Abstract
Background
Although previous research has demonstrated high rates of inappropriate diagnostic imaging, the potential influence of several physician-level characteristics is not well established.
Objective
To examine the influence of three types of physician characteristics on inappropriate imaging: experience, specialty training, and self-referral.
Design
A retrospective analysis of over 70,000 MRI claims submitted for commercially insured individuals. Physician characteristics were identified through a combination of administrative records and primary data collection. Multi-level modeling was used to assess relationships between physician characteristics and inappropriate MRIs.
Setting
Massachusetts
Participants
Commercially insured individuals who received an MRI between 2010 and 2013 for one of three conditions: low back pain, knee pain, and shoulder pain.
Measurements
Guidelines from the American College of Radiology were used to classify MRI referrals as appropriate/inappropriate. Experience was measured from the date of medical school graduation. Specialty training comprised three principal groups: general internal medicine, family medicine, and orthopedics. Two forms of self-referral were examined: (a) the same physician who ordered the procedure also performed it, and (b) the physicians who ordered and performed the procedure were members of the same group practice and the procedure was performed outside the hospital setting.
Results
Approximately 23% of claims were classified as inappropriate. Physicians with 10 or less years of experience had significantly higher odds of ordering inappropriate MRIs. Primary care physicians were almost twice as likely to order an inappropriate MRI as orthopedists. Self-referral was not associated with higher rates of inappropriate MRIs.
Limitations
Classification of MRIs was conducted with claims data. Not all self-referred MRIs could be detected.
Conclusions
Inappropriate imaging continues to be a driver of wasteful health care spending. Both physician experience and specialty training were highly associated with inappropriate imaging.
Similar content being viewed by others
INTRODUCTION
Diagnostic imaging now accounts for more than $100 billion of US health care spending annually.1,2 At the same time, there is much evidence that a substantial percentage of imaging procedures are inappropriate because the procedure was not indicated clinically. Prior studies point to rates of inappropriate imaging in excess of 20% for musculoskeletal conditions and prostate cancer.3,4,5,6
However, relatively little research has examined determinants of inappropriate imaging. In this paper, we report results from a study of inappropriate imaging with MRI relative to several characteristics of ordering physicians—experience, specialty training, and self-referral. For each of these characteristics, there has been speculation, but relatively little firm evidence, regarding their actual influence on inappropriate imaging. Thus, while previous research has found that less experienced physicians order relatively more diagnostic tests,7,8,9 whether this translates into more inappropriate imaging has not been well established. Similarly, physician specialty has been linked to higher rates of service utilization10 and some small-scale investigations suggest that physicians are less likely to order inappropriate imaging for clinical conditions in which they specialize.11,12 Regarding self-referral imaging, which is generally defined as physicians referring patients for imaging to facilities in which they or their partners have financial interests,13 this type of arrangement has been linked to higher rates of imaging utilization13,14,15,16,17,18 and also higher frequencies of negative findings from imaging studies.19,20 However, little current research has examined the central question of whether self-referral is, in fact, associated with a higher likelihood of inappropriate imaging.
METHODS
Data and Study Sample
The primary data source was the Massachusetts All-Payer Claims Database (APCD) from which we obtained all commercial health insurance claims for the years 2009 through 2013, including those claims paid as part of a Medicare supplemental health insurance policy and Medicare Advantage plans.
Physician data were obtained from several sources. One was the Massachusetts Board of Registration in Medicine, which provided information regarding a physician’s education and training programs including graduation dates, hospital affiliations, and practice location. Physician identifiers were available in the form of National Provider Identifiers (NPI). Additional data on physicians’ practice group affiliation came from health plans. We obtained from several large health plans in Massachusetts the names and practice locations of physicians who were members of their plan networks. We used these data sources along with Internet searches and phone calls to map physicians to practices for obtaining details about their practice setting including location and number of physician members.
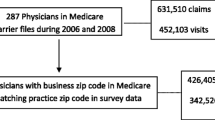
For the study sample, we focused on imaging procedures for three common clinical conditions: uncomplicated lower back pain, non-traumatic knee pain, and non-traumatic shoulder pain. We chose these conditions because they are prevalent among adults in the US, guidelines exist as to when imaging is appropriate, and the associated imaging procedures are routinely performed at a variety of clinical settings.21,22,23 Figure 1 provides the relevant ICD-9 codes for the selected three clinical conditions and also exclusion criteria for the sample that included any one of 19 chronic conditions listed by the Centers for Medicare and Medicaid Services.24 The remaining imaging claims (n = 71,694) provided the sample of patients for the study.
