Abstract
Introduction
Obstructive sleep apnea syndrome (OSAS) is a common form of sleep-related respiratory disease characterized by recurrent blockages in the upper airway. Rapid eye movement (REM)-related OSAS is a condition in which apneas and hypopneas are more common during REM sleep. We investigated whether there was any difference between REM-related mild OSAS group and NREM-related mild OSAS group in terms of anxiety, depression, and daytime sleepiness.
Methods
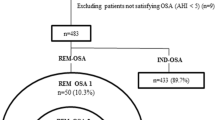
A total of 166 patients with mild OSAS (72 patients with REM-related and 94 NREM-related OSAS) participated in the study. Hospital Anxiety-Depression Scale (HADS) and Epworth Sleepiness Scale (ESS) questionnaires were completed by both groups.
Results
Anxiety and depression scores were significantly higher in patients with REM-related OSAS in comparison to the NREM-related OSAS group (p = 0.01, p = 0.02 respectively). There was no statistically significant difference between the two groups in terms of ESS scores (p = 0.60).
Conclusion
The results of our study suggest that patients with REM-related OSAS have higher rates of depression and anxiety compared to non-REM-related OSAS patients and this may adversely affect quality of life. It may be possible to prevent psychiatric complications, such as depression and anxiety, by administering treatments that reduce REM sleep duration and intensity in patients with REM-related OSAS.
Similar content being viewed by others
References
Haba-Rubio J, Janssens JP, Rochat T, Sforza E (2005) Rapid eye movement related disordered breathing: clinical and polysomnographic features. Chest 128:3350–3357
Koo BB, Dostal J, Ioachimescu O, Budur K (2008) The effects of gender and age on REM-related sleep-disordered breathing. Sleep Breath 12:259–264
Mohleksi B, Finn LA, Hagen EW, Young T, Hla KM, Van Cauter E, Peppard PE (2014) Obstructive sleep apnea during REM sleep and hypertension. Results of the Wisconsin SleepCohort. Am J Respir Crit Care Med 190(10):1158–1167
Mohleksi B, Punjabi NM (2012) “REM-related” obstructive sleep apnea: an epiphenomenon or a clinically important entity? Sleep 35(1):5–7
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J Clin Sleep Med 8(5):597–619
Thombs BD, Benedetti A, Kloda LA, Levis B, Azar M, Riehm KE, Saadat N, Cuijpers P, Gilbody S, Ioannidis JP, McMillan D, Patten SB, Shrier I, Steele RJ, Ziegelstein RC, Loiselle CG, Henry M, Ismail Z, Mitchell N, Tonelli M (2016) Diagnostic accuracy of the Depression subscale of the Hospital Anxiety and Depression Scale (HADS-D) for detecting major depression: protocol for a systematic review and individual patient data meta-analyses. BMJ Open 6(4):e011913
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Krachman SL, D’Alonzo GE, Criner GJ (1995) Sleep in the intensive care unit. Chest 107:1713–1720
Masahiko K, Bradley G et al (2000) Effects of sleep deprivation on neural circulatory control. Hypertension 35:1173–1175
Oksenberg A, Arons E, Nasser K, Vander T, Radwan H (2010) REM related obstructive sleep apnea: the effect of body position. J Clin Sleep Med 6:343–348
Sakao S, Sakurai T, Yahaba M, Sakurai Y, Terada J, Tanabe N, Tatsumi K (2015) Features of REM-related sleep disordered breathing in the Japanese population. Intern Med 54(12):1481–1487
Pamidi S1, Knutson KL, Ghods F, Mokhlesi B (2011) Depressive symptoms and obesity as predictors of sleepiness and quality of life in patients with REM-related obstructive sleep apnea: cross-sectional analysis of a large clinical population. Sleep Med 12(9):827–831
Lee SA, Paek JH, Han SH (2016) REM-related sleep disordered breathing is associated with depressive symptoms in men but not in women. Sleep Breath 20(3):995–1002
