Abstract
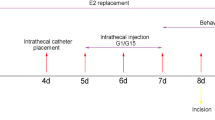
There is evidence that gonadal hormones may affect the perception of painful stimulation, although the underlying mechanisms remain unclear. This investigation was undertaken to determine whether the adenosine 5′-triphosphate (ATP) receptor subunit, P2X3, is involved in the modulatory action of estrogen in peripheral pain signal transduction in dorsal root ganglion (DRG). The mechanical pain behavior test, real-time quantitative reverse transcription–polymerase chain reaction analysis, and Western blot methods were used to determine the mean relative concentrations and functions of P2X3 receptors in DRG in sham, ovariectomized (OVX), and estradiol replacement (OVX+E2) female rats and in sham and orchiectomized male rats. The mechanical hyperalgesia appeared after ovariectomy, which was subsequently reversed after estradiol replacement, whereas it was not observed after orchiectomy in male rats. Plantar injection of 2′(3′)-O-(2,4,6-trinitrophenyl) ATP (TNP-ATP), a P2X3 and P2X2/3 receptor antagonist, resulted in an increase of the pain threshold force in OVX rats while had no effect on sham rats. Furthermore, A-317491, a selective P2X3/P2X2/3 receptor antagonist, significantly reversed the hyperalgesia of OVX rats. Injection of ATP into the plantars also caused a significant increase of the paw withdrawal duration in OVX rats compared with that seen in the sham group, which became substantially attenuated by TNP-ATP. P2X3 receptors expressed in DRG were significantly increased in both mRNA and protein levels after ovariectomy and then reversed after estrogen replacement, while a similar increase was not observed after orchiectomy in male rats. Furthermore, P2X3 mRNA was significantly decreased 24 h after the application of 17β-estradiol in a concentration-dependent manner in cultured DRG neurons. ICI 182,780, an estrogen receptor antagonist, blocked the reduction in the protein level. These results suggest that the female gonadal hormone, 17β-estradiol, might participate in the control of peripheral pain signal transduction by modulating P2X3 receptor-mediated events in primary sensory neurons, probably through genomic mechanisms.





Similar content being viewed by others
References
Fillingim RB (2000) Sex, gender, and pain: women and men really are different. Curr Rev Pain 4(1):24–30
Greenspan JD, Craft RM, LeResche L, Arendt-Nielsen L, Berkley KJ, Fillingim RB, Gold MS, Holdcroft A, Lautenbacher S, Mayer EA, Mogil JS, Murphy AZ, Traub RJ (2007) Consensus Working Group of the Sex, Gender, and Pain SIG of the IASP. Pain 132(Suppl 1):S26–S45
Craft RM (2007) Modulation of pain by estrogens. Pain 132:S3–S12
Butcher RL, Collins WE, Fugo NW (1974) Plasma concentration of LH, FSH, prolactin, progesterone, and estradiol-17beta throughout the 4-day estrous cycle of the rat. Endocrinology 94:1704–1708
Frye CA, Bock BC, Kanarek RB (1992) Hormonal milieu affects tailflick latency in female rats and may be attenuated by access to sucrose. Physiol Behav 52:699–706
Frye CA, Cuevas CA, Kanarek RB (1993) Diet and estrous cycle influence pain sensitivity in rats. Pharmacol Biochem Behav 45:255–260
Fischer L, Torres-Chávez KE, Clemente-Napimoga JT, Jorge D, Arsati F, de Arruda Veiga MC, Tambeli CH (2008) The influence of sex and ovarian hormones on temporomandibular joint nociception in rats. J Pain 9(7):630–638
Sanoja R, Cervero F (2005) Estrogen-dependent abdominal hyperalgesia induced by ovariectomy in adult mice: a model of functional abdominal pain. Pain 118(1–2):243–253
Sanoja R, Cervero F (2008) Estrogen modulation of ovariectomy-induced hyperalgesia in adult mice. Eur J Pain 12:573–581
Stoffel EC, Ulibarri CM, Craft RM (2003) Gonadal steroid hormone modulation of nociception, morphine antinociception and reproductive indices in male and female rats. Pain 103:285–302
Formanl LJ, Tingle V, Estilow S, Cater J (1989) The response to analgesia testing is affected by gonadal steroids in the rat. Life Sci 45(5):447–454
Bradshaw HB, Berkley KJ (2002) Estrogen replacement reverses ovariectomy-induced vaginal hyperalgesia in the rat. Maturitas 41:157–165
Gintzler AR, Bohan MC (1990) Pain thresholds are elevated during pseudopregnancy. Brain Res 507(2):312–316
Dawson-Basoa ME, Gintzler AR (1998) Gestational and ovarian sex steroid antinociception: synergy between spinal and opioid system. Brain Res 757:37–42