Variables and Measures
In line with previous research, we defined the outcome variable as whether an imaging procedure (i.e., MRI) was appropriate/inappropriate.25 To classify imaging procedures as inappropriate, we applied diagnostic imaging guidelines developed by the American College of Radiology (ACR).26,27,28,29 For uncomplicated lower back pain, the ACR guideline recommends against imaging (both X-ray and MRI) unless certain clinical factors are present including “red flag” indications (e.g., cancer) and prior medical management. This is consistent with another guideline for lower back pain issued jointly by the American College of Physicians (ACP) and the American Pain Society (APS).30 For shoulder pain without trauma, the ACR guideline recommends a routine X-ray as the first choice for imaging with shoulder MRI indicated if the X-ray results are inconclusive or pain is persistent. For knee pain without trauma, the ACR guideline also recommends X-ray as the first choice for imaging with knee MRI indicated when the X-ray results are inconclusive or indicate a joint effusion.
Our classification of imaging claims as inappropriate/appropriate entailed two key steps (see Fig. 1). First, for each patient for which an imaging claim was submitted between 2010 and 2013 (identified by CPT code for global or professional component), we searched the claims database for a preceding office visit that constituted the point at which the imaging referral was made as indicated by a referral code. We also searched for any prior claims for office visits and/or physical therapy sessions that were submitted within 12 months of this office visit to flag patients who may have had previous medical management for the relevant clinical condition. Previous office visits alone suggest a patient had sought care for the condition and may be on a treatment plan even in the absence of billed physical therapy. For claims occurring in 2010, we were able to search for prior evidence of medical management with data from 2009.
Second, we determined whether each imaging claim occurred within a time frame from the focal office visit such that it would be unlikely that the patient could have underwent some level of meaningful conservative treatment (i.e., unbilled therapy or home exercise) before the imaging procedure was performed. Clinical opinion varies as to the duration of such conservative treatment but typically falls in the range of 4 to 8 weeks.31,32 Accordingly, we classified an MRI for uncomplicated lower back pain as inappropriate if the procedure occurred within a 30-day window and there was no evidence of prior office visits or billed physical therapy sessions. We classified MRI imaging for non-traumatic knee or shoulder pain as inappropriate if the procedure occurred within a 30-day window without evidence of a previous X-ray, office visit, or physical therapy claim. We also conducted sensitivity analyses by expanding the window up to 60 days.
The key independent variables for physician characteristics were experience, specialty training, and self-referral arrangement. For physician experience, we subtracted the medical school graduation year of the referring physician for each claim from the year of submission for that claim. Physicians were grouped into four categories beginning with 10 years or less and ending with more than 35 years. Physicians were classified by specialty as primary care (i.e., internal medicine, family medicine), orthopedics, and other (i.e., small group comprised largely of neurologists and surgeons). In the case of musculoskeletal conditions, orthopedists would likely have more specialized knowledge compared with other specialists and possibly greater awareness of related imaging guidelines. Although many patients see a primary care physician for such conditions before being referred to an orthopedist, this is not always the case particularly for those enrolled in Preferred Provider Organization (PPO) plans where primary care referrals are typically not required.
We identified self-referred imaging from patterns in the imaging claims including the medical specialty and practice affiliations of the physicians submitting the claims.13,33 We identified two primary forms of self-referral arrangements. One was when the same non-radiologist physician who ordered the procedure also performed it. A second form entailed self-referral based on the presence of three criteria: (a) the physician who ordered the imaging procedure and the physician who performed it were members of the same group practice (as indicated by practice name, location, and tax ID), (b) the physician who performed the imaging procedure had billed for imaging services at least three times during the last 12 months, and (c) the imaging procedure was performed outside the hospital setting (i.e., office setting or imaging center). We excluded from this second form of self-referral arrangement claims that were submitted from large practices (i.e., over 50 physicians) on the basis that financial incentives to member physicians for imaging are likely to be diluted in such settings given the size of the practice and thus not likely to influence behavior.
