Abstract
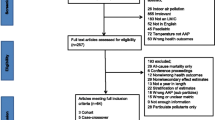
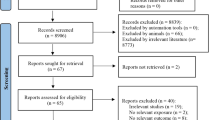
Ambient air pollution is nowadays one of the most crucial contributors to deteriorating health status worldwide. The components of air pollution include PM2.5 and PM10, NO2, SO2, CO, O3, and organic compounds. They are attributed to several health outcomes, for instance, cardiovascular diseases (CVD), respiratory diseases, birth outcomes, neurologic diseases, and psychiatric diseases. The objective of this study is to evaluate the association between different ambient air pollutants and the above-mentioned health outcomes. In this systematic review, a total of 76 articles was ultimately selected from 2653 articles, through multiple screening steps by the aid of a set of exclusion criteria as non-English articles, indoor air pollution assessment, work-related, occupational and home-attributed pollution, animal studies, tobacco smoking effects, letters to editors, commentaries, animal experiments, reviews, case reports and case series, out of 19,862 published articles through a systematic search in PubMed, Web of Science, and Scopus. Then, the associations between air pollution and different health outcomes were measured as relative risks and odds ratios. The association between air pollutants, PM2.5 and PM10, NO2, SO2, CO, O3, and VOC with major organ systems health was investigated through the gathered studies. Relative risks and/or odds ratios attributed to each air pollutant/outcome were ultimately reported. In this study, a thorough and comprehensive discussion of all aspects of the contribution of ambient air pollutants in health outcomes was proposed. To our knowledge up to now, there is no such comprehensive outlook on this issue. Growing concerns in concert with air pollution-induced health risks impose a great danger on the life of billions of people worldwide. Should we propose ideas and schemes to reduce ambient air pollutant, there will be dramatic reductions in the prevalence and occurrence of health-threatening conditions.

Similar content being viewed by others
References
Andersen ZJ, Olsen TS, Andersen KK, Loft S, Ketzel M, Raaschou-Nielsen O (2010) Association between short-term exposure to ultrafine particles and hospital admissions for stroke in Copenhagen, Denmark. Eur Heart J 31(16):2034–2040
Andersen ZJ, Hvidberg M, Jensen SS, Ketzel M, Loft S, Sørensen M, Tjønneland A, Overvad K, Raaschou-Nielsen O (2011) Chronic obstructive pulmonary disease and long-term exposure to traffic-related air pollution: a cohort study. Am J Respir Crit Care Med 183(4):455–461
Andersen ZJ, Bønnelykke K, Hvidberg M, Jensen SS, Ketzel M, Loft S, Sørensen M, Tjønneland A, Overvad K, Raaschou-Nielsen O (2012a) Long-term exposure to air pollution and asthma hospitalisations in older adults: a cohort study. Thorax. 67(1):6–11
Andersen ZJ, Kristiansen LC, Andersen KK, Olsen TS, Hvidberg M, Jensen SS, Ketzel M, Loft S, Sørensen M, Tjønneland A, Overvad K, Raaschou-Nielsen O (2012b) Stroke and long-term exposure to outdoor air pollution from nitrogen dioxide: a cohort study. Stroke. 43(2):320–325
Andersen ZJ, Pedersen M, Weinmayr G, Stafoggia M, Galassi C, Jørgensen JT et al (2017) Long-term exposure to ambient air pollution and incidence of brain tumor: the European Study of Cohorts for Air Pollution Effects (ESCAPE). Neuro-oncology. 20(3):420–432
Anderson JO, Thundiyil JG, Stolbach A (2012) Clearing the air: a review of the effects of particulate matter air pollution on human health. Journal of Medical Toxicology 8(2):166–175
