Abstract
Bariatric surgery results in long-term weight loss and an improved metabolic phenotype due to changes in the gut-brain axis regulating appetite and glycaemia. Neuroendocrine alterations associated with bariatric surgery may also influence hedonic aspects of eating by inducing changes in taste preferences and central reward reactivity towards palatable food. However, the impact of bariatric surgery on disordered eating behaviours (e.g.: binge eating, loss-of-control eating, emotional eating and ‘addictive eating’), which are commonly present in people with obesity are not well understood. Increasing evidence suggests gut-derived signals, such as appetitive hormones, bile acid profiles, microbiota concentrations and associated neuromodulatory metabolites, can influence pathways in the brain implicated in food intake, including brain areas involved in sensorimotor, reward-motivational, emotional-arousal and executive control components of food intake. As disordered eating prevalence is a key mediator of weight-loss success and patient well-being after bariatric surgery, understanding how changes in the gut-brain axis contribute to disordered eating incidence and severity after bariatric surgery is crucial to better improve treatment outcomes in people with obesity.


Similar content being viewed by others
References
The GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. 2017. https://doi.org/10.1056/NEJMoa1614362.
Sjöström L, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65.
Griffiths LJ, Parsons TJ, Hill AJ. Self-esteem and quality of life in obese children and adolescents: A systematic review. Int J Pediatr Obes. 2010;5:282–304.
Wu Y-K, Berry DC. Impact of weight stigma on physiological and psychological health outcomes for overweight and obese adults: A systematic review. J Adv Nurs. 2018;74:1030–42.
Williams G, Fruhbeck G. Obesity: Science to practice. John Wiley & Sons; 2009.
Succurro E, et al. Obese patients with a binge eating disorder have an unfavorable metabolic and inflammatory profile. Medicine (Baltimore). 2015;94.
Saunders R. Binge eating in gastric bypass patients before surgery. Obes Surg. 1999;9:72–6.
Mannucci E, et al. Quality of life and overweight: the obesity related well-being (Orwell 97) questionnaire. Addict Behav. 1999;24(3):345–57.
Sjöström L, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
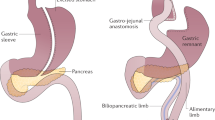
Rogers AM. Current state of bariatric surgery: Procedures, data, and patient management. Tech Vasc Interv Radiol. 2020;23:100654.
Ramos A, et al. IFSO Fifth Global Registry Report. Dendrite & Clinical Systems. 2019; 1-100.
Manning S, Pucci A, Batterham RL. Roux-en-Y gastric bypass: Effects on feeding behavior and underlying mechanisms. J Clin Invest. 2015;125:939–48.
Mulla CM, Middelbeek RJW, Patti M-E. Mechanisms of weight loss and improved metabolism following bariatric surgery. Ann N Y Acad Sci. 2018;1411:53–64.
Miras AD, le Roux CW. Mechanisms underlying weight loss after bariatric surgery. Nat Rev Gastroenterol Hepatol. 2013;10:575–84.
Murphy KG, Bloom SR. Gut hormones and the regulation of energy homeostasis. Nature. 2006;444:854–9.
Al-Najim W, Docherty NG, le Roux CW. Food intake and eating behavior after bariatric surgery. Physiol Rev. 2018;98:1113–41.
Opozda M, Chur-Hansen A, Wittert G. Changes in problematic and disordered eating after gastric bypass, adjustable gastric banding and vertical sleeve gastrectomy: A systematic review of pre-post studies. Obes Rev. 2016;17:770–92.
Vainik U, García-García I, Dagher A. Uncontrolled eating: A unifying heritable trait linked with obesity, overeating, personality and the brain. Eur J Neurosci. 2019;50:2430–45.
Stammers L, et al. Identifying stress-related eating in behavioural research: A review. Horm Behav. 2020;124:104752.
Dingemans A, Danner U, Parks M. Emotion regulation in binge eating disorder: A review. Nutrients. 2017;9:1274.
van Strien T. Causes of emotional eating and matched treatment of obesity. Curr Diab Rep. 2018;18:35.
Kessler RM, Hutson PH, Herman BK, Potenza MN. The neurobiological basis of binge-eating disorder. Neurosci Biobehav Rev. 2016;63:223–38.