Our analysis included control variables to account for potentially confounding patient characteristics. We assigned patients to one of several types of health plans (i.e., Health Maintenance Organization (HMO), PPO, indemnity). HMO plans often feature pre-authorization requirements and related controls for expensive clinical services that some studies suggest influence utilization for imaging services.34,35 For median household income, a proxy for a patient’s financial resources for covering deductibles and co-pays connected with imaging procedures, we grouped patients by quartiles. For geographic location, we grouped patients based on whether their residence was located in the northeast, southeast, central, or western regions of the state as this may account for some differences in the availability of imaging technology. MRIs per person have long been higher in the northeast region particularly compared with those in the western region. In addition, we accounted for whether the ordering physician had an affiliation with a teaching hospital as participation in a teaching environment might offer enhanced exposure to imaging guidelines and related clinical resources. The model also included indicator variables for the year in which the claim was submitted.
Statistical Analysis
We conducted bivariate analyses using chi-square tests for both global and specific comparisons regarding the physician characteristics of interest. For multivariate analyses, we estimated a logistic regression model for inappropriate MRI claims performed from 2010 to 2013. We utilized a generalized linear mixed model with fixed effects for physician practices and random effects to account for the nesting of patients by ordering physician.36 To determine the amount of variation attributable to ordering physicians, we re-estimated the model without fixed effects and computed the intraclass correlation coefficients (ICC) for the physician and physician practice levels.37,38,39
RESULTS
Table 1 presents characteristics of the physicians and patients included in the study. Of the 71,694 claims that comprised the study sample, 23.3% were classified as inappropriate. There were 8,297 physicians who ordered at least one MRI for which we had an insurance claim.
Table 2 presents results for the bivariate analyses. The global tests were statistically significant for experience (χ2 = 196.8; p < 0.001) and specialty training (χ2 = 279.9; p < 0.001). The specific comparisons show that physicians in the least experienced group had higher rates of inappropriate imaging compared with physicians in the reference group (i.e., more than 10 to 25 years of experience). A higher rate was also observed for physicians with more than 35 years of experience. For specialty training, both groups of primary care physicians (i.e., internists and family physicians) as well as those physicians comprising “other specialties” had higher rates of inappropriate imaging relative to orthopedists.
Table 3 presents results from the multi-level regression model. These results are generally consistent with those from the bivariate analyses. Physicians with 10 years or less experience had greater odds (1.75; 95%CI 1.51–2.02) of ordering an inappropriate MRI than the comparison group (i.e., > 10 to 25 years of experience). In comparison with orthopedists, physicians from each of the two primary care specialties (i.e., internal medicine and family medicine) had significantly higher odds of ordering an inappropriate MRI with odds ratios that exceeded 1.80. Physicians from the group of “other specialties” also had significantly higher odds of ordering inappropriate MRIs than did orthopedists (1.73; 95%CI 1.48–2.00). Neither form of self-referral was statistically significant. To further assess effects for self-referral, we re-estimated the model with both forms of self-referral combined. This combined variable was also not statistically significant. We also re-estimated the model to test for interaction effects among the selected physician characteristics, but the results were not statistically significant. Expanding the window from 30 to 60 days did not have any material impact on the results already reported. After re-estimating the model without fixed effects to compute ICC values, physicians and physician practices accounted for 19.1% and 15.3% of the variance, respectively. Regarding control variables, patients who were enrolled in either PPO or indemnity plans, resided in the western region of Massachusetts, and presented with lower back pain had relatively higher rates of inappropriate imaging.
DISCUSSION
Our analysis indicated that approximately 23% of the MRIs ordered for the selected conditions were inappropriate, which while largely consistent with previous research points to a serious and ongoing lack of adherence to imaging guidelines. A strong association existed between two of the three selected physician characteristics and inappropriate diagnostic imaging. Less experienced physicians had substantially higher rates of inappropriate imaging. One explanation for this finding is that physicians at the beginning of their careers are less aware of imaging guidelines. Prior research has reported a low level of incorporation of ACR imaging guidelines in physician training programs.40,41,42 One study that evaluated the impact of providing residents with training on imaging guidelines did report decreased utilization of abdominal imaging though the impact on inappropriate imaging was not assessed.43 A coordinated campaign among medical societies and teaching hospitals to increase awareness of imaging guidelines among physicians in training programs is likely a worthwhile undertaking. An additional consideration is that physicians at the beginning of their careers may engage in excessive imaging as a form of defensive medicine due to heightened concerns about malpractice liability. Defensive medicine has long been considered a key driver of excessive imaging.9 In this vein, physicians must have confidence that adherence to imaging guidelines protects them from malpractice liability.