Arbex MA, de Souza Conceição GM, Cendon SP, Arbex FF, Lopes AC, Moysés EP et al (2009) Urban air pollution and chronic obstructive pulmonary disease-related emergency department visits. J Epidemiol Community Health 63(10):777–783
Atkinson RW, Carey IM, Kent AJ, van Staa TP, Anderson HR, Cook DG. Long-term exposure to outdoor air pollution and incidence of cardiovascular diseases. Epidemiology (Cambridge, Mass). 2013 Jan;24(1):44–53
Atkinson R, Kang S, Anderson H, Mills I, Walton H. Epidemiological time series studies of PM2. 5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Thorax. 2014:thoraxjnl-2013-204492
Atkinson R, Carey IM, Kent AJ, Van Staa T, Anderson H, Cook DG (2015) Long-term exposure to outdoor air pollution and the incidence of chronic obstructive pulmonary disease in a national English cohort. Occup Environ Med 72(1):42–48
Ballester F, Saez M, Perez-Hoyos S, Iñiguez C, Gandarillas A, Tobias A et al (2002) The EMECAM project: a multicentre study on air pollution and mortality in Spain: combined results for particulates and for sulfur dioxide. Occup Environ Med 59(5):300–308
Bazyar J, Safarpour H, Daliri S, Karimi A, Keykaleh MS, Bazyar M. The prevalence of sexual violence during pregnancy in Iran and the world: a systematic review and meta-analysis. J Inj Violence Res. 2018 10(2)
Bentayeb M, Wagner V, Stempfelet M, Zins M, Goldberg M, Pascal M, Larrieu S, Beaudeau P, Cassadou S, Eilstein D, Filleul L, le Tertre A, Medina S, Pascal L, Prouvost H, Quénel P, Zeghnoun A, Lefranc A (2015) Association between long-term exposure to air pollution and mortality in France: a 25-year follow-up study. Environ Int 85:5–14
Brunekreef B, Holgate ST (2002) Air pollution and health. Lancet 360(9341):1233–1242
Cao J, Yang C, Li J, Chen R, Chen B, Gu D, Kan H (2011) Association between long-term exposure to outdoor air pollution and mortality in China: a cohort study. J Hazard Mater 186(2–3):1594–1600
Carlos-Wallace FM, Zhang L, Smith MT, Rader G, Steinmaus C (2016) Parental, in utero, and early-life exposure to benzene and the risk of childhood leukemia: a meta-analysis. Am J Epidemiol 183(1):1–14
Chang K-H, Chang M-Y, Muo C-H, Wu T-N, Chen C-Y, Kao C-H (2014) Increased risk of dementia in patients exposed to nitrogen dioxide and carbon monoxide: a population-based retrospective cohort study. PLoS One 9(8):e103078
Chen T-M, Kuschner WG, Gokhale J, Shofer S (2007) Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci 333(4):249–256
Chen G, Song G, Jiang L, Zhang Y, Zhao N, Chen B, Kan H (2008) Short-term effects of ambient gaseous pollutants and particulate matter on daily mortality in Shanghai, China. J Occup Health 50(1):41–47
Chen R, Huang W, Wong C-M, Wang Z, Thach TQ, Chen B, Kan H, CAPES Collaborative Group (2012a) Short-term exposure to sulfur dioxide and daily mortality in 17 Chinese cities: the China air pollution and health effects study (CAPES). Environ Res 118:101–106
Chen R, Samoli E, Wong C-M, Huang W, Wang Z, Chen B, Kan H (2012b) Associations between short-term exposure to nitrogen dioxide and mortality in 17 Chinese cities: the China Air Pollution and Health Effects Study (CAPES). Environ Int 45:32–38
Chen H, Kwong JC, Copes R, Hystad P, van Donkelaar A, Tu K, Brook JR, Goldberg MS, Martin RV, Murray BJ, Wilton AS, Kopp A, Burnett RT (2017) Exposure to ambient air pollution and the incidence of dementia: a population-based cohort study. Environ Int 108:271–277
Chen C, Liu C, Chen R, Wang W, Li W, Kan H et al (2018) Ambient air pollution and daily hospital admissions for mental disorders in Shanghai, China. Science of The Total Environment 613:324–330
