Abstract
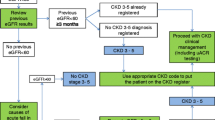
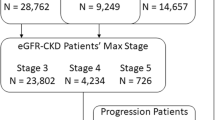
Whether automated estimated glomerular filtration rate (eGFR) reporting for patients is associated with improved provider recognition of chronic kidney disease (CKD), as measured by diagnostic coding of CKD in those with laboratory evidence of the disease, has not been explored in a poor, ethnically diverse, high-risk urban patient population. A retrospective cohort of 237 adult patients (≥20 years) with incident CKD (≥1 eGFR ≥60 ml/min/1.73 m2, followed by ≥2 eGFRs <60 ml/min/1.73 m2 ≥3 months apart)—pre- or postautomated eGFR reporting—was identified within the San Francisco Department of Public Health Community Health Network (January 2005–July 2009). Patients were considered coded if any ICD-9-CM diagnostic codes for CKD (585.x), other kidney disease (580.x–581.x, 586.x), or diabetes (250.4) or hypertension (403.x, 404.x) CKD were present in the medical record within 6 months of incident CKD. Multivariable logistic regression was used to obtain adjusted odds ratios (ORs) for CKD coding. We found that, pre-eGFR reporting, 42.5 % of incident CKD patients were coded for CKD. Female gender, increased age, and non-Black race were associated with lower serum creatinine and lower prevalence of coding but comparable eGFR. Prevalence of coding was not statistically significantly higher overall (49.6 %, P = 0.27) or in subgroups after the institution of automated eGFR reporting. However, gaps in coding by age and gender were narrowed post-eGFR, even after adjustment for sociodemographic and clinical characteristics: 47.9 % of those <65 and 30.3 % of those ≥65 were coded pre-eGFR, compared to 49.0 % and 52.0 % post-eGFR (OR = 0.43 and 1.16); similarly, 53.2 % of males and 25.4 % of females were coded pre-eGFR compared to 52.8 % and 44.0 % post-eGFR (OR 0.28 vs. 0.64). Blacks were more likely to be coded in the post-eGFR period: OR = 1.08 and 1.43 (P interaction > 0.05). Automated eGFR reporting may help improve CKD recognition, but it is not sufficient to resolve underidentification of CKD by safety net providers.


Similar content being viewed by others
References
Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007; 298(17): 2038–2047.
U. S. Renal Data System. USRDS 2010 annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2010.
Boulware LE, Troll MU, Jaar BG, Myers DI, Powe NR. Identification and referral of patients with progressive CKD: a national study. Am J Kidney Dis. 2006; 48(2): 192–204.
Agrawal V, Ghosh AK, Barnes MA, McCullough PA. Perception of indications for nephrology referral among internal medicine residents: a national online survey. Clin J Am Soc Nephrol. 2009; 4(2): 323–328.
Lea JP, McClellan WM, Melcher C, Gladstone E, Hostetter T. CKD risk factors reported by primary care physicians: do guidelines make a difference? Am J Kidney Dis. 2006; 47(1): 72–77.
Hall YN, Choi AI, Chertow GM, Bindman AB. Chronic kidney disease in the urban poor. Clin J Am Soc Nephro. 2010; 5(5): 828–835.
Crews DC, Charles RF, Evans MK, Zonderman AB, Powe NR. Poverty, race, and CKD in a racially and socioeconomically diverse urban population. Am J Kidney Dis. 2010; 55: 992–1000.
McClellan WM, Newsome BB, McClure LA, Howard G, Volkova N, Audhya P, Warnock DG. Poverty and racial disparities in kidney disease: the REGARDS study. Am J Nephrol. 2010; 32: 38–46.
Bruce MA, Beech BM, Crook ED, Sims M, Wyatt SB, Flessner MF, Taylor HA, Williams DR, Akylbekova EL, Ikizler TA. Association of socioeconomic status and CKD among African Americans: the Jackson Heart study. Am J Kidney Dis. 2010; 55: 1001–1008.
Mehrotra R, Norris K. Hypovitaminosis D, neighborhood poverty, and progression of chronic kidney disease in disadvantaged populations. Clin Nephrol. 2010; 74(Suppl 1): S95–8.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. modification of diet in renal disease study group. Ann Intern Med. 1999; 130(6): 461–470.
Guessous I, McClellan W, Vupputuri S, Wasse H. Low documentation of chronic kidney disease among high-risk patients in a managed care population: a retrospective cohort study. BMC Nephrol. 2009; 10: 25.
Grams ME, Plantinga LC, Hedgeman E, et al. Validation of CKD and related conditions in existing data sets: a systematic review. Am J Kidney Dis. 2011; 57: 44–54.
Richards N, Harris K, Whitfield M, et al. Primary care-based disease management of chronic kidney disease (CKD), based on estimated glomerular filtration rate (eGFR) reporting, improves patient outcomes. Nephrol Dial Transplant. 2008; 23(2): 549–555.
Noble E, Johnson DW, Gray N, et al. The impact of automated eGFR reporting and education on nephrology service referrals. Nephrol Dial Transplant. 2008; 23(12): 3845–3850.
Hemmelgarn BR, Zhang J, Manns BJ, et al. Nephrology visits and health care resource use before and after reporting estimated glomerular filtration rate. JAMA. 2010; 303(12): 1151–1158.
Kagoma YK, Weir MA, Iansavichus AV, et al. Impact of estimated GFR reporting on patients, clinicians, and health-care systems: a systematic review. Am J Kidney Dis. 2011; 57: 592–601.
Abdel-Kader K, Fischer GS, Johnston JR, Gu C, Moore CG, Unruh ML. Characterizing pre-dialysis care in the era of eGFR reporting: a cohort study. BMC Nephrol. 2011; 12(1): 12.
Cheung CK, Bhandari S. Perspectives on eGFR reporting from the interface between primary and secondary care. Clin J Am Soc Nephrol. 2009; 4(2): 258–260.
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150(9): 604–612.
Acknowledgments
We thank the patients and providers of the San Francisco Department of Community Health Network. Ms. Plantinga and Dr. Powe were partially supported by K24DK02643, Dr. Hsu was partially supported by K24DK92291, and Drs. Hsu and Powe were partially supported by R34DK093992, all from the National Institute of Diabetes, Digestive and Kidney Diseases, Bethesda, MD. Dr. Tuot was partially supported by UCSF KL2 RR024130 and an American Kidney Fund Clinical Scientist in Nephrology grant. Dr. Grubbs is supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Renal Diseases Diversity Supplement to R01 DK70939.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Plantinga, L.C., Tuot, D.S., Grubbs, V. et al. Chronic Kidney Disease Identification in a High-Risk Urban Population: Does Automated eGFR Reporting Make a Difference?. J Urban Health 89, 965–976 (2012). https://doi.org/10.1007/s11524-012-9726-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-012-9726-2