Abstract
Objectives
This retrospective study aimed to evaluate the effects of existing maxillary sinus pathologies on the survival rates of dental implants placed simultaneously with sinus augmentation.
Methods
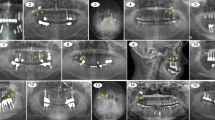
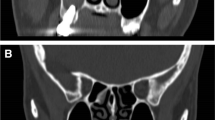
Cone-beam computed tomography images of 88 patients (34 females, 54 males), who underwent sinus augmentation, were retrospectively analyzed and the patients were divided into two groups: with (pathology group) and without pathology (control group). All maxillary sinus pathologies were recorded and categorized into mucosal thickening ( ≥ 3 mm), antral pseudocyst (polypoid mucosal thickening), and complete opacification. Implant survival rates were evaluated after a mean follow-up period of 28.2 ± 9.8 months based on the patient’s records and control radiographs.
Results
A total of 115 maxillary sinuses of 88 patients with 168 dental implants were included in the study. Maxillary sinus pathology was detected in 45 patients in the pathology group and 43 patients in the control group. In the pathology group, one implant was lost out of 82 implants during the 27.8 ± 9.5 months follow-up period, while in the control group, 5 implants were lost out of 86 implants during the 25.1 ± 10 months follow-up period. There was no statistically significant difference in the survival rates between the two groups.
Conclusions
The study concluded that the presence of pathology in the maxillary sinus before surgery does not affect the survival rates of dental implants placed simultaneously with sinus augmentation. The most common pathology noted included mucosal thickening (61.4%), which was detected in 35 patients.






Similar content being viewed by others
References
Korfage A, Raghoebar GM, Meijer HJA, Vissink A. Patients' expectations of oral implants: a systematic review. Eur J Oral Implantol. 2018;11(Suppl 1):S65–S76.
Antonoglou GN, Stavropoulos A, Samara MD, Ioannidis A, Benic GI, Papageorgiou SN, et al. Clinical performance of dental implants following sinus floor augmentation: a systematic review and meta-analysis of clinical trials with at least 3 years of follow-up. Int J Oral Maxillofac Implants. 2018;33:e45–e65.
Kozuma A, Sasaki M, Seki K, Toyoshima T, Nakano H, Mori Y. Preoperative chronic sinusitis as significant cause of postoperative infection and implant loss after sinus augmentation from a lateral approach. Oral Maxillofac Surg. 2017;21:193–200.
Manji A, Faucher J, Resnik RR, Suzuki JB. Prevalence of maxillary sinus pathology in patients considered for sinus augmentation procedures for dental implants. Implant Dent. 2013;22:428–35.
Kara MI, Kirmali O, Ay S. Clinical evaluation of lateral and osteotome techniques for sinus floor elevation in the presence of an antral pseudocyst. Int J Oral Maxillofac Implants. 2012;27:1205–10.
Kara IM, Kucuk D, Polat S. Experience of maxillary sinus floor augmentation in the presence of antral pseudocysts. J Oral Maxillofac Surg. 2010;68:1646–50.
Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E. Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol. 2009;38:187–95.
Mafee MF, Tran BH, Chapa AR. Imaging of rhinosinusitis and its complications: plain film, CT, and MRI. Clin Rev Allergy Immunol. 2006;30:165–86.
Havas TE, Motbey JA, Gullane PJ. Prevalence of incidental abnormalities on computed tomographic scans of the paranasal sinuses. Arch Otolaryngol Head Neck Surg. 1988;114:856–9.
Raghav M, Karjodkar FR, Sontakke S, Sansare K. Prevalence of incidental maxillary sinus pathologies in dental patients on cone-beam computed tomographic images. Contemp Clin Dent. 2014;5:361–5.
Gracco A, Incerti Parenti S, Ioele C, Alessandri Bonetti G, Stellini E. Prevalence of incidental maxillary sinus findings in Italian orthodontic patients: a retrospective cone-beam computed tomography study. Korean J Orthod. 2012;42:329–34.
Kfir E, Goldstein M, Abramovitz I, Kfir V, Mazor Z, Kaluski E. The effects of sinus membrane pathology on bone augmentation and procedural outcome using minimal invasive antral membrane balloon elevation. J Oral Implantol. 2014;40:285–93.
Ritter L, Lutz J, Neugebauer J, Scheer M, Dreiseidler T, Zinser MJ, et al. Prevalence of pathologic findings in the maxillary sinus in cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:634–40.