Chiusolo M, Cadum E, Stafoggia M, Galassi C, Berti G, Faustini A, Bisanti L, Vigotti MA, Dessì MP, Cernigliaro A, Mallone S, Pacelli B, Minerba S, Simonato L, Forastiere F, on behalf of the EpiAir Collaborative Group (2011) Short-term effects of nitrogen dioxide on mortality and susceptibility factors in 10 Italian cities: the EpiAir study. Environ Health Perspect 119(9):1233–1238
Crouse DL, Peters PA, Villeneuve PJ, Proux M-O, Shin HH, Goldberg MS, Johnson M, Wheeler AJ, Allen RW, Atari DO, Jerrett M, Brauer M, Brook JR, Cakmak S, Burnett RT (2015a) Within-and between-city contrasts in nitrogen dioxide and mortality in 10 Canadian cities; a subset of the Canadian Census Health and Environment Cohort (CanCHEC). Journal of Exposure Science and Environmental Epidemiology 25(5):482–489
Crouse DL, Peters PA, Hystad P, Brook JR, van Donkelaar A, Martin RV, et al. Ambient PM2. 5, O3, and NO2 exposures and associations with mortality over 16 years of follow-up in the Canadian Census Health and Environment Cohort (CanCHEC). Environmental health perspectives. 2015b;123(11):1180
Daliri S, Sayehmiri K, Asadollahi K, Rezaei N, Saroukhani D, Karimi A (2018) Prevalence of congenital anomalies in Iran: a systematic review and meta-analysis. Iranian Journal of Neonatology 9(2):21–32
Díaz J, Arroyo V, Ortiz C, Carmona R, Linares C (2016) Effect of environmental factors on low weight in non-premature births: a time series analysis. PLoS One 11(10):e0164741
Dong G-H, Qian Z, Xaverius PK, Trevathan E, Maalouf S, Parker J et al (2013) Association between long-term air pollution and increased blood pressure and hypertension in China. Hypertension. 61(3):578–584
Estarlich M, Ballester F, Davdand P, Llop S, Esplugues A, Fernández-Somoano A, Lertxundi A, Guxens M, Basterrechea M, Tardón A, Sunyer J, Iñiguez C (2016) Exposure to ambient air pollution during pregnancy and preterm birth: a Spanish multicenter birth cohort study. Environ Res 147:50–58
Feng J, Yang W (2012) Effects of particulate air pollution on cardiovascular health: a population health risk assessment. PLoS One 7(3):e33385
Forastiere F, Stafoggia M, Picciotto S, Bellander T, D’ippoliti D, Lanki T et al (2005) A case-crossover analysis of out-of-hospital coronary deaths and air pollution in Rome, Italy. Am J Respir Crit Care Med 172(12):1549–1555
Galan I, Tobias A, Banegas J, Aranguez E (2003) Short-term effects of air pollution on daily asthma emergency room admissions. Eur Respir J 22(5):802–808
Gehring U, Van Eijsden M, Dijkema MB, Van der Wal MF, Fischer P, Brunekreef B (2011a) Traffic-related air pollution and pregnancy outcomes in the Dutch ABCD birth cohort study. Occup Environ Med 68(1):36–43
Gehring U, Wijga AH, Fischer P, de Jongste JC, Kerkhof M, Koppelman GH, Smit HA, Brunekreef B Traffic-related air pollution, preterm birth and term birth weight in the PIAMA birth cohort study. Environ Res 2011b;111(1):125–135
Gu Y, Lin H, Liu T, Xiao J, Zeng W, Li Z, Lv X, Ma W (2017) The interaction between ambient PM10 and NO2 on mortality in Guangzhou, China. Int J Environ Res Public Health 14(11):1381
Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet (London, England). 2014 May 3;383(9928):1581–92
Guo Y, Tong S, Zhang Y, Barnett AG, Jia Y, Pan X (2010) The relationship between particulate air pollution and emergency hospital visits for hypertension in Beijing, China. Sci Total Environ 408(20):4446–4450
Guo P, Wang Y, Feng W, Wu J, Fu C, Deng H, Huang J, Wang L, Zheng M, Liu H (2017) Ambient air pollution and risk for ischemic stroke: a short-term exposure assessment in South China. Int J Environ Res Public Health 14(9):1091
Hansell A, Ghosh RE, Blangiardo M, Perkins C, Vienneau D, Goffe K, Briggs D, Gulliver J (2016) Historic air pollution exposure and long-term mortality risks in England and Wales: prospective longitudinal cohort study. Thorax. 71(4):330–338