We also found specialty training to be a relevant factor for inappropriate imaging. Primary care physicians were nearly twice as likely to order inappropriate MRIs as were orthopedists. These results are consistent with some prior but smaller scale investigations including a study of Canadian physicians that was conducted with medical records.11 Primary care physicians see a wide range of clinical conditions for the patients they treat and undoubtedly face substantial challenges in following all relevant guidelines. Initiatives such as the Choosing Wisely web-based tool and computerized radiology order entry systems are intended to facilitate physicians’ access to imaging guidelines,44,45 but their impact on inappropriate imaging has yet to be closely studied. Another relevant development is that CMS is phasing in a new rule that requires physicians participating in the Medicare program to document they are following appropriate use criteria for outpatient diagnostic imaging using clinical decision support software.46 The impact of this requirement will be important to assess.
For self-referral, study results stand perhaps somewhat in contrast to previous research linking self-referral to higher utilization of imaging procedures. Physicians in favor of self-referral have long contended that such arrangements offer greater continuity of care and convenience for patients that reduce delays for imaging.33 From this perspective, the fact that self-referral is associated with increased utilization is indicative of better access to care rather than inappropriate care. Opponents of self-referral maintain that it creates incentives that can drive up rates of unnecessary or inappropriate care. Federal regulations restricting self-referral for Medicare and Medicaid patients are predicated on this concern.47,48 While our results certainly do not resolve this debate, at the very least they suggest that more research is needed to understand the relationship between self-referral and inappropriate imaging as higher utilization alone for self-referral may not be a valid indicator of inappropriate care across the spectrum of physician specialties and clinical conditions.
Our results also indicate that individual physicians are an important determinant of inappropriate imaging as this level of decision-making was relatively substantial accounting for approximately 19% of the variance for inappropriate imaging. At the same time, the variation accounted for at the practice level was fairly large suggesting that practice-level characteristics are important, which might include, for example, the availability of clinical decision support systems.
Another relevant level of the health care system is the health plan in terms of whether an MRI order underwent some form of pre-authorization review and the nature of the review process. As noted, we observed relatively lower rates of inappropriate imaging among patients with an HMO plan, which is line with some literature suggesting these types of plans have in place more stringent pre-authorization requirements for expensive clinical services.34,35 However, we did not have information regarding whether and how health plans reviewed specific claims included in the study. Based on discussions we have had with senior leaders of health insurance companies in Massachusetts, during the time frame covered by this study most orders for diagnostic imaging were required to undergo some form of pre-authorization review, but these review systems did not include the type of criteria that ACR guidelines entail and medical denial rates were very low. Some health insurance companies reportedly have since upgraded their review systems with more detailed clinical criteria for reviewing orders for diagnostic imaging. As such, an important opportunity for future research is to evaluate whether rates of inappropriate diagnostic imaging are now declining due to perhaps more highly developed review systems.
Our study has several noteworthy limitations. One is the reliance on claims data, which do not contain complete clinical information for a patient’s condition and cannot fully capture the perspective of the ordering clinician. To mitigate this concern, we selected clinical conditions for which the ACR appropriateness criteria are well defined with relatively less opportunity for clinical subtleties to influence decision-making. It also seems unlikely that this limitation would explain differences in inappropriate imaging as large as the ones observed in this study for experience and specialty training. Nevertheless, future research that re-examines the impact of such physician characteristics with data from medical records would be a valuable addition to the literature. Another is the generalizability of the study’s findings beyond Massachusetts, which has more MRIs per person than the national average.49 A third limitation is that we were unable to identify all forms of self-referral arrangements as some physician practices have complex business arrangements for conducting self-referrals that cannot be readily identified from an analysis of claims alone.50 We also point out that our study considers the impact of self-referral on inappropriate imaging only. Previous research has raised questions about self-referral based on evidence that non-radiologists provide less accurate interpretations of imaging scans than radiologists.33,51
In conclusion, our study offers to date one of the largest investigations of inappropriate diagnostic imaging. Both physician experience and specialty training appear to be important factors underlying the ordering of inappropriate imaging at least with respect to musculoskeletal conditions. We believe these findings warrant attention and should be addressed through initiatives that can improve physicians’ attention to relevant imaging guidelines.
