Abstract
Background
Acute care events including emergency department (ED) visits and unscheduled inpatient re-admissions following lower-extremity arthroplasty are not fully understood.
Question/Purposes
The purpose of this study was to characterize acute care events occurring after discharge in patients who received a lower-extremity arthroplasty: the incidence, timing, and risk factors of inpatient admission and ED visits within 90 days of discharge.
Methods
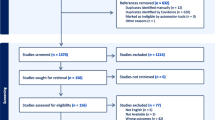
The New York State Inpatient and Emergency Department Databases were used to identify patients who underwent elective total knee arthroplasty (TKA) or total hip arthroplasty (THA) from 2009 to 2013 (124,234 and 76,411 patients, respectively). Multivariate logistic regression analysis was used to determine the predictors of and the most frequent reasons for unscheduled acute care within 90 days of discharge.
Results
Unscheduled acute care was needed in 13.79% of patients (8.81% of inpatient re-admissions and 4.98% of ED visits), most often in the first week after discharge (61.05% of all inpatient re-admissions and 20.46% of all ED visits). Most of these visits were for musculoskeletal pain, peri-prosthetic joint or wound infection, cardiac complications, blood transfusion, psychiatric events, mechanical complications, and deep vein thrombosis. Predictors for the need for acute care after TKA included African American and Hispanic race or ethnicity, Medicaid coverage, and neuraxial anesthesia. Predictors for the need for acute care after THA included older age (over 85 years), African American race, and Medicaid coverage.
Conclusion
We identified demographic and procedure-related variables associated with an increased risk of ED visits and inpatient re-admissions after TKA or THA. Understanding these variables will contribute to improved care quality.






Similar content being viewed by others
References
Adelani MA, Keeney JA, Nunley RM, Clohisy JC, Barrack RL. Readmission following total knee arthroplasty: venous thromboembolism as a “never event” is a counterproductive misnomer. J Arthroplasty . 2013;28:747–750.
Adelani MA, Keller MR, Barrack RL, Olsen MA. The impact of hospital volume on racial differences in complications, readmissions, and emergency department visits following total joint arthroplasty. J Arthroplasty. 2018;33(2):309–315.
Avram V, Petruccelli D, Winemaker M, de Beer J. Total joint arthroplasty readmission rates and reasons for 30-day hospital readmission. J Arthroplasty. 2014;29:465–468.
Bedard NA, Pugely AJ, McHugh MA, Lux NR, Bozic KJ, Callaghan JJ. Big data and total hip arthroplasty: how do large databases compare? J Arthroplasty. 2017;33(1):41–45.
Bini SA, Fithian DC, Paxton LW, Khatod MX, Inacio MC, Namba RS. Does discharge disposition after primary total joint arthroplasty affect readmission rates? J Arthroplasty. 2010;25:114–117.
Bohl DD, Ondeck NT, Basques BA, Levine BR, Grauer JN. What is the timing of general health adverse events that occur after total joint arthroplasty? Clin Orthop Relat Res. 2017;475: p. 2952–2959.
Boozary AS, Manchin J 3rd, Wicker RF. The medicare hospital readmissions reduction program: time for reform. JAMA. 2015;314:347–348.
Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am. 2010;92:2643–2652.
Browne JA, Novicoff WM, D’Apuzzo MR. Medicaid payer status is associated with in-hospital morbidity and resource utilization following primary total joint arthroplasty. J Bone Joint Surg Am. 2014;96:e180.
Cai X, Cram P, Vaughan-Sarrazin M. Are African American patients more likely to receive a total knee arthroplasty in a low-quality hospital? Clin Orthop Relat Res. 2012;470:1185–1193.
Centers for Medicare & Medicaid Services. Medicare program: comprehensive care for joint replacement payment model for acute care hospitals furnishing lower extremity joint replacemnt services. Federal register. 2015. Available at https://www.federalregister.gov/documents/2015/11/24/2015-29438/medicare-program-comprehensive-care-for-joint-replace. Accessed January 22, 2018.
Chen BP, Dobransky J, Poitras S, Forster A, Beaulé PE. Impact of definition and timeframe on capturing surgery-related readmissions after primary joint arthroplasty. J Arthroplasty. 2017;32:3563–3567.
Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–1236.