Heinrich J, Thiering E, Rzehak P, Krämer U, Hochadel M, Rauchfuss KM, Gehring U, Wichmann HE (2013) Long-term exposure to NO2 and PM10 and all-cause and cause-specific mortality in a prospective cohort of women. Occup Environ Med 70(3):179–186
Henrotin J, Besancenot J, Bejot Y, Giroud M (2007) Short-term effects of ozone air pollution on ischaemic stroke occurrence: a case-crossover analysis from a 10-year population-based study in Dijon, France. Occup Environ Med 64(7):439–445
Heydarpour P, Amini H, Khoshkish S, Seidkhani H, Sahraian MA, Yunesian M (2014) Potential impact of air pollution on multiple sclerosis in Tehran, Iran. Neuroepidemiology 43(3–4):233–238
Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef B, Kaufman JD (2013) Long-term air pollution exposure and cardio-respiratory mortality: a review. Environ Health 12(1):43
Hystad P, Demers PA, Johnson KC, Brook J, van Donkelaar A, Lamsal L, Martin R, Brauer M (2012) Spatiotemporal air pollution exposure assessment for a Canadian population-based lung cancer case-control study. Environ Health 11(1):22
Hystad P, Villeneuve PJ, Goldberg MS, Crouse DL, Johnson K, Group CCRER (2015) Exposure to traffic-related air pollution and the risk of developing breast cancer among women in eight Canadian provinces: a case–control study. Environ Int 74:240–248
IARC. Some non-heterocyclic polycyclic aromatic hydrocarbons and some related exposures. IARC Monogr Eval Carcinog Risks Hum. 2010;92:1–853
International Agency for Research on Cancer (2015) Outdoor air pollution. IARC monographs. World Health Organization International Agency for Research on Cancer, France, pp 1–449
International Agency for Research on Cancer Monograph Working Group, IARC. 2014 Diesel and gasoline engine exhaust and some nitroarenes. IARC ;105
Ito K, Mathes R, Ross Z, Nádas A, Thurston G, Matte T (2010) Fine particulate matter constituents associated with cardiovascular hospitalizations and mortality in New York City. Environ Health Perspect 119(4):467–473
Jacquemin B, Siroux V, Sanchez M, Carsin A-E, Schikowski T, Adam M, Bellisario V, Buschka A, Bono R, Brunekreef B, Cai Y, Cirach M, Clavel-Chapelon F, Declercq C, de Marco R, de Nazelle A, Ducret-Stich RE, Ferretti VV, Gerbase MW, Hardy R, Heinrich J, Janson C, Jarvis D, al Kanaani Z, Keidel D, Kuh D, le Moual N, Nieuwenhuijsen MJ, Marcon A, Modig L, Pin I, Rochat T, Schindler C, Sugiri D, Stempfelet M, Temam S, Tsai MY, Varraso R, Vienneau D, Vierkötter A, Hansell AL, Krämer U, Probst-Hensch NM, Sunyer J, Künzli N, Kauffmann F (2015) Ambient air pollution and adult asthma incidence in six European cohorts (ESCAPE). Environ Health Perspect 123(6):613–621
Johnson S, Bobb JF, Ito K, Savitz DA, Elston B, Shmool JL et al (2016) Ambient fine particulate matter, nitrogen dioxide, and preterm birth in New York City. Environ Health Perspect 124(8):1283–1290
Jørgensena JT, Johansena MS, Ravnskjærb L, Andersenb KK, Bräunercd EV, Lofta S et al (2016) Long-term exposure to ambient air pollution and incidence of brain tumours: the Danish Nurse Cohort. Neurotoxicology. 55:122–130
Jung C-R, Lin Y-T, Hwang B-F (2013) Air pollution and newly diagnostic autism spectrum disorders: a population-based cohort study in Taiwan. PLoS One 8(9):e75510
Kachuri L, Villeneuve PJ, Parent M-É, Johnson KC. Workplace exposure to diesel and gasoline engine exhausts and the risk of colorectal cancer in Canadian men. Environmental Health. 2016;15(4)
Khaniabadi YO, Daryanoosh SM, Hopke PK, Ferrante M, De Marco A, Sicard P et al (2017) Acute myocardial infarction and COPD attributed to ambient SO2 in Iran. Environ Res 156:683–687