Change history
06 May 2020
There were some errors in the variables in this paper.
References
Bautista AB, Burgos A, Nickel BJ, Yoon JJ, Tilara AA, Amorosa JK. Do clinicians use the American College of Radiology appropriateness criteria in the management of their patients? Am J Roentgenol 2009;192(6):1581–5. https://doi.org/10.2214/ajr.08.1622
Papanicola I, Woskie LR, Jha A. Health care spending in the United States and other high-income counties. JAMA. 2018; 319(10): 1024–1039. https://doi.org/10.1001/jama.2018.1150.
Choi WW, Williams SB, Gu X, Lipsitz SR, Nguyen PL, Hu JC. Overuse of imaging for staging low risk prostate cancer. J Urol 2011;185(5):1645–9. https://doi.org/10.1016/j.juro.2010.12.033
Prasad SM, Gu X, Lipsitz SR, Nguyen PL, Hu JC. Inappropriate utilization of radiographic imaging in men with newly diagnosed prostate cancer in the United States. Cancer. 2012;118(5):1260–7. https://doi.org/10.1002/cncr.26416
George E, Tsipas S, Wozniak G, Rubin DA, Seidenwurm DJ, Raghavan K, et al. MRI of the knee and shoulder performed before radiography. J Am Coll Radiol 2014;11(11):1053–8. https://doi.org/10.1016/j.jacr.2014.05.014
Flaherty S Zepeda ED, Mortele K, Young GJ. Magnitude and financial implications of inapporpriate diagnostic imaging. Int J Qual Health Care https://doi.org/10.1093/intqhc/mzy248
Mehrotra A, Reid RO, Adams JL, Friedberg MW, McGlynn EA, Hussey PS. Physicians with the least experience have higher cost profiles than do physicians with the most experience. Health Aff 2012;31(11):2453–63. https://doi.org/10.1016/j.juro.2013.03.090
Li C-J, Syue Y-J, Tsai T-C, Wu K-H, Lee C-H, Lin Y-R. The impact of emergency physician seniority on clinical efficiency, emergency department resource use, patient outcomes, and disposition accuracy. Medicine (Baltimore) 2016;95(6):e2706. https://doi.org/10.1097/md.0000000000002706
Hendee WR, Becker GJ, Borgstede JP, Bosma J, Casarella WJ, Erickson BA, et al. Addressing overutilization in medical imaging. Radiology. 2010;257(1):240–5. https://doi.org/10.7197/223.v39i29491.316370
Mazzuca SA, Brandt KD, Katz BP, Dittus RS, Freund DA, Lubitz R, et al. Comparison of general internists, family physicians, and rheumatologists managing patients with symptoms of osteoarthritis of the knee. Arthritis Care Res 1997;10(5):289–99. https://doi.org/10.1002/art.1790100503
Emery D, Shojania K, Forster A, Mojaverian N, Feasby T. Overuse of magnetic resonance imaging. JAMA Intern Med. 2013;173(9):823–5. http://archinte.jamanetwork.com/article.aspx?articleid=1672286&utm_source=email&utm_medium=ESR News January 2014&utm_content=utm_content%3Dtextlink&utm_campaign=JAMAOveruseMRI
Sheehan SE, Coburn JA, Singh H, Vanness DJ, Sittig DF, Moberg DP, et al. Reducing unnecessary shoulder MRI examinations within a capitated health care system: A potential role for shoulder ultrasound. J Am Coll Radiol 2016;13(7):780–7. https://doi.org/10.1016/j.jacr.2016.03.015
Amrhein TJ, Paxton BE, Lungren NY, Befera HR, Collins C, Yurko C, Eastwood JD and Kilani RK. Physician self referral and imaging use appropriatness: Negative cervical spine MRI frequency as an assessment metric. Am J Neuroradiol 2014; 35: 2248–53. https://doi.org/10.3174/ajnr.a4076
Mitchell JM. Utilization trends for advanced imaging procedures: evidence from individuals with private insurance coverage in California. Med Care. 2008;46(5):460–6. https://doi.org/10.1097/MLR.0b013e31815dc5ae
Levin DC, Rao VM, Parker L, Frangos AJ, Sunshine JH. Ownership or leasing of MRI facilities by nonradiologist physicians is a rapidly growing trend. J Am Coll Radiol 2008;5(2):105–9. https://doi.org/10.1016/s0098-1672(09)79382-8
Hillman BJ., Joseph CA., Mabry MR., Sunshine JH., Kennedy SD., Noether M. Frequency and costs of diagnostic imaging in office practice—a comparison of self-referring and radiologist-referring physicians. N Engl J Med 1990;323(23):1604–8. https://doi.org/10.1056/nejm199105093241920
Hughes DR, Bhargavan M, Sunshine JH. Imaging self-referral associated with higher costs and limited impact on duration of illness. Health Aff 2010;29(12):2244–51. https://doi.org/10.1377/hlthaff.2010.0413
Levin DC, Rao VM. The effect of self-referral on utilization of advanced diagnostic imaging. Am J Roentgenol 2011;196(4):848–52. https://doi.org/10.2214/ajr.10.5823