Gupta MA, Simpson FC (2015) Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med 11(2):165–175
Gresham SC, Agnew HW Jr, Williams RL (1965) The sleep of depressed patients. An EEG and eye movement study. Arch Gen Psychiatry 13(6):503–507
Armitage R (2007) Sleep and circadian rhythms in mood disorders. Acta Psychiatr Scand Suppl; (433) 115:104–115
Reynolds CF 3rd, Kupfer DJ (1987) Sleep research in affective illness: state of the art circa. Sleep 10(3):199–215
Staner L, Kerkhofs M, Detroux D, Leyman S, Linkowski P, Mendlewicz J (1995) Acute, subchronic and withdrawal sleep EEG changes during treatment with paroxetine and amitriptyline: a double-blind randomized trial in major depression. Sleep 18(6):470–477
Kraiczi H, Hedner J, Dahlöf P, Ejnell H, Carlson J (1999) Effect of serotonin uptake inhibition on breathing during sleep and daytime symptoms in obstructive sleep apnea. Sleep 22(1):61–67
Zhang B, Jia F, Li X, Tang Y, Zheng H, Liu W (2015) Effect of sertraline on breathing in depressed patients without moderate-to-severe sleep-related breathing disorders. Sleep Breath 19:1377–1386
Prasad B, Radulovacki M, Olopade C, Herdegen JJ, Logan T, Carley DW (2010) Prospective trial of efficacy and safety of ondansetron and fluoxetine in patients with obstructive sleep apnea syndrome. Sleep 33:982–989
Luthringer R, Toussaint M, Schaltenbrand N et al (1996) A double-blind, placebo-controlled evaluation of the effects of orally administered venlafaxine on sleep in inpatients with major depression. Psychopharmacol Bull 32:637–646
Thase ME (1998) Depression, sleep, and antidepressants. J Clin Psychiatry 59(Suppl 4):55–65
Chami HA, Baldwin CM, Silverman A, Zhang Y, Rapoport D, Punjabi NM, Gottlieb DJ (2010) Sleepiness, quality of life, and sleep maintenance in REM versus non-REM sleep-disordered breathing. Am J Respir Crit Care Med 181(9):997–1002
Liu Y, Su C, Liu R, Lei G, Zhang W, Yang T, Miao J, Li Z (2011) NREM-AHI greater than REM-AHI versus REM-AHI greater than NREMAHI in patients with obstructive sleep apnea: clinical and polisomnographic features. Sleep Breath 15:463–470
Nykamp K, Rosenthal L, Folkerts M, Roehrs T, Guido P, Roth T (1998) The effect of REM sleep deprivation on the level of sleepiness/alertness. Sleep 21:609–614
İtil O (2016) Uykuda kardiak kayıtlama ve skorlama. J Turk Sleep Med 3(1):29–29
Al Oweidat K, AlRyalat SA, Al-Essa M, Obeidat N (2018) Comparing REM- and NREM-related obstructive sleep apnea in Jordan: a cross-sectional study. Can Respir J 12:9270329
Zinchuk A, Edwards BA, Jeon S, Koo BB, Concato J, Sands S, Wellman A, Yaggi HK (2018) Prevalence, associated clinical features, and impact on continuous positive airway pressure use of a low respiratory arousal threshold among male United States veterans with obstructive sleep apnea. J Clin Sleep Med 14(5):809–817
Gray EL, McKenzie DK, Eckert DJ (2017) Obstructive sleep apnea without obesity is common and difficult to treat: evidence for a distinct pathophysiological phenotype. J Clin Sleep Med 13(2):81–88
Eckert DJ, Younes MK (2014) Arousal from sleep: implications for obstructive sleep apnea pathogenesis and treatment. J Appl Physiol 116(3):302–313
Edwards BA, Eckert DJ, McSharry DG et al (2014) Clinical predictors of the respiratory arousal threshold in patients with obstructive sleep apnea. Am J Respir Crit Care Med 190(11):1293–1300
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The institutional review board (IRB) approved the research methodology.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Geckil, A.A., Ermis, H. The relationship between anxiety, depression, daytime sleepiness in the REM-related mild OSAS and the NREM-related mild OSAS. Sleep Breath 24, 71–75 (2020). https://doi.org/10.1007/s11325-019-01838-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01838-y