Abstract
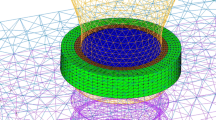
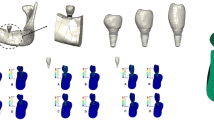
The purpose of this study was to explore the biomechanical effects of progressive marginal bone loss in the peri-implant bone. Finite element model of a Ø 4.1 × 10 mm Straumann dental implant and a solid abutment was constructed as predefined eight-layers around the implant neck. The implant-abutment complex was embedded in a cylindrical bone model to analyze bone biomechanics regardless of anatomical influences. Angular and circular progressive marginal bone loss was simulated by sequential removal of each layer, resulting crater-like defects and a total of ten finite element models for analysis. Each model was subjected to a vertical and oblique static load of 100 N in separate load cases. Principal stress minimum and maximum, displacement, and equivalent of elastic strain outcomes were compared. Under vertical loading, principal stresses minimum and maximum decreased remarkably as with the increase in bone resorption. Under oblique load simulations, decrease in principal stress maximum and minimum was evident. With progressive bone loss and under oblique load simulations, displacement and equivalent of elastic strain increased considerably in trabecular bone contacting the implant neck. The presence of cortical bone contacting a load-carrying implant, even in a bone defect, improves the biomechanical performance of implants in comparison with only trabecular bone support as a sequel of progressive marginal bone loss.





Similar content being viewed by others
References
Akca K, Cehreli MC, Iplikcioglu H (2003) Evaluation of the mechanical characteristics of the implant-abutment complex of a reduced-diameter morse-taper implant. A nonlinear finite element stress analysis. Clin Oral Implants Res 14:444–455
Akca K, Iplikcioglu H (2002) Finite element stress analysis of the effect of short -implant usage in place of cantilever extensions in mandibular posterior edentulism. J Oral Rehabil 4:350–356
Astrand P, Engquist B, Dahlgren S, Engquist E, Feldmann H, Grondahl K (1999) Astra tech and Brånemark system implants: a prospective 5-year comparative study. Results after one year. Clin Implant Dent Relat Res 1:17–26
Barbier L, Schepers E (1997) Adaptive bone remodeling around oral implants under axial and nonaxial loading conditions in the dog mandible. Int J Oral Maxillofac Implants 12:215–223
Brägger U (1998) Use of radiographs in evaluating success, stability and failure in implant dentistry. Periodontol 2000 17:77–88
Cehreli MC, Akca K, Iplikcioglu H (2004a) Force transmission of one- and two-piece morse-taper oral implants: a nonlinear finite element analysis. Clin Oral Implants Res 15:481–9
Cehreli M, Akkocaoğlu. M, Cömert A, Tekdemir I, Akca K (2005) Human ex vivo bone tissue strains around natural teeth versus immediate oral implants. Clin Oral Implants Res 16:540–548
Cehreli M, Sahin S, Akca K (2004b) Role of mechanical environment and implant design on bone tissue differentiation: current knowledge and future contexts. J Dent 32:123–132
Cehreli MC, Akca K (2005) Mechanobiology of bone and mechanocoupling of endosseous titanium oral implants. J Long Term Eff Med Implants 15:139–152
Davarpanah M, Martinez H, Etienne D, Zabalegui I, Mattout P, Chiche F, Michel JF (2002) A prospective multicenter evaluation of 1,583 3i implants: 1- to 5-year data. Int J Oral Maxillofac Implants 17:820–8
Esposito M, Hirsch J-M, Lekholm U, Thompsen P (1998). Biological factors contributing to failures of osseointegrated oral implants (II) Etiopathogenesis. Eur J Oral Sci 106:721–764
Esposito M, Worthington HV, Coulthard P (2001) In search of truth: the role of systematic reviews and meta-analyses for assessing the effectiveness of rehabilitation with oral implants. Clin Implant Dent Relat Res 3:62–78
Frost HM (1987a) Bone “mass” and “mechanostat”, a proposal. Anat Rec 219:1–19
Frost HM (1987b) The mechanostat proposed pathogenic mechanism of osteoporoses and the bone mass effects of mechanical and nonmechanical agents. Bone Miner 2:73–85
Frost HM (1997) Perspective, on our-age related bone loss: Insights from a new paradigm. J Bone Miner Res 12:1539–1546
Goldman FM, Millsap JS, Brenman HS (1957) Origin of registration of the architectural pattern, the lamina dura, and the alveolar crest in the dental radiograph. Oral Surg Oral Med Oral Pathol 10:749–58
Goaz PW, White SC (eds) (1987) Oral radiology: principles and interpretation. 176. St Louis: CV Mosby company
