Abstract
Purpose
The purpose of this study was to evaluate how the reference fat position influenced the calculation of the sonoelastographic strain ratio.
Methods
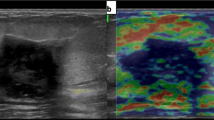
Three hundred fifty-eight breast masses (256 benign lesions and 102 malignant lesions) in 300 women (mean age 47.4 years; age range 17–82 years) who had been scheduled for a percutaneous needle biopsy or surgical excision were examined using B-mode ultrasonography and elastography. The sonoelastographic strain ratio was calculated twice per lesion; once by dividing the strain value of the fat near the mass by that of the mass (FLR 1) and once by dividing the strain value of the subcutaneous fat by that of the mass (FLR 2).
Results
Most (91.9 %) showed a difference of less than 0.5 between FLR 1 and FLR 2 values. Regardless of the position of reference fat, there was no statistically significant difference between the FLR 1 and FLR 2 values (p value = 0.077 and 0.0825, respectively). According to the pathology of the lesion, a difference between FLR 1 and FLR 2 less than 0.5 occurred in 95.3 % of the benign lesions and 84 % of the malignant lesions (p < 0.001).
Conclusions
The sonoelastographic strain ratio was not significantly affected by the position of reference fat.



Similar content being viewed by others
References
Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas J-M, Gilja OH, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med. 2013;34:238–53.
Bamber J, Cosgrove D, Dietrich CF, Fromageau J, Bojunga J, Calliada F, et al. EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: Basic principles and technology. Ultraschall Med. 2013;34:169–84.
Mendelson EB, Böhm-Vélez M, Berg WA, Whitman GJ, Feldman MI, Madjar H, et al. ACR BI-RADS® Ultrasound. In: D’Orsi CJ, Sickles EA, Mendelson EB, et al., editors. ACR BI-RADS® atlas, breast imaging reporting and data system. 5th ed. Reston: American College of Radiology; 2013.
Itoh A, Ueno E, Tohno E, Kamma H, Takahashi H, Shiina T, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239:341–50.
Ueno E, Umemoto T, Bando H, TohnoE, Waki K, Matsumura T. New quantitative method in breast elastography: fat lesion ratio (FLR). In: Radiological Society of North America 2007 Scientific Assembly and Annual Meeting, November 25 November 30, 2007. http://archive.rsna.org/2007/5015476.html. Accessed 17 July 2014.
Zhi H, Xiao XY, Yang HY, Wen YL, Ou B, Luo BM, et al. Semi-quantitating stiffness of breast solid lesions in ultrasonic elastography. Acad Radiol. 2008;15:1347–53.
Cho N, Moon WK, Kim HY, Chang JM, Park SH, Lyou CY. Sonoelastographic strain index for differentiation of benign and malignant nonpalpable breast masses. J Ultrasound Med. 2010;29:1–7.
Zhi H, Xiao XY, Yang JY, Wen YL, Ou B, Luo BM, et al. Ultrasonic elastography in breast cancer diagnosis: strain ratio vs 5-point scale. Acad Radiol. 2010;17:1227–33.
Thomas A, Degenhardt F, Farrokh A, Wojcinski S, Slowinski T, Fischer T. Significant differentiation of focal breast lesions: calculation of strain ratio in breast sonoelastography. Acad Radiol. 2010;17:558–63.
Fischer T, Peisker U, Fiedor S, Slowinski T, Wedemeyer P, Diekmann F, et al. Significant differentiation of focal breast lesions: raw data-based calculation of strain ratio. Ultraschall Med. 2012;33:372–9.
Stachs A, Hartmann S, Stubert J, Dieterich M, Martin A, Kundt G, et al. Differentiating between malignant and benign breast masses: factors limiting sonoelastographic strain ratio. Ultraschall Med. 2013;34:131–6.
Zhi H, Ou B, Luo BM, Feng X, Wen YL, Yang HY. Comparison of ultrasound elastography, mammography, and sonography in the diagnosis of solid breast lesions. J Ultrasound Med. 2007;26:807–15.
Waki K, Murayama N, Matsumura T, Mitake T. Investigation of strain ratio using ultrasound elastography technique. In: Proceedings of ISICE: The first international symposium on information and computer elements. Kitakyushu, Japan, Sep 12–14, 2007, pp 449–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Jung, N.Y., Park, C.S., Kim, S.H. et al. Sonoelastographic strain ratio: how does the position of reference fat influence it?. Jpn J Radiol 34, 440–447 (2016). https://doi.org/10.1007/s11604-016-0543-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-016-0543-5