Unruh AM (1996) Gender variations in clinical pain experience. Pain 65:123–167
Berkley KJ (1997) Sex differences in pain. Behav Brain Sci 20:371–380
Robbins A, Berkley KJ, Sato Y (1992) Estrous cycle variation of afferent fibers supplying reproductive organs in the female rat. Brain Res 596(1–2):353–356
Sapsed-Byrne S, Ma D, Ridout D, Holdcroft A (1996) Estrous cycle phase variations in visceromotor and cardiovascular responses to colonic distension in the anesthetized rat. Brain Res 742(1–2):10–16
Holdcroft A, Sapsed-Byrne S, Ma D, Hammal D, Forsling ML (2000) Sex and oestrous cycle differences in visceromotor responses and vasopressin release in response to colonic distension in male and female rats anaesthetized with halothane. Br J Anaesth 85(6):907–910
Aloisi AM, Bonifazi M (2006) Sex hormones, central nervous system and pain. Horm Behav 50:1–7
Bettini E, Pollio G, Santagati S, Maggi A (1992) Estrogen receptor in rat brain: presence in the hippocampal formation. Neuroendocrinology 56(4):502–508
Papka RE, Srinivasan B, Miller KE, Hayashi S (1997) Localization of estrogen receptor protein and estrogen receptor messenger RNA in peripheral autonomic and sensory neurons. Neuroscience 79(4):1153–1163
Taleghany N, Sarajari S, DonCarlos LL, Gollapudi L, Oblinger MM (1999) Differential expression of estrogen receptor alpha and beta in rat dorsal root ganglion neurons. J Neurosci Res 57:603–615
Xiang Z, Bo X, Burnstock G (1998) Localization of ATP-gated P2X receptor immunoreactivity in rat sensory and sympathetic ganglia. Neurosci Lett 256(2):105–108
Burnstock G (2007) Physiology and pathophysiology of purinergic neurotransmission. Physiol Rev 87(2):659–797
Cockayne DA, Hamilton SG, Zhu QM, Dunn PM, Zhong Y, Novakovic S, Malmberg AB, Cain G, Berson A, Kassotakis L, Hedley L, Lachnit WG, Burnstock G, McMahon SB, Ford AP (2000) Urinary bladder hyporeflexia and reduced pain-related behaviour in P2X3-deficient mice. Nature 407(6807):1011–1015
Cockayne DA, Dunn PM, Zhong Y, Rong W, Hamilton SG, Knight GE, Ruan HZ, Ma B, Yip P, Nunn P, McMahon SB, Burnstock G, Ford AP (2005) P2X2 knockout mice and P2X2/P2X3 double knockout mice reveal a role for the P2X2 receptor subunit in mediating multiple sensory effects of ATP. J Physiol 567(Pt 2):621–639
Chaban VV, Mayer EA, Ennes HS, Micevych PE (2003) Estradiol inhibits ATP-induced intracellular calcium concentration increase in dorsal root ganglia neurons. Neuroscience 118:941–948
Ma B, Rong W, Dunn PM, Burnstock G (2005) 17β-estradiol attenuates α,β-meATP-induced currents in rat dorsal root ganglion neurons. Life Sci 76(22):2547–2558
Carley ME, Cliby WA, Spelsberg TC (2002) P2X3 receptor subunit messenger RNA expression in the female mouse bladder after oophorectomy with or without estrogen replacement. Am J Obstet Gynecol 187(1):103–106
Papka RE, Hafemeister J, Storey-Workley M (2005) P2X receptors in the rat uterine cervix, lumbosacral dorsal root ganglia, and spinal cord during pregnancy. Cell Tissue Res 321(1):35–44
McGaraughty S, Wismer CT, Zhu CZ, Mikusa J, Honore P, Chu KL, Lee CH, Faltynek CR, Jarvis MF (2003) Effects of A-317491, a novel and selective P2X3/P2X2/3 receptor antagonist, on neuropathic, inflammatory and chemogenic nociception following intrathecal and intraplantar administration. Br J Pharmacol 140(8):1381–1388
Hamilton SG, Wade A, McMahon SB (1999) The effects of inflammation and inflammatory mediators on nociceptive behaviour induced by ATP analogues in the rat. Br J Pharmacol 126(1):326–332
Sawynok J, Reid A (1997) Peripheral adenosine 5′-triphosphate enhances nociception in the formalin test via activation of a purinergic p2X receptor. Eur J Pharmacol 330(2–3):115–121
Gorodeski GI (1998) Estrogen increases the permeability of the cultured human cervical epithelium by modulating cell deformability. Am J Physiol 275:C888–C899
Jarvis MF, Wismer CT, Schweitzer E, Yu H, van Biesen T, Lynch KJ, Burgard EC, Kowaluk EA (2001) Modulation of BzATP and formalin induced nociception: attenuation by the P2X receptor antagonist, TNP-ATP and enhancement by the P2X(3) allosteric modulator, cibacron blue. Br J Pharmacol 132(1):259–269
Tsuda M, Shigemoto-Mogami Y, Koizumi S, Mizokoshi A, Kohsaka S, Salter MW, Inoue K (2003) P2X4 receptors induced in spinal microglia gate tactile allodynia after nerve injury. Nature 424(6950):778–783