Heitz-Mayfield LJ, Schmid B, Weigel. C, Gerber. S, Bosshardt. DD, Jönsson J, Lang NP (2004) Does excessive occlusal load affect osseointegration? An experimental study in the dog. Clin Oral Implants Res 15:259–268
Hoshaw SJ, Brunski JB, Cochran GVB (1994) Mechanical loading of Brånemark implants affects interfacial bone modeling and remodeling. Int J Oral Maxillofac Implants 9:345–360
Isidor F (1996) Loss of osseointegration caused by occlusal load of oral implants. A clinical and radiographic study in monkeys. Clin Oral Implants Res 7:143–152
Jee WSS (2001) Integrated bone tissue physiology: Anatomy and physiology. In: Cowin SC (eds) Bone mechanics handbook. CRP LLC, Florida, pp 1–35
Kitamura E, Stegaroiu R, Nomura S, Miyakawa O (2004) Biomechanical aspects of marginal bone resorption around osseointegrated implants: considerations based on a three-dimensional finite element analysis. Clin Oral Implants Res 15:401–412
Kitamura E, Stegaroiu R, Nomura S, Miyakawa O (2005) Influence of marginal bone resorption on stress around an implant – a three-dimensional finite element analysis. J Oral Rehabil 32:279–286
Lang NP, Brëgger U, Walther D, Beamer B, Kornman KS (1993) Ligature-induced periimplant infection in cynomolgus monkeys. I. Clinical and radiographic findings. Clin Oral Implants Res 4:2–11
Lindhe J, Berglundh T, Ericsson I, Liljenberg B, Marinello C (1992) Experimental breakdown of peri-implant and periodontal tissues. Clin Oral Implants Res 3:9–16
Mellal A, Wiskott HWA, Botsis J, Scherrer SS, Belser UC (2004) Stimulating effect of implant loading on surrounding bone. Comparison of three numerical models and validation by in vivo data. Clin Oral Implants Res 15:239–248
Melsen B, Lang NP (2001) Biological reactions of alveolar bone to orthodontic loading of oral implants. Clin Oral Implants Res 12:144–152
Miyata T, Kobayashi Y, Araki H, Motomura Y, Shin K (1998) The influence of controlled occlusal overload on peri-implant tissue: a histologic study in monkeys. Int J Oral Maxillofac Implants 13:677–683
Miyata T, Kobayashi Y, Araki H, Motomura Y, Shin K (2000) The influence of controlled occlusal overload on peri-implant tissue. Part: 3 a histologic study in monkeys. Int J Oral Maxillofac Implants 15:425–431
Moberg LE, Kondell PA, Sagulin GB, Bolin A, Heimdahl A, Gynther GW (2001) Brånemark system and ITI dental implant system for treatment of mandibular edentulism. A comparative randomized study 3-year follow-up. Clin Oral Implants Res 12:450–61
Mombelli A (1999) Prevention and therapy of periimplant infections. In: Lang NP, Karring T, Lindhe J (eds) Proceedings of the third European wsorkshop on Periodontology. Quintessenz Verlag, Berlin pp 281–303
Mericske-Stern R, Piotti M, Sirtes G (1996) 3-D in vivo force measurements on mandibular implants supporting overdentures. A comparative study. Clin Oral Implants Res 7:387–396
Quirynen M, Naert I, van Steenberghe D (1992) Fixture design and overload influence marginal bone loss and fixture success in the Brånemark system. Clin Oral Implants Res 3:1–8
Ricci G, Aimetti M, Stablum W, Guasti A (2004) Crestal bone resorption 5 years after implant loading: clinical and radiologic results with a 2-stage implant system. Int J Oral Maxillofac Implants 19:597–602
Sanz M, Alandex J, Lazaro P, Calvo JL, Quirynen M, van Steenberghe D (1991) Histopathologic characteristics of peri-implant soft tissues in Branemark implants with 2 district clinical and radiological patterns. Clin Oral Implants Res 2:128–134
Schou S, Holmstrup P, Reibel J, Juhl M, Hjorting-Hansen E, Kornman KS (1993) Ligature-induced marginal inflammation around osseointegrated implants and ankylosed teeth: stereologic and histologic observations in cynomolgus monkeys (Macaca fascicularis). J Periodontol 64:529–537
Turner CH (1999) Toward a mathematical description of bone biology: the principle of cellular accomodation. Calcif Tissue Int 65:466–471
Weber HP, Crohin CC, Fiorellini JP (2000) A 5-year prospective clinical and radiographic study of non-submerged dental implants. Clin Oral Implants Res 11:144–53
Wennström J, Zurdo J, Karlsson S, Ekestubbe A, Gröndahl K, Lindhe J (2004) Bone level change at implant-supported fixed partial dentures with and without cantilever extension after 5 years in function. J Clin Periodontol 31:1077–1083
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akca, K., Cehreli, M.C. Biomechanical consequences of progressive marginal bone loss around oral implants: a finite element stress analysis. Med Bio Eng Comput 44, 527–535 (2006). https://doi.org/10.1007/s11517-006-0072-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-006-0072-y