Parker K, O’Brien P, Brennan L. Measurement of disordered eating following bariatric surgery: A systematic review of the literature. Obes Surg. 2014;24:945–53.
Baldofski S, et al. Nonnormative eating behavior and psychopathology in prebariatric patients with binge-eating disorder and night eating syndrome. Surg Obes Relat Dis. 2015;11:621–6.
Spirou D, Raman J, Smith E. Psychological outcomes following surgical and endoscopic bariatric procedures: A systematic review. Obes Rev. 2020;21.
Ivezaj V, Wiedemann AA, Grilo CM. Food addiction and bariatric surgery: A systematic review of the literature: Food addiction and bariatric surgery. Obes Rev. 2017;18:1386–97.
Dodsworth A, Warren-Forward H, Baines S. Changes in eating behavior after laparoscopic adjustable gastric banding: A systematic review of the literature. Obes Surg. 2010;20:1579–93.
Wong LY, et al. Change in emotional eating after bariatric surgery: Systematic review and meta-analysis. BJS Open. 2020;4:995–1014.
Athanasiadis DI, Martin A, Kapsampelis P, Monfared S, Stefanidis D. Factors associated with weight regain post-bariatric surgery: A systematic review. Surg Endosc. 2021. https://doi.org/10.1007/s00464-021-08329-w.
Bryant EJ, Malik MS, Whitford-Bartle T, Waters GM. The effects of bariatric surgery on psychological aspects of eating behaviour and food intake in humans. Appetite. 2020;150:104575.
Pepino MY, Stein RI, Eagon JC, Klein S. Bariatric surgery-induced weight loss causes remission of food addiction in extreme obesity. Obesity. 2014;22:1792–8.
Clark SM, Saules KK. Validation of the Yale Food Addiction Scale among a weight-loss surgery population. Eat Behav. 2013;14:216–9.
Kofman MD, Lent MR, Swencionis C. Maladaptive eating patterns, quality of life, and weight outcomes following gastric bypass: Results of an Internet survey. Obesity. 2010;18:1938–43.
Smith KE, et al. Loss of control eating and binge eating in the 7 years following bariatric surgery. Obes Surg. 2019;29:1773–80.
Conceição EM, Utzinger LM, Pisetsky EM. Eating disorders and problematic eating behaviours before and after bariatric surgery: Characterization, assessment and association with treatment outcomes. Eur Eat Disord Rev. 2015;23:417–25.
Marino JM, et al. The emergence of eating pathology after bariatric surgery: A rare outcome with important clinical implications. Int J Eat Disord. 2012;45:179–84.
Colles SL, Dixon JB, O’Brien PE. Grazing and loss of control related to eating: Two high-risk factors following bariatric surgery. Obesity. 2008;16:615–22.
Herpertz S, et al. Does obesity surgery improve psychosocial functioning? A systematic review. Int J Obes. 2003;27:1300–14.
Powers PS, Perez A, Boyd F, Rosemurgy A. Eating pathology before and after bariatric surgery: A prospective study. Int J Eat Disord. 1999;25:293–300.
Busetto L, et al. Weight loss and postoperative complications in morbidly obese patients with binge eating disorder treated by laparoscopic adjustable gastric banding. Obes Surg. 2005;15:195–201.
Saunders R. Compulsive eating and gastric bypass surgery: What does hunger have to do with It? Obes Surg. 2001;11:757–61.
Williams-Kerver GA, Steffen KJ, Mitchell JE. Eating pathology after bariatric surgery: An updated review of the recent literature. Curr Psychiatry Rep. 2019;21:86.
Rolls ET. Taste, olfactory and food texture reward processing in the brain and the control of appetite. Proc Nutr Soc. 2012;71:488–501.
Oberndorfer TA, et al. Altered insula response to sweet taste processing after recovery from anorexia and bulimia nervosa. Am J Psychiatry. 2013;170:1143–51.
Radeloff D, et al. High-fat taste challenge reveals altered striatal response in women recovered from bulimia nervosa: A pilot study. World J Biol Psychiatry. 2014;15:307–16.
Kenler HA, Brolin RE, Cody RP. Changes in eating behavior after horizontal gastroplasty and Roux-en-Y gastric bypass. Am J Clin Nutr. 1990;52:87–92.
Olbers T, et al. Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty. Ann Surg. 2006;244:715–22.
