Abstract
Background
Urinary and sexual dysfunctions are frequent after surgery for rectal cancer. Total mesorectal excision (TME) improves local recurrence and survival rates, and does not hamper recognition and sparing of hypogastric and pelvic splanchnic nerves. It is not known how laparoscopic rectal resection could change functional complication rates.
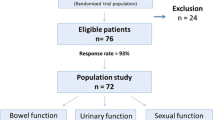
Materials and Methods
From a global series of 1,216 laparoscopic interventions for colorectal diseases, 35 cases of males less than 70 years old, undergoing rectal resection and TME for a T1-3M0 medium and low rectal cancer were selected. Urinary and sexual functions after the operations were retrospectively recorded by means of specific tools (International Prostate Symptom Score (IPSS) and IIEF questionnaires, respectively).
Results
None of the patients necessitated permanent or intermittent catheterization. More than half the patients had no complaints about urinary functions; about one third had nocturia; 72% of the patients had an IPSS less that 10, and no case of IPSS worse that 31 was recorded. Sexual desire was reduced and spontaneous erectile function was impaired in almost half the cases, while induced erections were possible in about 90% of cases; about 70% of patients still had the possibility of penetration and a normal ejaculation and orgasm after the intervention.
Discussion and Conclusions
The present series confirms previous data and contribute to the creation of a benchmark specifically related to the laparoscopic approach to which surgeons should face when informing the patients before the operation. While severe urinary dysfunction is rare, sexual impairment remains a serious concern after rectal resection with TME.
Similar content being viewed by others
References
Keating J. Sexual function after rectal excision. ANZ J Surg 2004; 74,248–259
Pikarsky A, Rosenthal R, Weiss E, Wexner S. Laparoscopic total mesorectal excision. Surg Endosc 2002; 16,558–562
Lelong B, Bege T, Esterni B, et al. Short–term outcome after laparoscopic or open restorative mesorectal excision for rectal cancer: a comparative cohort study. Dis Colon Rectum 2007; 50,176–183
Sartori CA. Trattato di tecnica chirurgica laparoscopica del colon e del retto. 2008, Ed. Surgical Video Production spa, pagg 334
Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, Cockett AT. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992; 148:1549-57
Rosen R, Riley A, Wagner G, Osterloh I, Kirkpatrick J, Mishra A. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 1997; 49,822–830
Fazio V, Fletcher J, Montague D. Prospective study of the effect of resection of the rectum on male sexual function. World J Surg 1980; 4,149–152
Heald R. The ‘holy Plane’ of rectal surgery. J R Soc Med 1988; 81,503–508
Hojo K, Vernava AI, Sugihara K, Katumata K. Preservation of urine voiding and sexual function after rectal cancer surgery. Dis Colon Rectum1991; 34,532–539
Akasu T, Sugihara K, Moriya Y. Male urinary and sexual functions after mesorectal excision alone or in combination with extended lateral pelvic lymph node dissection for rectal cancer. Ann Surg Oncol 2009; 16:2779-86
Kyo K, Sameshima S, Takahashi M, Furugori T, Sawada T. Impact of autonomic nerve preservation and lateral node dissection on male urogenital function after total mesorectal excision for lower rectal cancer. World J Surg 2006; 30:1014-9
Heald R, Husband E, Ryall R. The mesorectum in rectal cancer surgery – the clue to pelvic recurrence? Br. J. Surg 1982; 69,613–616.
Enker W, Thaler H, Cranor M. Total mesorectal excision in the operative treatment of carcinoma of the rectum. J Am Coll Surg 1995; 181,335–346.
Havenga K, Enker W, McDermott K, Cohen A, Minsky B, Guillem J. Male and female sexual and urinary function after total mesorectal excision with autonomic nerve preservation for carcinoma of the rectum. J Am Coll Surg 1996; 182,495–502.
Sterk P, Shekarriz B, Ganter S, Nolde J, Keller R, Bruch HP, Shekarriz H. Voiding and sexual dysfunction after deep rectal resection and total mesorectal excision: prospective study on 52 patients. Int J Colorectal Dis 2005; 20:423-7.
Kneist W, Junginger T. Male urogenital function after confirmed nerve-sparing total mesorectal excision with dissection in front of Denonvilliers’ fascia. World J Surg 2007; 31:1321-8.
Kim N, Aahn T, Park J, et al. Assessment of sexual and voiding function after total mesorectal excision with pelvic autonomic nerve preservation in males with rectal cancer. Dis Colon Rectum 2002; 45,1178–1185.
Nesbakken A, Nygaard K, Bull–Njaa T, Carlsen E, Eri, L. Bladder and sexual dysfunction after mesorectal excision for rectal cancer. Br J Surg 2000; 87,206–210.
Masui H, Ike H, Yamaguchi S, Oki S, Shimada H. Male sexual function after autonomic nerve–preserving operation for rectal cancer. Dis Colon Rectum 1996; 39,1140–1145.
Pocard M, Zinzindohoue F, Haab F, Caplin S, Parc R, Tiret E. A prospective study of sexual and urinary function before and after total mesorectal excision with autonomic nerve preservation for rectal cancer. Surgery 2002; 131,368–372.
Hanna NN, Guillem J, Dosoretz A, Steckelman E, Minsky BD, Cohen AM. Intraoperative parasympathetic nerve stimulation with tumescence monitoring during total mesorectal excision for rectal cancer. J Am Coll Surg. 2002; 195:506-12.
Quah H, Jayne D, Eu K, Seow–Choen F. Bladder and sexual dysfunction following laparoscopically assisted and conventional open mesorectal resection for cancer. Br J Surg 2002; 89,1551–1556.
Jayne D, Brown J, Thorpe H, Walker J, Quirke P, Guillou P. Bladder and sexual function following resection for rectal cancer in a randomized clinical trial of laparoscopic versus open technique. Br J Surg 2005; 92,1124–1132.
Asoglu O, Matlim T, Karanlik H, et al. Impact of laparoscopic surgery on bladder and sexual function after total mesorectal excision for rectal cancer. Surgical Endoscopy 2009; 23:296-303.
Liang JT, Lai HS, Lee PH. Laparoscopic pelvic autonomic nerve-preserving surgery for patients with lower rectal cancer after chemoradiation therapy. Ann Surg Oncol. 2007; 14:1285-7.
Morino M, Parini U, Allaix ME, Monasterolo G, Brachet Contul R, Garrone C. Male sexual and urinary function after laparoscopic total mesorectal excision. Surg Endosc. 2009; 23:1233-40.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sartori, C.A., Sartori, A., Vigna, S. et al. Urinary and Sexual Disorders After Laparoscopic TME for Rectal Cancer in Males. J Gastrointest Surg 15, 637–643 (2011). https://doi.org/10.1007/s11605-011-1459-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1459-0