Abstract
Aim
To clarify whether unmasking of central sleep apnea during continuous positive airway pressure (CPAP) initiation can be identified from initial diagnostic polysomnography (PSG) in patients with heart failure with reduced ejection fraction (HFREF) and obstructive sleep apnea (OSA)
Materials and methods
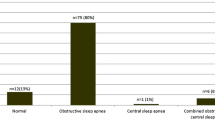
Forty-three consecutive patients with obstructive sleep apnea and central sleep apnea (OSA/CSA) in HFREF were matched with 43 HFREF patients with OSA and successful CPAP initiation. Obstructive apneas during diagnostic PSG were then analyzed for cycle length (CL), ventilation length (VL), apnea length (AL), time to peak ventilation (TTPV), and circulatory delay (CD). We calculated duty ratio (DR) as the ratio of VL/CL and mathematic loop gain (LG).
Results
While AL was similar, CL, VL, TTPV, CD, and DR was significantly longer in patients with OSA/CSA compared to those with OSA, and LG was significantly higher. Receiver operator curves identified optimal cutoff values of 50.2 s for CL (area under the curve (AUC) 0.85, 29.2 s for VL (AUC 0.92), 11.5 s for TTPV (AUC 0.82), 26.4 s for CD (AUC 0.79), and 3.96 (AUC 0.78)) respectively for LG to identify OSA/CSA.
Conclusion
OSA/CSA in HFREF can be identified by longer CL, VL, TTPV, and CD from obstructive events in initial diagnostic PSG. The underlying mechanisms seem to be the presence of an increased LG.


Similar content being viewed by others
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 37:2129–2200
Arzt M, Woehrle H, Oldenburg O, Graml A, Suling A, Erdmann E, Teschler H, Wegscheider K, SchlaHF Investigators (2016) Prevalence and predictors of sleep-disordered breathing in patients with stable chronic heart failure: the SchlaHF registry. JACC Heart Fail 4:116–125
Oldenburg O, Lamp B, Faber L, Teschler H, Horstkotte D, Töpfer V (2007) Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 9:251–257
Levy P, Ryan S, Oldenburg O, Parati G (2013) Sleep apnoea and the heart. Eur Respir Rev 22:333–352
Oldenburg O, Wellmann B, Buchholz A, Bitter T, Fox H, Thiem U, Horstkotte D, Wegscheider K (2016) Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur Heart J 37:1695–1703
Bitter T, Westerheide N, Prinz C, Hossain MS, Vogt J, Langer C, Horstkotte D, Oldenburg O (2011) Cheyne-Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Eur Heart J 32:61–74
Kasai T, Narui K, Dohi T, Yanagisawa N, Ishiwata S, Ohno M, Yamaguchi T, Momomura SI (2008) Prognosis of patients with heart failure and obstructive sleep apnea treated with continuous positive airway pressure. Chest 133:690–696
Randerath WJ, Nothofer G, Priegnitz C, Anduleit N, Treml M, Kehl V, Galetke W (2012) Long-term auto-servoventilation or constant positive pressure in heart failure and coexisting central with obstructive sleep apnea. Chest 142:440–447
Bitter T, Westerheide N, Hossain MS, Lehmann R, Prinz C, Kleemeyer A, Horstkotte D, Oldenburg O (2011) Complex sleep apnoea in congestive heart failure. Thorax 66:402–407
Wedewardt J, Bitter T, Prinz C, Faber L, Horstkotte D, Oldenburg O (2010) Cheyne-Stokes respiration in heart failure: cycle length is dependent on left ventricular ejection fraction. Sleep Med 11:137–142
Efken C, Bitter T, Prib N, Horstkotte D, Oldenburg O (2013) Obstructive sleep apnoea: longer respiratory event lengths in patients with heart failure. Eur Respir J 41:1340–1346
Sands SA, Edwards BA, Kee K, Turton A, Skuza EM, Roebuck T, O'Driscoll DM, Hamilton GS, Naughton MT, Berger PJ (2011) Loop gain as a means to predict a positive airway pressure suppression of Cheyne-Stokes respiration in patients with heart failure. Am J Respir Crit Care Med 184:1067–1075
Randerath W, Verbraecken J, Andreas S, Arzt M, Bloch KE, Brack T, Buyse B, de Backer W, Eckert DJ, Grote L, Hagmeyer L, Hedner J, Jennum P, la Rovere MT, Miltz C, McNicholas WT, Montserrat J, Naughton M, Pepin JL, Pevernagie D, Sanner B, Testelmans D, Tonia T, Vrijsen B, Wijkstra P, Levy P (2017) Definition, discrimination, diagnosis and treatment of central breathing disturbances during sleep. Eur Respir J 49:1600959