Korek MJ, Bellander TD, Lind T, Bottai M, Eneroth KM, Caracciolo B, de Faire UH, Fratiglioni L, Hilding A, Leander K, Magnusson PKE, Pedersen NL, Östenson CG, Pershagen G, Penell JC (2015) Traffic-related air pollution exposure and incidence of stroke in four cohorts from Stockholm. Journal of Exposure Science and Environmental Epidemiology. 25(5):517–523
Krewski D. Evaluating the effects of ambient air pollution on life expectancy. Mass Medical Soc; 2009
Liawa Y-P, Ting T-F, Ho K-K, Yang C-F (2008) Cell type specificity of lung cancer associated with air pollution. Sci Total Environ 395:23–27
Liu H, Tian Y, Xu Y, Huang Z, Huang C, Hu Y, Zhang J (2017) Association between ambient air pollution and hospitalization for ischemic and hemorrhagic stroke in China: a multicity case-crossover study. Environ Pollut 230:234–241
Loomis D, Grosse Y, Lauby-Secretan B (2013) The carcinogenicity of outdoor air pollution. Lancet Oncol 14:1262–1263
Madsen C, Gehring U, Walker SE, Brunekreef B, Stigum H, Næss Ø et al (2010) Ambient air pollution exposure, residential mobility and term birth weight in Oslo, Norway. Environmental Research 110(4):363–371
Mahalingaiaha S, Hart JE, Laden F, Terryd KL, Boynton-Jarrettg R, Aschengrauh A et al (2014) Adult air pollution exposure and risk of uterine leiomyoma in the nurses’ health study II. Epidemiology. 25(5):682–688
Mannucci PM, Harari S, Martinelli I, Franchini M (2015 Sep) Effects on health of air pollution: a narrative review. Intern Emerg Med 10(6):657–662
Milojevic A, Wilkinson P, Armstrong B, Bhaskaran K, Smeeth L, Hajat S.(2014) Short-term effects of air pollution on a range of cardiovascular events in England and Wales: case-crossover analysis of the MINAP database, hospital admissions and mortality. Heart.heartjnl-2013-304963
Nafstad P, Håheim L, Oftedal B, Gram F, Holme I, Hjermann I, Leren P (2003) Lung cancer and air pollution: a 27 year follow up of 16 209 Norwegian men. Thorax. 58(12):1071–1076
Nafstad P, Håheim LL, Wisløff T, Gram F, Oftedal B, Holme I, Hjermann I, Leren P (2004) Urban air pollution and mortality in a cohort of Norwegian men. Environ Health Perspect 112(5):610–615
Nagel G, Stafoggia M, Pedersen M, Andersen ZJ, Galassi C, Munkenast J et al (2018) Air pollution and incidence of cancers of the stomach and the upper aerodigestive tract in the European Study of Cohorts for Air Pollution Effects (ESCAPE). Int J Cancer 1:1–24
Nascimento LFC, Francisco JB, Patto MBR, Antunes AM (2012) Environmental pollutants and stroke-related hospital admissions. Cadernos de saude publica 28(7):1319–1324
Newby D, Mannucci P, Tell G, Baccarelli A, Brook R (2015) Expert position paper on air pollution and cardiovascular disease. EurHeart J 36(2):83–93
Ngoc LTN, Park D, Lee Y, Lee Y-C (2017) Systematic review and meta-analysis of human skin diseases due to particulate matter. Int J Environ Res Public Health 14:1458
Oftedal B, Nafstad P, Magnus P, Bjørkly S, Skrondal A (2003) Traffic related air pollution and acute hospital admission for respiratory diseases in Drammen, Norway 1995–2000. Eur J Epidemiol 18:671–675
Okona-Mensah K, Battershill J, Boobis A, Fielder R (2005) An approach to investigating the importance of high potency polycyclic aromatic hydrocarbons (PAHs) in the induction of lung cancer by air pollution. Food Chem Toxicol 43:1103–1116
Omori T, Fujimoto G, Yoshimura I, Nitta H, Ono M (2003) Original article effects of particulate matter on daily mortality in 13 Japanese cities. Journal of epidemiology 13(6):314–322
organization wh.2018 Burden of disease from ambient air pollution for 2016. wwwhoint/airpollution/ambient.
