s “Standards of Medical Care in Diabetes.” Diabetes Care. 2015;38(Supplement_1):S1–2.
Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222(3):339–52.
Cummings DE, Cohen RV. Bariatric/metabolic surgery to treat type 2 diabetes in patients with a BMI & lt; 35 kg/m 2. Diabetes Care. 2016;39(6):924–33.
Schauer PR, Mingrone G, Ikramuddin S, et al. Clinical outcomes of metabolic surgery: efficacy of glycemic control, weight loss, and remission of diabetes. Diabetes Care. 2016;39(6):902–11.
Nauck MA. Unraveling the science of incretin biology. Am J Med. 2009;122(6):S3–10.
Rubino F, Gagner M. Potential of surgery for curing type 2 diabetes mellitus. Ann Surg. 2002;236(5):554–9.
Reimann F. Molecular mechanisms underlying nutrient detection by incretin-secreting cells. Int Dairy J. 2010;20(4):236–42.
Drucker DJ. The biology of incretin hormones. Cell Metab. 2006;3(3):153–65.
Rubino F, Gagner M, Gentileschi P, et al. The early effect of the Roux-en-Y gastric bypass on hormones involved in body weight regulation and glucose metabolism. Ann Surg. 2004;240(2):236–42.
Rubino F, Forgione A, Cummings DE, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006;244(5):741–9.
Li P, Zhu L, Wang G, Yang X, Yi B, Zhu S. The role of foregut exclusion in the deterioration of glucose and lipid metabolism induced by a high-fat diet. Diabetes Res Clin Pract [Internet]. 2016 Jan [cited 2016 Apr 19]; Available from: http://linkinghub.elsevier.com/retrieve/pii/S0168822716000589
Chai J, Zhang G, Liu S, et al. Exclusion of the distal ileum cannot reverse the anti-diabetic effects of duodenal-jejunal bypass surgery. Obes Surg. 2016;26(2):261–8.
Ren Z-Q, Zhang P-B, Zhang X-Z, et al. Duodenal-jejunal exclusion improves insulin resistance in type 2 diabetic rats by upregulating the hepatic insulin signaling pathway. Nutrition. 2015;31(5):733–9.
Castagneto M, Mingrone G. The effect of gastrointestinal surgery on insulin resistance and insulin secretion. Curr Atheroscler Rep. 2012;14(6):624–30.
Hedberg J, Sundström J, Sundbom M. Duodenal switch versus Roux-en-Y gastric bypass for morbid obesity: systematic review and meta-analysis of weight results, diabetes resolution and early complications in single-centre comparisons. Obes Rev. 2014;15(7):555–63.
Currò G, Centorrino T, Cogliandolo A, et al. A clinical and nutritional comparison of biliopancreatic diversion performed with different common and alimentary channel lengths. Obes Surg. 2015;25(1):45–9.
De Luca M, Angrisani L, Himpens J, et al. Indications for surgery for obesity and weight-related diseases: position statements from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). Obes Surg. 2016;26(8):1659–96.
Sánchez-Pernaute A, Herrera MAR, Pérez-Aguirre ME, et al. Single anastomosis duodeno–ileal bypass with sleeve gastrectomy (SADI-S). One to Three-Year Follow-up Obes Surg. 2010;20(12):1720–6.
Marjanovic G, Holzner P, Kulemann B, et al. Pitfalls and technical aspects during the research of intestinal anastomotic healing in rats. Eur Surg Res. 2010;45(3–4):314–20.
Karcz WK, Kuesters S, Marjanovic G, et al. Duodeno-enteral omega switches—more physiological techniques in metabolic surgery. Videosurgery Miniinvasive Tech. 2013;4:273–9.
Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Katz A, Nambi SS, Mather K, et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000;85(7):2402–10.
Pacheco D, de Luis DA, Romero A, et al. The effects of duodenal-jejunal exclusion on hormonal regulation of glucose metabolism in Goto-Kakizaki rats. Am J Surg. 2007;194(2):221–4.
Rubino F, Marescaux J. Effect of duodenal-jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg. 2004;239(1):1–11.
Kindel TL, Yoder SM, Seeley RJ, et al. Duodenal-jejunal exclusion improves glucose tolerance in the diabetic, Goto-Kakizaki rat by a GLP-1 receptor-mediated mechanism. J Gastrointest Surg. 2009;13(10):1762–72.
Chambers AP, Jessen L, Ryan KK, et al. Wilson–Pérez HE, Stefater MA, et al. weight-independent changes in blood glucose homeostasis after gastric bypass or vertical sleeve gastrectomy in rats. Gastroenterology. 2011;141(3):950–8.
Abegg K, Corteville C, Docherty NG, et al. Effect of bariatric surgery combined with medical therapy versus intensive medical therapy or calorie restriction and weight loss on glycemic control in Zucker diabetic fatty rats. Am J Physiol - Regul Integr Comp Physiol. 2015;308(4):R321–9.
Grueneberger JM, Karcz-Socha I, Sawczyn T, et al. Systematic ileal transposition in Zucker rats shows advantage for long segment distal transposition. Surgery. 2014;155(1):165–72.
