Abstract
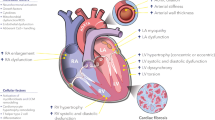
Age-related changes in cardiac homeostasis can be observed at the cellular, extracellular, and tissue levels. Progressive cardiomyocyte hypertrophy, inflammation, and the gradual development of cardiac fibrosis are hallmarks of cardiac aging. In the absence of a secondary insult such as hypertension, these changes are subtle and result in slight to moderate impaired myocardial function, particularly diastolic function. While collagen deposition and cross-linking increase during aging, extracellular matrix (ECM) degradation capacity also increases due to increased expression of matrix metalloproteinases (MMPs). Of the MMPs elevated with cardiac aging, MMP-9 has been extensively evaluated and its roles are reviewed here. In addition to proteolytic activity on ECM components, MMPs oversee cell signaling during the aging process by modulating cytokine, chemokine, growth factor, hormone, and angiogenic factor expression and activity. In association with elevated MMP-9, macrophage numbers increase in an age-dependent manner to regulate the ECM and angiogenic responses. Understanding the complexity of the molecular interactions between MMPs and the ECM in the context of aging may provide novel diagnostic indicators for the early detection of age-related fibrosis and cardiac dysfunction.


Similar content being viewed by others
References
Ahluwalia A, Jones MK, Szabo S, Tarnawski AS (2014) Aging impairs transcriptional regulation of vascular endothelial growth factor in human microvascular endothelial cells: implications for angiogenesis and cell survival. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society 65:209–215
Annoni G et al (1998) Age-dependent expression of fibrosis-related genes and collagen deposition in the rat myocardium. Mech Ageing Dev 101:57–72
Antia M, Baneyx G, Kubow KE, Vogel V (2008) Fibronectin in aging extracellular matrix fibrils is progressively unfolded by cells and elicits an enhanced rigidity response. Faraday Discuss 139:229–249 discussion 309-225, 419-220
Anversa P, Hiler B, Ricci R, Guideri G, Olivetti G (1986) Myocyte cell loss and myocyte hypertrophy in the aging rat heart. J Am Coll Cardiol 8:1441–1448
Anversa P, Palackal T, Sonnenblick EH, Olivetti G, Meggs LG, Capasso JM (1990) Myocyte cell loss and myocyte cellular hyperplasia in the hypertrophied aging rat heart. Circ Res 67:871–885
Anversa P et al (2005) Myocardial aging. Basic Res Cardiol 100:482–493
Asif M et al (2000) An advanced glycation endproduct cross-link breaker can reverse age-related increases in myocardial stiffness. Proc Natl Acad Sci U S A 97:2809–2813
Basso N, Cini R, Pietrelli A, Ferder L, Terragno NA, Inserra F (2007) Protective effect of long-term angiotensin II inhibition. Am J Phys Heart Circ Phys 293:H1351–H1358. doi:10.1152/ajpheart.00393.2007
Biernacka A, Frangogiannis NG (2011) Aging and cardiac fibrosis. Aging and disease 2:158–173
Bildyug NB, Voronkina IV, Smagina LV, Yudintseva NM, Pinaev GP (2015) Matrix metalloproteinases in primary culture of cardiomyocytes. Biochemistry Biokhimiya 80:1318–1326. doi:10.1134/S0006297915100132
Bokov AF, Lindsey ML, Khodr C, Sabia MR, Richardson A (2009) Long-lived Ames dwarf mice are resistant to chemical stressors the journals of gerontology series A. Biological sciences and medical sciences 64:819–827
Bonnema DD et al (2007) Effects of age on plasma matrix metalloproteinases (MMPs) and tissue inhibitor of metalloproteinases (TIMPs). J Card Fail 13:530–540
Bradshaw AD (2009) The role of SPARC in extracellular matrix assembly. Journal of cell communication and signaling 3:239–246. doi:10.1007/s12079-009-0062-6