Pedersen M, Giorgis-Allemand L, Bernard C, Aguilera I, Andersen A, Ballester F, et al. Ambient air pollution and low birthweight: a European cohort study (ESCAPE) Lancet Respir Med. 2013; 1 (9): 695–704. doi: 10.1016. S2213-2600 (13).70192-9.
Peel JL, Metzger KB, Klein M, Flanders WD, Mulholland JA, Tolbert PE (2006) Ambient air pollution and cardiovascular emergency department visits in potentially sensitive groups. Am J Epidemiol 165(6):625–633
Pereira G, Evans KA, Rich DQ, Bracken MB, Bell ML (2016) Fine particulates, preterm birth, and membrane rupture in Rochester. NY Epidemiology 27(1):66–73
Poulsen AH, Sørensen M, Andersen ZJ, Ketzel M, Raaschou-Nielsen O (2016) Air pollution from traffic and risk for brain tumors: a nationwide study in Denmark. Cancer Causes Control 27(4):473–480
Qian Z, He Q, Lin H-M, Kong L, Liao D, Yang N, Bentley CM, Xu S (2007) Short-term effects of gaseous pollutants on cause-specific mortality in Wuhan, China. J Air Waste Manage Assoc 57(7):785–793
Qian Z, Liang S, Yang S, Trevathan E, Huang Z, Yang R, Wang J, Hu K, Zhang Y, Vaughn M, Shen L, Liu W, Li P, Ward P, Yang L, Zhang W, Chen W, Dong G, Zheng T, Xu S, Zhang B (2016) Ambient air pollution and preterm birth: a prospective birth cohort study in Wuhan, China. Int J Hyg Environ Health 219(2):195–203
Raaschou-Nielsen O, Andersen ZJ, Hvidberg M, Jensen SS, Ketzel M, Sørensen M, Hansen J, Loft S, Overvad K, Tjønneland A (2011) Air pollution from traffic and cancer incidence: a Danish cohort study. Environ Health 10(1):67
Raaschou-Nielsen O, Andersen ZJ, Jensen SS, Ketzel M, Sørensen M, Hansen J, Loft S, Tjønneland A, Overvad K (2012) Traffic air pollution and mortality from cardiovascular disease and all causes: a Danish cohort study. Environ Health 11(1):60
Raaschou-Nielsen O, Andersen ZJ, Beelen R, Samoli E, Stafoggia M, Weinmayr G, Hoffmann B, Fischer P, Nieuwenhuijsen MJ, Brunekreef B, Xun WW, Katsouyanni K, Dimakopoulou K, Sommar J, Forsberg B, Modig L, Oudin A, Oftedal B, Schwarze PE, Nafstad P, de Faire U, Pedersen NL, Östenson CG, Fratiglioni L, Penell J, Korek M, Pershagen G, Eriksen KT, Sørensen M, Tjønneland A, Ellermann T, Eeftens M, Peeters PH, Meliefste K, Wang M, Bueno-de-Mesquita B, Key TJ, de Hoogh K, Concin H, Nagel G, Vilier A, Grioni S, Krogh V, Tsai MY, Ricceri F, Sacerdote C, Galassi C, Migliore E, Ranzi A, Cesaroni G, Badaloni C, Forastiere F, Tamayo I, Amiano P, Dorronsoro M, Trichopoulou A, Bamia C, Vineis P, Hoek G (2013) Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). The lancet oncology 14(9):813–822
Ritz B, Lee P-C, Hansen J, Lassen CF, Ketzel M, Sørensen M, Raaschou-Nielsen O (2015) Traffic-related air pollution and Parkinson’s disease in Denmark: a case–control study. Environ Health Perspect 124(3):351–356
Ruidavets J-B, Cournot M, Cassadou S, Giroux M, Meybeck M, Ferrières J (2005) Ozone air pollution is associated with acute myocardial infarction. Circulation. 111(5):563–569
Savitz DA, Bobb JF, Carr JL, Clougherty JE, Dominici F, Elston B, Ito K, Ross Z, Yee M, Matte TD. Ambient fine particulate matter, nitrogen dioxide, and term birth weight in New York, New York. American journal of epidemiology. 2013;179(4):457–66.