Wakeling AE, Dukes M, Bowler JA (1991) A potent specific pure antiestrogen with clinical potential. Cancer Res 51:3867–3873
Gaumond I, Arsenault P, Marchand S (2002) The role of sex hormones on formalin-induced nociceptive responses. Brain Res 958(1):139–145
Gaumond I, Arsenault P, Marchand S (2005) Specificity of female and male sex hormones on excitatory and inhibitory phases of formalin-induced nociceptive responses. Brain Res 1052(1):105–111
Mannino CA, South SM, Quinones-Jenab V, Inturrisi CE (2007) Estradiol replacement in ovariectomized rats is antihyperalagesic in the formalin test. J Pain 8(4):334–342
Cutolo M, Villaggio B, Foppiani L, Briata M, Sulli A, Pizzorni C, Faelli F, Prete C, Felli L, Seriolo B, Giusti M (2000) The hypothalamic–pituitary–adrenocortical and gonadal axis function in rheumatoid arthritis. Z Rheumatol 59(Suppl):S65–S69
Navarro MA, Nolla JM, Machuca MI, González A, Mateo L, Bonnin RM, Roig-Escofet D (1998) Salivary testosterone in postmenopausal women with rheumatoid arthritis. J Rheumatol 25:1059–1062
Green PG, Dahlqvist SR, Isenberg WM, Strausbaugh HJ, Miao FJ, Levine JD (1999) Sex steroid regulation of the inflammatory response: sympathoadrenal dependence in the female rat. J Neurosci 19:4082–4089
Beyenburg S, Stoffel-Wagner B, Bauer J, Watzka M, Blumcke I, Bidlingmaier F, Elger CE (2001) Neuroactive steroids and seizure susceptibility. Epilepsy Res 44:141–153
Hammer RP Jr, Bridges RS (1987) Preoptric area opiods and opiate receptors increase during pregnancy and decrease during lactation. Brain Res 420(1):48–56
Dondi D, Limonta P, Maggi R, Piva F (1992) Effects of ovarian hormones on brain opioid binding sites in castrated female rats. Am J Physiol 263(3 Pt 1):E507–E511
Quinones-Jenab V, Jenab S, Ogawa S, Inturrisi C, Pfaff DW (1997) Estrogen regulation of mu-opioid receptor mRNA in the forebrain of female rats. Brain Res Mol Brain Res 47(1–2):134–138
Amandusson A, Hallbeck M, Hallbeck AL, Hermanson O, Blomqvist A (1999) Estrogen-induced alterations of spinal cord enkephalin gene expression. Pain 83(2):243–248
Burnstock G, Wood JN (1996) Purinergic receptors: their role in nociception and primary afferent neurotransmission. Curr Opin Neurobiol 6(4):526–532
Chen CC, Akopian AN, Sivilotti L, Colquhoun D, Burnstock G, Wood JN (1995) A P2X purinoreceptors expressed by a subset of sensory neurons. Nature 377:428–431
Lewis C, Neidhart S, Holy C, North RA, Buell G, Surprenant A (1995) Coexpression of P2X2 and P2X3 receptor subunits can account for ATP-gated currents in sensory neurons. Nature 377:432–435
North RA (2004) P2X3 receptors and peripheral pain mechanisms. J Physiol 554:301–308
Kobayashi K, Fukuoka T, Yamanaka H, Dai Y, Obata K, Tokunaga A, Noguchi K (2005) Differential expression patterns of mRNAs for P2X receptor subunits in neurochemically characterized dorsal root ganglion neurons in the rat. J Comp Neurol 481:377–390
Li L, Fan X, Warner M, Lili Li XuX-J, Gustafsson J-A, Wiesenfeld-Hallin Z (2009) Ablation of estrogen receptor α or β eliminates sex differences in mechanical pain threshold in normal and inflamed mice. Pain 143:37–40
Fan XT, Kim H-J, Warner M, Gustafsson J (2007) Estrogen receptor β is essential for sprouting of nociceptive primary afferents and for morphogenesis and maintenance of the dorsal horn interneurons. Proc Natl Acad Sci USA 104:13696–13701
Xu GY, Huang LY (2002) Peripheral inflammation sensitizes P2X receptor mediated responses in rat dorsal root ganglion neurons. J Neurosci 22:93–102
Xu GY, Huang LY (2004) Ca2+/calmodulin-dependent protein kinase II potentiates ATP responses by promoting trafficking of P2X receptors. Proc Natl Acad Sci USA 101:11868–11873
Acknowledgment
This study was supported by National Natural Science Foundation of China (NSFC, no. 30570597, B. Ma) and Program of Changjiang Scholar and innovative team. We are deeply grateful to Dr. Gillian E. Knight (from the Autonomic Neuroscience Centre, University College Medical School, UK) for her kind assistance in English writing.
Author information
Authors and Affiliations
Corresponding authors
Additional information
The first two authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ma, B., Yu, Lh., Fan, J. et al. Estrogen modulation of peripheral pain signal transduction: involvement of P2X3 receptors. Purinergic Signalling 7, 73–83 (2011). https://doi.org/10.1007/s11302-010-9212-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-010-9212-9