Bradshaw AD, Baicu CF, Rentz TJ, Van Laer AO, Bonnema DD, Zile MR (2010) Age-dependent alterations in fibrillar collagen content and myocardial diastolic function: role of SPARC in post-synthetic procollagen processing. Am J Phys Heart Circ Phys 298:H614–H622. doi:10.1152/ajpheart.00474.2009
Brandes RP, Fleming I, Busse R (2005) Endothelial aging. Cardiovasc Res 66:286–294. doi:10.1016/j.cardiores.2004.12.027
Bujak M, Kweon HJ, Chatila K, Li N, Taffet G, Frangogiannis NG (2008) Aging-related defects are associated with adverse cardiac remodeling in a mouse model of reperfused myocardial infarction. J Am Coll Cardiol 51:1384–1392
Burgess ML, McCrea JC, Hedrick HL (2001) Age-associated changes in cardiac matrix and integrins. Mech Ageing Dev 122:1739–1756
Burkauskiene A (2005) Age-related changes in the structure of myocardial collagen network of auricle of the right atrium in healthy persons and ischemic heart disease patients. Medicina 41:145–154
Campbell DJ et al (2012) Diastolic dysfunction of aging is independent of myocardial structure but associated with plasma advanced glycation end-product levels. PLoS One 7:e49813. doi:10.1371/journal.pone.0049813
Cauwe B, Martens E, Proost P, Opdenakker G (2009) Multidimensional degradomics identifies systemic autoantigens and intracellular matrix proteins as novel gelatinase B/MMP-9 substrates. Integrative biology : quantitative biosciences from nano to macro 1:404–426
Cauwe B, Opdenakker G (2010) Intracellular substrate cleavage: a novel dimension in the biochemistry, biology and pathology of matrix metalloproteinases. Crit Rev Biochem Mol Biol 45:351–423. doi:10.3109/10409238.2010.501783
Cauwe B, Van den Steen PE, Opdenakker G (2007) The biochemical, biological, and pathological kaleidoscope of cell surface substrates processed by matrix metalloproteinases. Crit Rev Biochem Mol Biol 42:113–185
Chiao YA et al (2011) Multi-analyte profiling reveals matrix metalloproteinase-9 and monocyte chemotactic protein-1 as plasma biomarkers of cardiac aging. Circ Cardiovasc Genet 4:455–462. doi:10.1161/CIRCGENETICS.111.959981
Chiao YA et al (2012) Matrix metalloproteinase-9 deletion attenuates myocardial fibrosis and diastolic dysfunction in ageing mice. Cardiovasc Res 96:444–455. doi:10.1093/cvr/cvs275
Chow AK, Cena J, Schulz R (2007) Acute actions and novel targets of matrix metalloproteinases in the heart and vasculature. Br J Pharmacol 152:189–205. doi:10.1038/sj.bjp.0707344
Dai DF, Rabinovitch PS (2009) Cardiac aging in mice and humans: the role of mitochondrial oxidative stress. Trends in cardiovascular medicine 19:213–220. doi:10.1016/j.tcm.2009.12.004
Dai DF et al (2009) Overexpression of catalase targeted to mitochondria attenuates murine cardiac aging. Circulation 119:2789–2797
de Castro Bras LE, Toba H, Baicu CF, Zile MR, Weintraub ST, Lindsey ML, Bradshaw AD (2014) Age and SPARC change the extracellular matrix composition of the left ventricle. Biomed Res Int 2014:810562. doi:10.1155/2014/810562
Deshmane SL, Kremlev S, Amini S, Sawaya BE (2009) Monocyte chemoattractant protein-1 (MCP-1): an overview. Journal of interferon & cytokine research : the official journal of the International Society for Interferon and Cytokine Research 29:313–326. doi:10.1089/jir.2008.0027
Domenighetti AA, Wang Q, Egger M, Richards SM, Pedrazzini T, Delbridge LM (2005) Angiotensin II-mediated phenotypic cardiomyocyte remodeling leads to age-dependent cardiac dysfunction and failure. Hypertension 46:426–432. doi:10.1161/01.HYP.0000173069.53699.d9