D’Apuzzo M, Westrich G, Hidaka C, Pan TJ, Lyman S. All-cause versus complication-specific readmission following total knee arthroplasty. J Bone Joint Surg Am. 2017;99:1093–1103.
Edwards PK, Levine M, Cullinan K, Newbern G, Barnes CL. Avoiding readmissions-support systems required after discharge to continue rapid recovery? J Arthroplasty. 2015;30:527–530.
Finnegan MA, Shaffer R, Remington A, Kwong J, Curtin C, Hernandez-Boussard T. Emergency department visits following elective total hip and knee replacement surgery: identifying gaps in continuity of care. J Bone Joint Surg Am. 2017;99:1005–1012.
Gold HT, Slover JD, Joo L, Bosco J, Iorio R, Oh C. Association of depression with 90-day hospital readmission after total joint arthroplasty. J Arthroplasty. 2016;31:2385–2388.
Keeney JA, Adelani MA, Nunley RM, Clohisy JC, Barrack RL. Assessing readmission databases: how reliable is the information? J Arthroplasty. 2012;27:72.
Kelly MP, Prentice HA, Wang W, Fasig BH, Sheth DS, Paxton EW. Reasons for ninety-day emergency visits and readmissions after elective total joint arthroplasty: results from a us integrated healthcare system. J Arthroplasty. 2018;33(7):2075–2081.
Kiridly DN, Karkenny AJ, Hutzler LH, Slover JD, Iorio R, Bosco JA 3rd. The effect of severity of disease on cost burden of 30-day readmissions following total joint arthroplasty (TJA). J Arthroplasty. 2014;29:1545–1547.
Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306:1794–1795.
Kocher KE, Nallamothu BK, Birkmeyer JD, Dimick JB. Emergency department visits after surgery are common for Medicare patients, suggesting opportunities to improve care. Health Aff (Millwood). 2013;32:1600–1607.
Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT. Hospital, patient, and clinical factors influence 30- and 90-day readmission after primary total hip arthroplasty. J Arthroplasty. 2016;31:2130–2138.
Newman JM, de Paz Nieves A, Cáceres Sánchez L, Lee Y, Gonzalez Della Valle A. Women and minorities are at risk of developing unexpected reduction of preoperative flexion after total knee arthroplasty. J Arthroplasty. 2016;31:781–785.
Oronce CIA, Shao H, Shi L. Disparities in 30-day readmissions after total hip arthroplasty. Med Care. 2015;53:924–930.
Paxton EW, Inacio MCS, Singh JA, Love R, Bini SA, Namba RS. Are there modifiable risk factors for hospital readmission after total hip arthroplasty in a us healthcare system? Clin Orthop Relat Res. 2015;473:3446–3455.
Pugely AJ, Callaghan JJ, Martin CT, Cram P, Gao Y. Incidence of and risk factors for 30-day readmission following elective primary total joint arthroplasty: analysis from the ACS-NSQIP. J Arthroplasty. 2013;28:1499–1504.
Raines BT, Ponce BA, Reed RD, Richman JS, Hawn MT. Hospital acquired conditions are the strongest predictor for early readmission: an analysis of 26,710 arthroplasties. J Arthroplasty. 2015;30:1299–307.
Ricciardi BF, Oi KK, Daines SB, Lee Y-Y, Joseph AD, Westrich GH. Patient and perioperative variables affecting 30-day readmission for surgical complications after hip and knee arthroplasties: a matched cohort study. J Arthroplasty. 2017;32:1074–1079.
Saucedo JM, Marecek GS, Wanke TR, Lee J, Stulberg SD, Puri L. Understanding readmission after primary total hip and knee arthroplasty: who’s at risk? J Arthroplasty. 2014;29:256–260.
Schairer WW, Sing DC, Vail TP, Bozic KJ. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res. 2014;472:464–470.
Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res. 2014;472:181–187.
Stone AH, Dunn L, MacDonald JH, King PJ. Reducing length of stay does not increase emergency room visits or readmissions in patients undergoing primary hip and knee arthroplasties. J Arthroplasty. 2018; pii: S0883-5403(18)30301-2.
Trimba R, Laughlin RT, Krishnamurthy A, Ross JS, Fox JP. Hospital-based acute care after total hip and knee arthroplasty: implications for quality measurement. J Arthroplasty. 2016;31:573–578.e2.