Brethauer SA, Aminian A, Romero-Talamás H, Batayyah E, Mackey J, Kennedy L, et al. Can diabetes be surgically cured? Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus: Ann Surg. 2013:1.
Shimabukuro M, Zhou Y-T, Levi M, et al. Fatty acid-induced β cell apoptosis: a link between obesity and diabetes. Proc Natl Acad Sci. 1998;95(5):2498–502.
Insulin Values for Obese Male ZDF Rats Fed IR Purina 5008 (Portage, MI and Kingston, NY - September 2005) [Internet]. Available from: http://www.criver.com/files/pdfs/rms/zdf/rm_rm_r_zdf_rat_insulin_levels_sept05.aspx.
Weight chart for obese male ZDf rats fed IR Purina 5008 (Portage, MI and Kingstone, NY-September 2005)[Internet]. Available from: http://www.criver.com/files/pdfs/rms/zdf/rm_rm_r_zdf_rat_weight_chart_sept05.aspx.
Gumbs AA, Modlin IM, Ballantyne GH. Changes in insulin resistance following bariatric surgery: role of caloric restriction and weight loss. Obes Surg. 2005;15(4):462–73.
Liu Y, Zhou Y, Wang Y, et al. Roux-en-Y gastric bypass-induced improvement of glucose tolerance and insulin resistance in type 2 diabetic rats are mediated by glucagon-like peptide-1. Obes Surg. 2011;21(9):1424–31.
Salinari S, le Roux CW, Bertuzzi A, et al. Duodenal-jejunal bypass and jejunectomy improve insulin sensitivity in Goto-Kakizaki diabetic rats without changes in incretins or insulin secretion. Diabetes. 2014;63(3):1069–78.
Zhou X, Qian B, Ji N, Lui C, Liu Z, Li B, et al. Pancreatic hyperplasia after gastric bypass surgery in a GK rat model of non-obese type 2 diabetes. J Endocrinol. 2016;228:13–23.
Speck M, Cho YM, Asadi A, et al. Duodenal-jejunal bypass protects GK rats from -cell loss and aggravation of hyperglycemia and increases enteroendocrine cells coexpressing GIP and GLP-1. AJP Endocrinol Metab. 2011;300(5):E923–32.
Kindel TL, Yoder SM, D’Alessio DA, et al. The effect of duodenal–jejunal bypass on glucose-dependent insulinotropic polypeptide secretion in Wistar rats. Obes Surg. 2010;20(6):768–75.
Mingrone G, Castagneto-Gissey L. Mechanisms of early improvement/resolution of type 2 diabetes after bariatric surgery. Diabetes Metab. 2009;35(6):518–23.
Zander M, Madsbad S, Madsen JL, et al. Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and β-cell function in type 2 diabetes: a parallel-group study. Lancet. 2002;359(9309):824–30.
Perfetti R, Hui H. The role of GLP-1 in the life and death of pancreatic beta cells. Horm Metab Res. 2004;36(11/12):804–10.
Buchwald H, Menchaca HJ, Michalek VN, et al. Ileal effect on blood glucose, HbA1c, and GLP-1 in Goto-Kakizaki rats. Obes Surg. 2014;24(11):1954–60.
Seyfried F, Bueter M, Spliethoff K, et al. Roux-en Y gastric bypass is superior to duodeno-jejunal bypass in improving glycaemic control in Zucker diabetic fatty rats. Obes Surg. 2014;24(11):1888–95.
Flynn CR, Albaugh VL, Cai S, et al. Bile diversion to the distal small intestine has comparable metabolic benefits to bariatric surgery. Nat Commun. 2015;6:7715.
Kohli R, Setchell KD, Kirby M, et al. A surgical model in male obese rats uncovers protective effects of bile acids post-bariatric surgery. Endocrinology. 2013;154(7):2341–51.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Topart P, Becouarn G, Delarue J. Weight loss and nutritional outcomes 10 years after biliopancreatic diversion with duodenal switch. Obes Surg [Internet]. 2017 Jan 4 [cited 2017 Jan 14]; Available from: http://link.springer.com/10.1007/s11695-016-2537-x
Hedberg J, Sundbom M. superior Weight loss and lower HbA1c 3 years after duodenal switch compared with Roux-en-Y gastric bypass—a randomized controlled trial. Surg Obes Relat Dis 2012;8(3):338–343.
Acknowledgments
The authors thank Silke Hempel for the outstanding work in assistance with ELISA measurements. Also, we thank Dieter Hauschke for his advice in statistical questions. Moreover, we thank Claudia Bravo and Monika Kolterjahn for the excellent work with animal care.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All animal experimental protocols were approved by the local Animal Welfare Committee under the auspices of the responsible regional commission. All applicable institutional and national guidelines for the care and use of animals were followed.
Grant Information
None.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Laessle, C., Michelmichel, S., Marjanovic, G. et al. Common Channel Length in Bypass Surgery Does Not Impact T2DM in Diabetic Zucker Rats. OBES SURG 27, 2090–2098 (2017). https://doi.org/10.1007/s11695-017-2611-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2611-z