Donato AJ, Eskurza I, Silver AE, Levy AS, Pierce GL, Gates PE, Seals DR (2007) Direct evidence of endothelial oxidative stress with aging in humans: relation to impaired endothelium-dependent dilation and upregulation of nuclear factor-kappaB. Circ Res 100:1659–1666. doi:10.1161/01.RES.0000269183.13937.e8
Eckhard U et al (2016) Active site specificity profiling of the matrix metalloproteinase family: proteomic identification of 4300 cleavage sites by nine MMPs explored with structural and synthetic peptide cleavage analyses matrix biology. Journal of the International Society for Matrix Biology 49:37–60. doi:10.1016/j.matbio.2015.09.003
Egeblad M, Werb Z (2002) New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer 2:161–174. doi:10.1038/nrc745
Eghbali M et al (1989a) Localization of types I, III and IV collagen mRNAs in rat heart cells by in situ hybridization. J Mol Cell Cardiol 21:103–113
Eghbali M, Eghbali M, Robinson TF, Seifter S, Blumenfeld OO (1989b) Collagen accumulation in heart ventricles as a function of growth and aging. Cardiovasc Res 23:723–729
Finkel T (2015) The metabolic regulation of aging. Nat Med 21:1416–1423. doi:10.1038/nm.3998
Flack EC et al (2006) Alterations in cultured myocardial fibroblast function following the development of left ventricular failure. J Mol Cell Cardiol 40:474–483
Franceschi C (2007) Inflammaging as a major characteristic of old people: can it be prevented or cured? Nutr Rev 65:S173–S176
Gazoti Debessa CR, Mesiano Maifrino LB, Rodrigues de Souza R (2001) Age related changes of the collagen network of the human heart. Mech Ageing Dev 122:1049–1058
Graf K et al (1997) Myocardial osteopontin expression is associated with left ventricular hypertrophy. Circulation 96:3063–3071
Gunning JF, Coleman HN 3rd (1973) Myocardial oxygen consumption during experimental hypertrophy and congestive heart failure. J Mol Cell Cardiol 5:25–38
Hartog JW, Voors AA, Bakker SJ, Smit AJ, van Veldhuisen DJ (2007) Advanced glycation end-products (AGEs) and heart failure: pathophysiology and clinical implications. Eur J Heart Fail 9:1146–1155. doi:10.1016/j.ejheart.2007.09.009
Hellstrom M, Johansson B, Engstrom-Laurent A (2006) Hyaluronan and its receptor CD44 in the heart of newborn and adult rats. The anatomical record part A. Discoveries in molecular, cellular, and evolutionary biology 288:587–592. doi:10.1002/ar.a.20332
Herrera MD, Mingorance C, Rodriguez-Rodriguez R, Alvarez de Sotomayor M (2010) Endothelial dysfunction and aging: an update. Ageing Res Rev 9:142–152. doi:10.1016/j.arr.2009.07.002
Horn MA et al (2012) Age-related divergent remodeling of the cardiac extracellular matrix in heart failure: collagen accumulation in the young and loss in the aged. J Mol Cell Cardiol 53:82–90. doi:10.1016/j.yjmcc.2012.03.011
Horn MA, Trafford AW (2016) Aging and the cardiac collagen matrix: novel mediators of fibrotic remodelling. J Mol Cell Cardiol 93:175–185. doi:10.1016/j.yjmcc.2015.11.005
Huet E et al (2015) Deletion of extracellular matrix metalloproteinase inducer/CD147 induces altered cardiac extracellular matrix remodeling in aging mice. Journal of physiology and pharmacology : an official journal of the Polish Physiological Society 66:355–366
Iyer RP, Chiao YA, Flynn ER, Hakala K, Cates CA, Weintraub ST, de Castro Bras LE (2016) Matrix metalloproteinase-9-dependent mechanisms of reduced contractility and increased stiffness in the aging heart. Proteomics Clin Appl 10:92–107. doi:10.1002/prca.201500038
Johnson JL et al (2011) A selective matrix metalloproteinase-12 inhibitor retards atherosclerotic plaque development in apolipoprotein E-knockout mice. Arterioscler Thromb Vasc Biol 31:528–535. doi:10.1161/ATVBAHA.110.219147