Friedland B, Metson R. A guide to recognizing maxillary sinus pathology and for deciding on further preoperative assessment prior to maxillary sinus augmentation. Int J Periodontics Restorative Dent. 2014;34:807–15.
Buser D, Weber HP, Bragger U, Balsiger C. Tissue integration of one-stage implants: three-year results of a prospective longitudinal study with hollow cylinder and hollow screw implants. Quintessence Int. 1994;25:679–86.
Albrektsson T, Zarb GA. Determinants of correct clinical reporting. Int J Prosthodont. 1998;11:517–21.
Albrektsson T, Sennerby L, Wennerberg A. State of the art of oral implants. Periodontol. 2000;2008(47):15–26.
Pazera P, Bornstein MM, Pazera A, Sendi P, Katsaros C. Incidental maxillary sinus findings in orthodontic patients: a radiographic analysis using cone-beam computed tomography (CBCT). Orthod Craniofac Res. 2011;14:17–24.
Cho BH, Jung YH. Prevalence of incidental paranasal sinus opacification in an adult dental population. Korean J Oral Maxillofac Radiol. 2009;39:191–4.
Rege IC, Sousa TO, Leles CR, Mendonca EF. Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health. 2012;12:30.
Lambert F, Lecloux G, Rompen E. One-step approach for implant placement and subantral bone regeneration using bovine hydroxyapatite: a 2- to 6-year follow-up study. Int J Oral Maxillofac Implants. 2010;25:598–606.
Chiapasco M, Zaniboni M. Methods to treat the edentulous posterior maxilla: implants with sinus grafting. J Oral Maxillofac Surg. 2009;67:867–71.
Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008;35:216–40.
Tukel HC, Tatli U. Risk factors and clinical outcomes of sinus membrane perforation during lateral window sinus lifting: analysis of 120 patients. Int J Oral Maxillofac Surg. 2018;47:1189–94.
Perfetti G, Rossi F, Massei G, Raffaelli L, Manicone PF, Paolantonio M, et al. Sinus augmentation procedure of the jaw sinus in patients with mucocele. Int J Immunopathol Pharmacol. 2008;21:243–6.
Lim HC, Nam JY, Cha JK, Lee JS, Lee DW, Jung UW, et al. Retrospective analysis of sinus membrane thickening: profile, causal factors, and its influence on complications. Implant Dent. 2017;26:868–74.
Shanbhag S, Karnik P, Shirke P, Shanbhag V. Cone-beam computed tomographic analysis of sinus membrane thickness, ostium patency, and residual ridge heights in the posterior maxilla: implications for sinus floor elevation. Clin Oral Implants Res. 2014;25:755–60.
Wen SC, Lin YH, Yang YC, Wang HL. The influence of sinus membrane thickness upon membrane perforation during transcrestal sinus lift procedure. Clin Oral Implants Res. 2015;26:1158–64.
Nkenke E, Stelzle F. Clinical outcomes of sinus floor augmentation for implant placement using autogenous bone or bone substitutes: a systematic review. Clin Oral Implants Res. 2009;20(Suppl 4):124–33.
Conrad HJ, Jung J, Barczak M, Basu S, Seong WJ. Retrospective cohort study of the predictors of implant failure in the posterior maxilla. Int J Oral Maxillofac Implants. 2011;26:154–62.
Zinser MJ, Randelzhofer P, Kuiper L, Zoller JE, De Lange GL. The predictors of implant failure after maxillary sinus floor augmentation and reconstruction: a retrospective study of 1045 consecutive implants. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:571–82.
Gultekin BA, Cansiz E, Borahan O, Mangano C, Kolerman R, Mijiritsky E, et al. Evaluation of volumetric changes of augmented maxillary sinus with different bone grafting biomaterials. J Craniofac Surg. 2016;27:e144–e148148.
Gultekin BA, Sirali A, Gultekin P, Yalcin S, Mijiritsky E. Does the laser-microtextured short implant collar design reduce marginal bone loss in comparison with a machined collar? Biomed Res Int. 2016;2016:9695389.
Funding
Nil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Küçükkurt, S. Evaluation of the survival of implant placement simultaneously with sinus augmentation: relationship in maxillary sinus pathologies. Oral Radiol 36, 225–237 (2020). https://doi.org/10.1007/s11282-019-00399-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-019-00399-w