Vashi AA, Fox JP, Carr BG, D’Onofrio G, Pines JM, Ross JS, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309:364–371.
Vorhies JS, Wang Y, Herndon JH, Maloney WJ, Huddleston JI. Decreased length of stay after TKA is not associated with increased readmission rates in a national Medicare sample. Clin Orthop Relat Res. 2012;470:166–171.
Xu HF, White RS, Sastow DL, Andreae MH, Gaber-Baylis LK, Turnbull ZA. Medicaid insurance as primary payer predicts increased mortality after total hip replacement in the state inpatient databases of California, Florida and New York. J Clin Anesth. 2017;43:24–32.
Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation (YNHHSC/CORE). Procedure-specific readmission measure updates and specifications report: elective primary total hip arthroplasty (THA) and/or total knee arthroplasty (TKA), version 30. Available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed January 22, 2018.
Zhang W, Lyman S, Boutin-Foster C, Parks ML, Pan T-J, Lan A, et al. Racial and ethnic disparities in utilization rate, hospital volume, and perioperative outcomes after total knee arthroplasty. J Bone Joint Surg Am. 2016;98:1243–1252.
Zmistowski B, Restrepo C, Hess J, Adibi D, Cangoz S, Parvizi J. Unplanned readmission after total joint arthroplasty: rates, reasons, and risk factors. J Bone Joint Surg Am. 2013;95:1869–1876.
Acknowledgements
The authors thank Kara Fields and Yu-fen Chiu for their help with manuscript preparation.
Funding
This study was partially funded by the generous donations of Mr. Glenn Bergenfield, the Sidney Milton and Leoma Simon Foundation, and Mr. and Mrs. David Forber.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Elina Huerfano, MD, Kate Shanaghan, Federico Girardi, Stavros Memtsoudis, MD, and Jiabin Liu, MD, declare that they have no conflicts of interest. Alejandro Gonzalez Della Valle, MD, reports receiving personal fees from OrthoSensor, Ortho Development, LINK, and Intellijoint, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Additional information
Level of Evidence: Level III: retrospective cohort study
Electronic Supplementary Material
Online Resource Fig. 1
Forest plot of musculoskeletal pain in total knee arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 45 kb)
Online Resource Fig. 2
Forest plot of periprosthetic infection/wound infection in total knee arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 39 kb)
Online Resource Fig. 3
Forest plot of cardiac complications excluding acute myocardial infarction in total knee arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 39 kb)
Online Resource Fig. 4
Forest plot of blood transfusions in total knee arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 47 kb)
Online Resource Fig. 5
Forest plot of psychiatric events in total knee arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 36 kb)
Online Resource Fig. 6
Forest plot of deep vein thrombosis in total knee arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 30 kb)
Online Resource Fig. 7
Forest plot of periprosthetic infection / wound infection in total hip arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 38 kb)
Online Resource Fig. 8
Forest plot of blood transfusions in total hip arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 48 kb)
Online Resource Fig. 9
Forest plot of cardiac complications excluding acute myocardial infarction in total hip arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 44 kb)
Online Resource Fig. 10
Forest plot of psychiatric events in total hip arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 29 kb)
Online Resource Fig. 11
Forest plot of mechanical complications in total hip arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 43 kb)
Online Resource Fig. 12
Forest plot of musculoskeletal pain in total hip arthroplasty cohort. Online Resource for “Characterization of Readmission and Emergency Department Visits Within 90 days Following Lower-Extremity Arthroplasty” (PNG 35 kb)
Online Resource Table 1
(DOCX 40 kb)
ESM 1
(PDF 1224 kb)
ESM 2
(PDF 1224 kb)
ESM 3
(PDF 1224 kb)
ESM 4
(PDF 1224 kb)
ESM 5
(PDF 1224 kb)
ESM 6
(PDF 1224 kb)
Rights and permissions
About this article
Cite this article
Huerfano, E., Gonzalez Della Valle, A., Shanaghan, K. et al. Characterization of Re-admission and Emergency Department Visits Within 90 Days Following Lower-Extremity Arthroplasty. HSS Jrnl 14, 271–281 (2018). https://doi.org/10.1007/s11420-018-9622-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-018-9622-8