Jugdutt BI, Jelani A, Palaniyappan A, Idikio H, Uweira RE, Menon V, Jugdutt CE (2010) Aging-related early changes in markers of ventricular and matrix remodeling after reperfused ST-segment elevation myocardial infarction in the canine model: effect of early therapy with an angiotensin II type 1 receptor blocker. Circulation 122:341–351. doi:10.1161/circulationaha.110.948190
Kajstura J et al (1996) Necrotic and apoptotic myocyte cell death in the aging heart of Fischer 344 rats. Am J Phys 271:H1215–H1228
Kandasamy AD, Chow AK, Ali MAM, Schulz R (2010) Matrix metalloproteinase-2 and myocardial oxidative stress injury: beyond the matrix. Cardiovasc Res 85:413–423. doi:10.1093/cvr/cvp268
Kaplan P et al (2007) Effect of aging on the expression of intracellular Ca(2+) transport proteins in a rat heart. Mol Cell Biochem 301:219–226. doi:10.1007/s11010-007-9414-9
Khan AS, Lynch CD, Sane DC, Willingham MC, Sonntag WE (2001) Growth hormone increases regional coronary blood flow and capillary density in aged rats. The journals of gerontology series A. Biological sciences and medical sciences 56:B364–B371
Khan AS, Sane DC, Wannenburg T, Sonntag WE (2002) Growth hormone, insulin-like growth factor-1 and the aging cardiovascular system. Cardiovasc Res 54:25–35
Kwak HB, Kim JH, Joshi K, Yeh A, Martinez DA, Lawler JM (2011) Exercise training reduces fibrosis and matrix metalloproteinase dysregulation in the aging rat heart. FASEB J 25:1106–1117. doi:10.1096/fj.10-172924
Lakatta EG (1994) Cardiovascular reserve capacity in healthy older humans. Aging (Milano) 6:213–223
Lakatta EG, Levy D (2003) Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: part II: the aging heart in health. Links to Heart Disease Circulation 107:346–354
Lin J, Lopez E, Jin Y, Van Remmen H, Bauch T, Han H, Lindsey M (2008) Age-related cardiac muscle sarcopenia: combining experimental and mathematical modeling to identify mechanisms. Exp Gerontol 43:296–306
Lindsey ML et al (2005) Age-dependent changes in myocardial matrix metalloproteinase/tissue inhibitor of metalloproteinase profiles and fibroblast function. Cardiovasc Res 66:410–419
Lindsey ML, Iyer RP, Jung M, De Leon-Pennell KY, Ma Y (2016) Matrix metalloproteinases as input and output signals for post-myocardial infarction remodeling. J Mol Cell Cardiol 91:134–140. doi:10.1016/j.yjmcc.2015.12.018
Liu J, Finkel T (2014) Aging: the blurry line between life and death. Curr Biol 24:R610–R613. doi:10.1016/j.cub.2014.05.057
Liu J et al (2003) Glycation end-product cross-link breaker reduces collagen and improves cardiac function in aging diabetic heart. Am J Phys Heart Circ Phys 285:H2587–H2591
Luther DJ et al (2012) Absence of type VI collagen paradoxically improves cardiac function, structure, and remodeling after myocardial infarction. Circ Res. doi:10.1161/CIRCRESAHA.111.252734
Ma Y et al (2015) Deriving a cardiac ageing signature to reveal MMP-9-dependent inflammatory signalling in senescence. Cardiovasc Res 106:421–431. doi:10.1093/cvr/cvv128
Ma Y, Chiao YA, Zhang J, Manicone AM, Jin YF, Lindsey ML (2012) Matrix metalloproteinase-28 deletion amplifies inflammatory and extracellular matrix responses to cardiac aging. Microsc Microanal 18:81–90. doi:10.1017/S1431927611012220
Mamuya W, Chobanian A, Brecher P (1992) Age-related changes in fibronectin expression in spontaneously hypertensive. Wistar-Kyoto, and Wistar rat hearts Circulation research 71:1341–1350
Martin-Fernandez B, Gredilla R (2016) Mitochondria and oxidative stress in heart aging Age doi:10.1007/s11357-016-9933-y
Mendes AB, Ferro M, Rodrigues B, Souza MR, Araujo RC, Souza RR (2012) Quantification of left ventricular myocardial collagen system in children, young adults, and the elderly. Medicina (B Aires) 72:216–220
