Abstract
Summary
Vitamin D intake over the recommended dose is usually associated with high serum 25(OH)D levels and generally not associated with symptoms of hypercalcemia. High doses of cholecalciferol need to be avoided to protect against vitamin D toxicity and related complications. Strict adherence to the clinical guidelines for treating vitamin D deficiency can ensure safe and effective treatment.
Purpose
We observed a tendency to use high doses of cholecalciferol for vitamin D deficiency treatment or vitamin D supplementation. We aimed to determine the biochemical characteristics of patients with high normal and elevated serum 25(OH)D levels.
Methods
An online invitation was sent to all tertiary endocrinology clinics in Turkey to complete an online retrospective survey (DeVIT-TOX Survey) for patients diagnosed with high serum 25(OH)D levels (> 88 ng/mL) between January 2019 and December 2019. The patients were evaluated according to the presence of signs and symptoms of hypercalcemia and doses of vitamin D intake, evaluated into the following three groups according to their 25(OH)D levels: group 1, > 150 ng/mL; group 2, 149–100 ng/mL; and group 3, 99–88 ng/mL.
Results
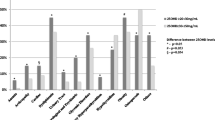
A total of 253 patients were included in the final analysis (female/male: 215/38; mean age, 51.5 ± 15.6 years). The average serum 25(OH)D level was 119.9 ± 33 (range, 88–455) ng/mL, and the average serum calcium level was 9.8 ± 0.7 (range, 8.1–13.1) mg/dL. Most (n = 201; 75.4%) patients were asymptomatic despite having high serum 25(OH)D and calcium levels. The serum 25(OH)D level was significantly higher in the symptomatic groups than in the asymptomatic groups (138.6 ± 64 ng/mL vs. 117.7 ± 31 ng/mL, p < 0.05). The most common cause (73.5%) associated with high serum 25(OH)D levels was the inappropriate prescription of a high dose of oral vitamin D (600.000–1.500.000 IU) for treating vitamin D deficiency/insufficiency in a short time (1–3 months). The cut-off value of 25 (OH) D level in patients with hypercalcemia was found to be 89 ng/mL [median 116.5 (89–216)].
Conclusions
High dose of vitamin D intake is associated with a high serum 25 OH D level, without symptoms of hypercalcemia. Inappropriate prescription of vitamin D is the primary cause for elevated 25(OH) D levels and related hypercalcemia. Hypercalcemia may not be observed in every patient at very high 25(OH) D levels. Adherence to the recommendation of guidelines is essential to ensure safe and effective treatment of vitamin D deficiency.



Similar content being viewed by others
Data availability
The datasets generated for this study are available on request to the corresponding author.
References
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP et al (2011) Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930. https://doi.org/10.1210/jc.2011-0385
Matsui MS (2020) Vitamin D update. Curr Derm Rep 9:323–330. https://doi.org/10.1007/s13671-020-00315-0
Berridge MJ (2017) Vitamin D deficiency and diabetes. Biochem J 474:1321–1332. https://doi.org/10.1042/BCJ20170042
Sassi F, Tamone C, D’Amelio P (2018) Vitamin D: nutrient, hormone, and immunomodulator. Nutrients 10(11):1656. https://doi.org/10.3390/nu10111656
Alfredsson L, Armstrong BK, Butterfield DA, Chowdhury R, de Gruijl FR, Feelisch M, … Young AR (2020) Insufficient sun exposure has become a real public health problem. Int J Environ Res Public Health 17(14):5014.https://doi.org/10.3390/ijerph17145014
Mirhosseini N, Rainsbury J, Kimball SM (2018) Vitamin D supplementation, serum 25(OH)D concentrations and cardiovascular disease risk factors: a systematic review and meta-analysis. Front Cardiovasc Med 12(5):87. https://doi.org/10.3389/fcvm.2018.00087
Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B et al (2019) Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr Rev 40:1109–1151. https://doi.org/10.1210/er.2018-00126
Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S et al (2019) Vitamin D supplements and prevention of cancer and cardiovascular disease. N Engl J Med 380:33–44
Lips P, Bilezikian JP, Bouillon R (2019) Vitamin D: giveth to those who needeth. JBMR Plus 4(1):e10232. https://doi.org/10.1002/jbm4.10232
Holick MF (2017) The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord 18(2):153–165. https://doi.org/10.1007/s11154-017-9424-1
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281. https://doi.org/10.1056/NEJMra070553
Pludowski P, Holick MF, Grant WB, Konstantynowicz J, Mascarenhas MR, Haq A et al (2018) Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol 175:125–135. https://doi.org/10.1016/j.jsbmb.2017.01.021
Jorde R, Sollid ST, Svartberg J, Schirmer H, Joakimsen RM, Njolstad I et al (2016) Vitamin D 20,000 IU per week for five years does not prevent progression from prediabetes to diabetes. J Clin Endocrinol Metab 101:1647–1655. https://doi.org/10.1210/jc.2015-4013
Scragg R, Khaw KT, Toop L, Sluyter J, Lawes CMM, Waayer D et al (2018) Monthly high-dose vitamin D supplementation and cancer risk: a post hoc analysis of the vitamin D assessment randomized clinical trial. JAMA Oncol 4(11):e182178. https://doi.org/10.1001/jamaoncol.2018.2178
Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ, Staehelin HB, Meyer OW, Theiler R et al (2016) Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern Med 176(2):175–183. https://doi.org/10.1001/jamainternmed.2015.7148
Khaw KT, Stewart AW, Waayer D, Lawes CMM, Toop L, Camargo CA Jr et al (2017) Effect of monthly high-dose vitamin D supplementation on falls and non-vertebral fractures: secondary and post-hoc outcomes from the randomised, double-blind, placebo-controlled ViDA trial. Lancet Diabetes Endocrinol 5(6):438–447. https://doi.org/10.1016/S2213-8587(17)30103-1
Pludowski P, Grant WB, Konstantynowicz J, Holick MF (2019) Editorial: classic and pleiotropic actions of vitamin D. Front Endocrinol (Lausanne) 10:341. https://doi.org/10.3389/fendo.2019.00341
Marcinowska-Suchowierska E, Kupisz-Urbańska M, Łukaszkiewicz J, Płudowski P, Jones G (2018) Vitamin D toxicity-a clinical perspective. Front Endocrinol (Lausanne) 9:550. https://doi.org/10.3389/fendo.2018.00550
Ozkan B, Hatun S, Bereket A (2012) Vitamin D intoxication. Turk J Pediatr 54:93–98
Taylor PN, Davies JS (2018) A review of the growing risk of vitamin D toxicity from inappropriate practice. Br J Clin Pharmacol 84:1121–1127. https://doi.org/10.1111/bcp.13573
Varimli D (2021) Ülkemizde D Vitamini Reçetelemesinin ve Tüketiminin Değerlendirilmesi. Thesis, Haceetepe University, Ankara, Turkey
Płudowski P, Karczmarewicz E, Bayer M, Carter G, Chlebna-Sokół D, Czech-Kowalska J et al (2013) Practical guidelines for the supplementation of vitamin D and the treatment of deficits in Central Europe - recommended vitamin D intakes in the general population and groups at risk of vitamin D deficiency. Endokrynol Pol 64(4):319–327. https://doi.org/10.5603/ep.2013.0012
Kucukerdem HS, Arslan M, Koc EM, Can H (2017) Retrospective evaluation of family medicine outpatient clinic profile at a tertiary hospital in İzmir. J Acad Res Med 7(3):112–116. https://doi.org/10.5152/jarem.2017.1165
Al-Yatama FI, AlOtaibi F, Al-Bader MD, Al-Shoumer KA (2019) The effect of clothing on vitamin d status, bone turnover markers, and bone mineral density in young Kuwaiti females. Int J Endocrinol 2019:6794837. https://doi.org/10.1155/2019/6794837
Buyukuslu N, Esin K, Hizli H, Sunal N, Yigit P, Garipagaoglu M (2014) Clothing preference affects vitamin D status of young women. Nutr Res 34(8):688–693. https://doi.org/10.1016/j.nutres.2014.07.012
Bassil D, Rahme M, Hoteit M, Fuleihan Gel-H (2013) Hypovitaminosis D in the Middle East and North Africa: prevalence, risk factors and impact on outcomes. Dermatoendocrinol. 5(2):274–298. https://doi.org/10.4161/derm.25111
Lips P, Cashman KD, Lamberg-Allardt C, Bischoff-Ferrari HA, Obermayer-Pietsch B, Bianchi ML, … Bouillon R (2019) Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society. Eur J Endocrinol 180(4):P23–P54.https://doi.org/10.1530/eje-18-0736
Galior K, Grebe S, Singh R (2018) Development of vitamin D toxicity from overcorrection of vitamin D deficiency: a review of case reports. Nutrients 10(8):953. https://doi.org/10.3390/nu10080953
Amrein K, Sourij H, Wagner G, Holl A, Pieber TR, Smolle KH et al (2011) Short-term effects of high-dose oral vitamin D3 in critically ill vitamin D deficient patients: a randomized, double-blind, placebo-controlled pilot study. Crit Care 15(2):R104. https://doi.org/10.1186/cc10120
Balk EM, Adam GP, Langberg VN, Earley A, Clark P, Ebeling PR et al (2017) Global dietary calcium intake among adults: a systematic review. Osteoporos Int 28:3315–3324. https://doi.org/10.1007/s00198-017-4230-x
Ersoy B, Kizilay DÖ, Yilmaz SK, Taneli F, Gümüşer G (2018) Bone mineral density, vitamin D status, and calcium intake in healthy female university students from different socioeconomic groups in Turkey. Arch Osteoporos 13:135. https://doi.org/10.1007/s11657-018-0482-0
Kaur P, Mishra SK, Mithal A (2015) Vitamin D toxicity resulting from overzealous correction of vitamin D deficiency. Clin Endocrinol (Oxf) 83:327–331. https://doi.org/10.1111/cen.12836
Acknowledgements
Preparation for publication of this article is supported by the Society of Endocrinology and Metabolism of Turkey.
Author information
Authors and Affiliations
Contributions
DGY conceived and designed the study. DGY, ZP, and ESS analyzed and interpreted the data. DGY, ZP, and ESS drafted and revised the manuscript. All authors have contributed to the work and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
Written informed consent was obtained from all patients based on the Declaration of Helsinki. The study was approved by the Ethics Committee of Marmara University School of Medicine.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pekkolay, Z., Yavuz, D.G., Saygılı, E.S. et al. Biochemical characteristics and calcium and PTH levels of patients with high normal and elevated serum 25(OH)D levels in Turkey: DeVIT-TOX survey. Arch Osteoporos 16, 138 (2021). https://doi.org/10.1007/s11657-021-01002-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-021-01002-8