Mayer G et al (2017) S3-Leitlinie Nicht erholsamer Schlaf/Schlafstörungen–Kapitel “Schlafbezogene Atmungsstörungen”. Somnologie 20:597–S180
Mayer G, Rodenbeck A, Geisler P, Schulz H (2015) International classification of sleep disorders: overview of the changes in ICSD-3. Somnologie 19:116–125
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep Medicine (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. J Clin Sleep Med 8:597–619
Stanchina M, Robinson K, Corrao W, Donat W, Sands S, Malhotra A (2015) Clinical use of loop gain measures to determine continuous positive airway pressure efficacy in patients with complex sleep apnea: a pilot study. Ann Am Thorac Soc 12:1351–1357
Oldenburg O (2012) Cheyne-Stokes respiration in chronic heart failure. Circ J 76:2305–2317
Hall M et al (1996) Cycle length of periodic breathing in patients with and without heart failure. Am J Respir Crit Care Med 154:376–381
Solin P, Roebuck T, Swieca J, Walters E, Naughton M (1998) Effects of cardiac dysfunction on non-hypercapnic central sleep apnea. Chest 113:104–110
Ryan C, Bradley T (2005) Periodicity of obstructive sleep apnea in patients with and without heart failure. Chest 127:536–542
Oldenburg O, Bitter T, Wiemer M, Langer C, Horstkotte D, Piper C (2009) Pulmonary capillary wedge pressure and pulmonary arterial pressure in heart failure patients with sleep-disordered breathing. Sleep Med 10:726–730
Agostoni P (2008) Mechanisms of periodic breathing during exercise in patients with chronic heart failure<xref rid=‘AFF1’>*</xref>. Chest J 133:197–203
Rubin A, Gottlieb S, Gold A, Schwartz A, Smith P (2004) The role of feedback delay in periodic breathing. Thorax 59:174–177
Churchill E, Cope O, Churchill E, Cope O (1929) The rapid shallow breathing resulting from pulmonary congestion and edema. ( From the Surgical Laboratories, Massachusetts General Host ~ tal, Boston.) ( Received for publication, December 12, 1928.) Experimental studies by Dunn ( 1 ) demonstrated. J Exp Med 49:531–537
Solin P, Bergin P, Richardson M, Kaye DM, Walters EH, Naughton MT (1999) Influence of pulmonary capillary wedge pressure on central apnea in heart failure. Circulation 99:1574–1579
Yiu KH et al (2008) Alleviation of pulmonary hypertension by cardiac resynchronization therapy is associated with improvement in central sleep apnea. Pacing Clin Electrophysiol 31:1522–1527
Dernaika T, Tawk M, Nazir S, Younis W, Kinasewitz GT (2007) Pressure-related central sleep apnea the significance and outcome of continuous positive airway pressure-related central sleep apnea during split-night sleep studies. Chest 132:81–87
Javaheri S, Smith J, Chung E (2009) The prevalence and natural history of complex sleep apnea. J Clin Sleep Med 5:205–211
Liu D, Armitstead J, Benjafield A, Shao S, Malhotra A, Cistulli PA, Pepin JL, Woehrle H (2017) Trajectories of emergent central sleep apnea during CPAP therapy. Chest 152:751–760
Morgenthaler TI, Kuzniar TJ, Wolfe LF, Willes L, McLain WC III, Goldberg R (2014) The complex sleep apnea resolution study: a prospective randomized controlled trial of continuous positive airway pressure versus adaptive servoventilation therapy. Sleep 37:927–934
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Ethical Review Board of the Ruhr University, Bochum, and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Conflict of interest
Olaf Oldenburg reports personal fees from ResMed, personal fees from LivaNova, personal fees from Novartis, and personal fees from Bayer, outside the submitted work. The other authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Bitter, T., Özdemir, B., Fox, H. et al. Cycle length identifies obstructive sleep apnea and central sleep apnea in heart failure with reduced ejection fraction. Sleep Breath 22, 1093–1100 (2018). https://doi.org/10.1007/s11325-018-1652-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1652-4