Nahrendorf M (2016) Monocyte and macrophage contributions to cardiac remodeling Journal of molecular and cellular cardiology in press (JMCC9602)
Nguyen NT, Yabluchanskiy A, de Castro Brás LE, Jin Y-F, Lindsey ML (2014) Aging-related changes in extracellular matrix: implications for ventricular remodeling following myocardial infarction
Olivetti G, Melissari M, Capasso JM, Anversa P (1991) Cardiomyopathy of the aging human heart. Myocyte loss and reactive cellular hypertrophy. Circulation research 68:1560–1568
Olivetti G, Ricci R, Anversa P (1987) Hyperplasia of myocyte nuclei in long-term cardiac hypertrophy in rats. J Clin Invest 80:1818–1821. doi:10.1172/JCI113278
Parati G, Frattola A, Di Rienzo M, Castiglioni P, Mancia G (1997) Broadband spectral analysis of blood pressure and heart rate variability in very elderly subjects. Hypertension 30:803–808
Prockop DJ, Kivirikko KI (1995) Collagens: molecular biology, diseases, and potentials for therapy. Annu Rev Biochem 64:403–434. doi:10.1146/annurev.bi.64.070195.002155
Riches K, Morley ME, Turner NA, O'Regan DJ, Ball SG, Peers C, Porter KE (2009) Chronic hypoxia inhibits MMP-2 activation and cellular invasion in human cardiac myofibroblasts. J Mol Cell Cardiol 47:391–399
Rossi S et al (2014) The effect of aging on the specialized conducting system: a telemetry ECG study in rats over a 6 month period. PLoS One 9:e112697. doi:10.1371/journal.pone.0112697
Sack MN, Finkel T (2012) Mitochondrial metabolism, sirtuins, and aging. Cold Spring Harb Perspect Biol:4. doi:10.1101/cshperspect.a013102
Saucerman J (2016) Computational modeling of cardiac fibroblasts and fibrosis. Journal of molecular and cellular cardiology in press (JMCC9598)
Sternlicht M, Werb Z (2001) How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol 17:463–516
Strait JB, Lakatta EG (2012) Aging-associated cardiovascular changes and their relationship to heart failure. Heart failure clinics 8:143–164. doi:10.1016/j.hfc.2011.08.011
Sun N, Youle RJ, Finkel T (2016) The mitochondrial basis of aging. Mol Cell 61:654–666. doi:10.1016/j.molcel.2016.01.028
Swinnen M et al (2009) Absence of thrombospondin-2 causes age-related dilated cardiomyopathy. Circulation 120:1585–1597. doi:10.1161/CIRCULATIONAHA.109.863266
Thomas DP, Cotter TA, Li X, McCormick RJ, Gosselin LE (2001) Exercise training attenuates aging-associated increases in collagen and collagen crosslinking of the left but not the right ventricle in the rat. Eur J Appl Physiol 85:164–169
Thomas DP, McCormick RJ, Zimmerman SD, Vadlamudi RK, Gosselin LE (1992) Aging- and training-induced alterations in collagen characteristics of rat left ventricle and papillary muscle. Am J Phys 263:H778–H783
Thomas DP, Zimmerman SD, Hansen TR, Martin DT, McCormick RJ (2000) Collagen gene expression in rat left ventricle: interactive effect of age and exercise training. J Appl Physiol 89:1462–1468
Toba H, de Castro Bras LE, Baicu CF, Zile MR, Lindsey ML, Bradshaw AD (2015) Secreted protein acidic and rich in cysteine facilitates age-related cardiac inflammation and macrophage M1 polarization. American Journal of Physiology Cell Physiology 308:C972–C982 doi:10.1152/ajpcell.00402.2014
Toba H, de Castro Bras LE, Baicu CF, Zile MR, Lindsey ML, Bradshaw AD (2016) Increased ADAMTS1 mediates SPARC-dependent collagen deposition in the aging myocardium. Am J Phys Endocrinol Metab 310:E1027–E1035. doi:10.1152/ajpendo.00040.2016
Toprak A, Reddy J, Chen W, Srinivasan S, Berenson G (2009) Relation of pulse pressure and arterial stiffness to concentric left ventricular hypertrophy in young men (from the Bogalusa Heart Study). Am J Cardiol 103:978–984. doi:10.1016/j.amjcard.2008.12.011