Lungren MP, Amrhein TJ, Paxton BE, Srinivasan RC, Collins HR, Eastwood JD, et al. Physician self-referral: Frequency of negative findings at mr imaging of the knee as a marker of appropriate utilization. Radiology. 2013;269(3):810–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24046441
Amrhein TJ, Paxton BE, Lungren MP, Befera NT, Collins HR, Yurko C, et al. Physician self-referral and imaging use appropriateness: Negative cervical spine MRI frequency as an assessment metric. Am J Neuroradiol 2014;35(12):2248–53. https://doi.org/10.3174/ajnr.a4076
Ma VY, Chan L, & Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: Stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. 2014; 95(5), 986–995.e1. https://doi.org/10.1016/j.apmr.2013.10.032
Center for Disease Contol and Prevention. Health, United States, 2006 with Chartbook on Trends in the Health of Americans (DHHS Publication No. 2006-1232). Washington, D.C.: U.S. Government Publishing Office. 2006. https://www.cdc.gov/nchs/data/hus/hus06.pdf. Accessed February 14, 2018.
Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: Results of an internet-based survey. J Pain. 2010; 11(11),
Centers for Medicare & Medicaid Services. Chronic Conditions. 2017. Retrieved from https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/CC_Main.html. Accessed February 21, 2018.
Timbie JW, Hussey PS, Burgette L, et al. Medicare Imaging Demonstration Report to Congress. Vol. 135. 2014. http://www.rand.org/content/dam/rand/pubs/research_reports/RR700/RR706/RAND_RR706.pdf. Accessed March 16, 2018.
Chou R, Qaseem A, Owens DK, Shekelle P, Guidelines C. Clinical guideline diagnostic imaging for low back pain : advice for high-value health care from the American College of Physicians. Ann Intern Med 2011;154:181–90.
ACR. ACR Appropriateness Criteria: Nontraumatic Knee Pain. 2012. https://acsearch.acr.org/docs/69432/Narrative/. Accessed December 11, 2018.
Patel ND, Broderick DF, Burns J, Deshmukh TK, Fries IB, Harvey HB, et al. ACR appropriateness criteria low back pain. J Am Coll Radiol 2016;1069–78. http://www.ncbi.nlm.nih.gov/pubmed/27496288. Accessed December 20, 2018.
ACR. ACR Appropriateness Criteria: Acute Shoulder Pain. 2012. https://acsearch.acr.org/docs/3101482/Narrative/
Chou R, Qaseem A, Snow V, et al. Clinical guidelines diagnosis and treatment of low back pain : A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007; 147(7), 478–491. https://doi.org/10.7326/0003-4819-147-7-200710020-00006
Lehnert BE, and Bree RL. Analysis of appropriateness of outpatient ct and mri referred from primary care clinics at an academic medical center: How critical is the need for improved decision support? J Am Coll Radiol 2010; 7(3), 192–197. https://doi.org/10.1016/j.jacr.2009.11.010
Fransen M, Crosbie J, and Edmonds J. Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. J Rheumatol 2001; 28(1), 156–164. https://www.ncbi.nlm.nih.gov/pubmed/11196518
Kouri BE et al. Physician self referral for diagnostic imaging: Review of the empiric literature. Am J Roentgenol 2002;179 (4); 840–850. https://doi.org/10.2214/ajr.179.4.1790843
Bell N, Repáraz L, Fry WR, Smith RS, Luis A. Variation in type and frequency of diagnostic imaging during trauma care across multiple time points by patient insurance type. BMC Med Imaging 2016;16(1):61. http://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-016-0146-8
Brinjikji W, El-Sayed AM, Rabinstein AA, McDonald JS, Cloft HJ. Disparities in imaging utilization for acute ischemic stroke based on patient insurance status. Am J Roentgenol 2014;203(2):372–6. https://doi.org/10.2214/ajr.13.12008
Li B, Lingsma HF, Steyerberg EW, Lesaffre E. Logistic random effects regression models: A comparison of statistical packages for binary and ordinal outcomes. BMC Med Res Methodol 2011;11:1–11. https://doi.org/10.1186/1471-2288-11-77
Schabenberger O. Introducing the Glimmix Procedure for Generalized Linear Mixed Models. SUGI 30 Proc. 2005;1–20. Available from: http://nesug.org/proceedings/nesug05/an/an4.pdf
Austin PC. Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and monte carlo simulations. Biometrical J 2009;51(1):171–84. https://doi.org/10.1002/bimj.200810488
Snijders TAB, Bosker R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. 2nd ed. Sage Publications Ltd.; 2011.