Seo JH, Leem JH, Ha EH, Kim OJ, Kim BM, Lee JY, Park HS, Kim HC, Hong YC, Kim YJ (2010) Population-attributable risk of low birthweight related to PM10 pollution in seven Korean cities. Paediatr Perinat Epidemiol 24(2):140–148
Shah PS, Balkhair T (2011) Air pollution and birth outcomes: a systematic review. Environ Int 37(2):498–516
Shah AS, Langrish JP, Nair H, McAllister DA, Hunter AL, Donaldson K et al (2013) Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet 382(9897):1039–1048
Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W et al (2015) Short term exposure to air pollution and stroke: systematic review and meta-analysis. bmj 350:h1295
Silverman RA, Ito K, Freese J, Kaufman BJ, De Claro D, Braun J et al (2010) Association of ambient fine particles with out-of-hospital cardiac arrests in New York City. Am J Epidemiol 172(8):917–923
Song Q, Christiani DC, Ren J (2014) The global contribution of outdoor air pollution to the incidence, prevalence, mortality and hospital admission for chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Environ Res Public Health 11(11):11822–11832
Stieb DM, LiChen, Eshoul M, StanJudek. Ambient air pollution, birth weight and preterm birth: a systematic review and meta-analysis. Environ Res 2012;117:100–111
STRAIF K, COHEN A, Samet J (2013) Air pollution and cancer. International Agency for Research on Cancer 150:1–17
Su C, Breitner S, Schneider A, Liu L, Franck U, Peters A, Pan X (2016) Short-term effects of fine particulate air pollution on cardiovascular hospital emergency room visits: a time-series study in Beijing, China. Int Arch Occup Environ Health 89(4):641–657
Szyszkowicz M (2007) Air pollution and emergency department visits for ischemic heart disease in Montreal, Canada. Int J Occup Med Environ Health 20(2):167–174
White A, Bradshaw P, Hamra G (2018) Air pollution and breast cancer: a review. Curr Epidemiol Rep 5(2):92–100
Yorifuji T, Kashima S, Doi H (2015) Outdoor air pollution and term low birth weight in Japan. Environ Int 74:106–111
Zanobetti A, Schwartz J (2006) Air pollution and emergency admissions in Boston, MA. J Epidemiol Community Health 60(10):890–895
Zhao Y, Wang S, Aunan K, Seip HM, Hao J (2006) Air pollution and lung cancer risks in China—a meta-analysis. Sci Total Environ 366:500–513
Zheng Z, Xu X, Zhang X, Wang A, Zhang C, Hüttemann M, Grossman LI, Chen LC, Rajagopalan S, Sun Q, Zhang K (2013) Exposure to ambient particulate matter induces a NASH-like phenotype and impairs hepatic glucose metabolism in an animal model. J Hepatol 58:148–154
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible editor: Philippe Garrigues
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bazyar, J., Pourvakhshoori, N., Khankeh, H. et al. A comprehensive evaluation of the association between ambient air pollution and adverse health outcomes of major organ systems: a systematic review with a worldwide approach. Environ Sci Pollut Res 26, 12648–12661 (2019). https://doi.org/10.1007/s11356-019-04874-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-019-04874-z