Toussaint O, Royer V, Salmon M, Remacle J (2002) Stress-induced premature senescence and tissue ageing. Biochem Pharmacol 64:1007–1009
Turner N (2016) Inflammatory and fibrotic responses of cardiac fibroblasts to myocardial damage associated molecular patterns (DAMPs). Journal of molecular and cellular cardiology in press (JMCC9542)
Vanhoutte D, Heymans S (2010) TIMPs and cardiac remodeling: ‘embracing the MMP-independent-side of the family’. J Mol Cell Cardiol 48:445–453
Voorhees AP et al (2015) Building a better infarct: modulation of collagen cross-linking to increase infarct stiffness and reduce left ventricular dilation post-myocardial infarction. J Mol Cell Cardiol 85:229–239. doi:10.1016/j.yjmcc.2015.06.006
Wang M, Shah AM (2015) Age-associated pro-inflammatory remodeling and functional phenotype in the heart and large arteries. J Mol Cell Cardiol 83:101–111. doi:10.1016/j.yjmcc.2015.02.004
Weber KT, Janicki JS, Shroff SG, Pick R, Chen RM, Bashey RI (1988) Collagen remodeling of the pressure-overloaded, hypertrophied nonhuman primate myocardium, Circulation research 62:757–765
Wohlgemuth SE, Calvani R, Marzetti E (2014) The interplay between autophagy and mitochondrial dysfunction in oxidative stress-induced cardiac aging and pathology. J Mol Cell Cardiol 71:62–70. doi:10.1016/j.yjmcc.2014.03.007
Wu JJ et al (2013) Increased mammalian lifespan and a segmental and tissue-specific slowing of aging after genetic reduction of mTOR expression. Cell Rep 4:913–920. doi:10.1016/j.celrep.2013.07.030
Xu D, Finkel T (2002) A role for mitochondria as potential regulators of cellular life span. Biochem Biophys Res Commun 294:245–248. doi:10.1016/S0006-291X(02)00464-3
Yabluchanskiy A et al (2014) Cardiac aging is initiated by matrix metalloproteinase-9-mediated endothelial dysfunction American journal of physiology. Heart and circulatory physiology 306:H1398–H1407. doi:10.1152/ajpheart.00090.2014
Yabluchanskiy A et al (2015) Myocardial infarction superimposed on aging: MMP-9 deletion promotes M2 macrophage polarization. The journals of gerontology series A. Biological sciences and medical sciences. doi:10.1093/gerona/glv034
Yamamoto D, Takai S (2009) Pharmacological implications of MMP-9 inhibition by ACE inhibitors. Curr Med Chem 16:1349–1354
Yamamoto D, Takai S, Jin D, Inagaki S, Tanaka K, Miyazaki M (2007a) Molecular mechanism of imidapril for cardiovascular protection via inhibition of MMP-9. J Mol Cell Cardiol 43:670–676
Yamamoto D, Takai S, Miyazaki M (2007b) Prediction of interaction mode between a typical ACE inhibitor and MMP-9 active site. Biochem Biophys Res Commun 354:981–984
Yang Y et al (2008) Age-related differences in postinfarct left ventricular rupture and remodeling American journal of physiology. Heart and circulatory physiology 294:H1815–H1822. doi:10.1152/ajpheart.00831.2007
Zweier JL, Chen CA, Druhan LJ (2011) S-glutathionylation reshapes our understanding of endothelial nitric oxide synthase uncoupling and nitric oxide/reactive oxygen species-mediated signaling. Antioxid Redox Signal 14:1769–1775. doi:10.1089/ars.2011.3904
Acknowledgements
This work was supported by the National Institute of Health HL075360, HL129823, HL051971, T32HL105324, GM114833, and GM104357 and by the Biomedical Laboratory Research and Development Service of the Veterans Affairs Office of Research and Development Award 5I01BX000505.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Meschiari, C., Ero, O.K., Pan, H. et al. The impact of aging on cardiac extracellular matrix. GeroScience 39, 7–18 (2017). https://doi.org/10.1007/s11357-017-9959-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-017-9959-9