Sheng AY, Castro A, Lewiss RE. Awareness, utilization, and education of the acr appropriateness criteria: a review and future directions. J Am Coll Radiol 2016;13(2):131–6. https://doi.org/10.1016/j.jacr.2015.08.026
Powell DK, Silberzweig JE. The use of ACR Appropriateness Criteria: A survey of radiology residents and program directors. Clin Imaging 2015;39(2):334–8. https://doi.org/10.1016/j.clinimag.2014.10.011
Covington MF, Agan DL, Liu Y, Johnson JO, Shaw DJ. Teaching cost-conscious medicine: Impact of a simple educational intervention on appropriate abdominal imaging at a community-based teaching hospital. J Grad Med Educ 2013;5(2):284–8. http://www.jgme.org/doi/abs/10.4300/JGME-D-12-00117.1
Kozak B, Webb EM, Khan BK, Orozco NM, Straus CM, Naeger DM. Medical student usage of the american college of radiology appropriateness criteria. Acad Radiol 2015;22(12):1606–11. https://doi.org/10.1016/j.acra.2015.08.011
Rao VM, Levin DC. The overuse of diagnostic imaging and the choosing wisely initiative. Ann Intern Med 2012;157(8):574–6. https://doi.org/10.7326/0003-4819-157-8-201210160-00535
Vartanians VM, Sistrom CL, Weilburg JB, Rosenthal DI, Thrall JH. Increasing the appropriateness of outpatient imaging: Effects of a barrier to ordering low-yield examinations. Radiology. 2010; 255(3): 842–849. https://doi.org/10.1148/radiol.10091228
Center for Medicare and Medicaid Services. Appropriate Use Criteria Program. 2019. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Appropriate-Use-Criteria-Program/index.html. Accessed July 15, 2018.
Government Accountability Office. Medicare: Implementation of Financial Incentive Programs Under Federal Fraud and Abuse Laws (GAO-12-355) March 2012. https://www.gao.gov/products/GAO-12-355
Goodell S and Cassalino LP. Physician self referral and physician-owned specialty facilities. Policy Brief. Robert Wood Johnson Foundation. 2008. https://www.rwjf.org/en/library/research/2008/06/physician-self-referral-and-physician-owned-specialty-facilities0.html
Sullivan J. Overexposed. Commonwealth Magazine. 2010, pp. 1–8. https://commonwealthmagazine.org/health-care/overexposed/
Mitchell JM. The prevalence of physician self-referral arrangements after stark II: Evidence from advanced diagnostic imaging. Health Aff. 2007;26(3). https://doi.org/10.1377/hlthaff.26.3.w415
Paxton BE, Lungren MP, Srinivasan RC, Jung SH, Yu M, Eastwood JD, et al. Physician self-referral of lumbar spine MRI with comparative analysis of negative study rates as a marker of utilization appropriateness. Am J Roentgenol 2012;198(6):1375–9. https://doi.org/10.2214/ajr.11.
Funding
This study received financial support from the National Institute for Health Care Management Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Young, G.J., Flaherty, S., Zepeda, E.D. et al. Effects of Physician Experience, Specialty Training, and Self-referral on Inappropriate Diagnostic Imaging. J GEN INTERN MED 35, 1661–1667 (2020). https://doi.org/10.1007/s11606-019-05621-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05621-3