Ernst B, Thurnheer M, Wilms B, Schultes B. Differential changes in dietary habits after gastric bypass versus gastric banding operations. Obes Surg. 2009;19:274–80.
Zerrweck C, et al. Taste and olfactory changes following laparoscopic gastric bypass and sleeve gastrectomy. Obes Surg. 2016;26:1296–302.
Gero D, et al. Desire for core tastes decreases after sleeve gastrectomy: A single-center longitudinal observational study with 6-month follow-up. Obes Surg. 2017;27:2919–26.
Scholtz S, et al. Obese patients after gastric bypass surgery have lower brain-hedonic responses to food than after gastric banding. Gut. 2014;63:891–902.
Duan S, et al. Bariatric surgery induces alterations in effective connectivity between the orbitofrontal cortex and limbic regions in obese patients. Sci China Inf Sci. 2020;63:170104.
le Roux CW, et al. Gastric bypass reduces fat intake and preference. Am J Physiol Regul Integr Comp Physiol. 2011;301:R1057–66.
Seyfried F, et al. Effects of preoperative exposure to a high-fat versus a low-fat diet on ingestive behavior after gastric bypass surgery in rats. Surg Endosc. 2013;27:4192–201.
Zheng H, et al. Meal patterns, satiety, and food choice in a rat model of Roux-en-Y gastric bypass surgery. Am J Physiol Regul Integr Comp Physiol. 2009;297:R1273–82.
Shin AC, Zheng H, Pistell PJ, Berthoud H-R. Roux-en-Y gastric bypass surgery changes food reward in rats. Int J Obes. 2011;2005(35):642–51.
Saeidi N, et al. Sleeve gastrectomy and Roux-en-Y gastric bypass exhibit differential effects on food preferences, nutrient absorption and energy expenditure in obese rats. Int J Obes. 2012;2005(36):1396–402.
Bueter M, et al. Alterations of sucrose preference after Roux-en-Y gastric bypass. Physiol Behav. 2011;104:709–21.
Chelikani PK, Shah IH, Taqi E, Sigalet DL, Koopmans HH. Comparison of the effects of Roux-en-Y gastric bypass and ileal transposition surgeries on food intake, body weight, and circulating peptide YY concentrations in rats. Obes Surg. 2010;20:1281–8.
Wilson-Pérez HE, et al. The effect of vertical sleeve gastrectomy on food choice in rats. Int J Obes. 2013;2005(37):288–95.
García-Cabrerizo R, Carbia C, O’Riordan KJ, Schellekens H, Cryan JF. Microbiota-gut-brain axis as a regulator of reward processes. J Neurochem. 2021;157:1495–524.
Volkow ND, Wang G-J, Baler RD. Reward, dopamine and the control of food intake: Implications for obesity. Trends Cogn Sci. 2011;15:37–46.
Dallman MF, et al. Chronic stress and obesity: A new view of “comfort food.” Proc Natl Acad Sci U S A. 2003;100:11696–701.
Meule A. The psychology of food cravings: The role of food deprivation. Curr Nutr Rep. 2020;9:251–7.
Burge JC, Schaumburg JZ, Choban PS, DiSilvestro RA, Flancbaum L. Changes in patients’ taste acuity after Roux-en-Y gastric bypass for clinically severe obesity. J Am Diet Assoc. 1995;95:666–70.
Altun H, et al. Improved gustatory sensitivity in morbidly obese patients after laparoscopic sleeve gastrectomy. Ann Otol Rhinol Laryngol. 2016;125:536–40.
El Labban S, Safadi B, Olabi A. Effect of Roux-en-Y gastric bypass and sleeve gastrectomy on taste acuity and sweetness acceptability in postsurgical subjects. Nutrition. 2016;32:1299–302.
Pepino MY, et al. Changes in taste perception and eating behavior after bariatric surgery-induced weight loss in women. Obesity. 2014;22:E13–20.
Smith KR, et al. Taste-related reward is associated with weight loss following bariatric surgery. J Clin Invest. 2020;130:4370–81.
Thanos PK, et al. Roux-en-Y gastric bypass alters brain activity in regions that underlie reward and taste perception. PLoS One. 2015;10:e0125570.
Hajnal A, et al. Gastric bypass surgery alters behavioral and neural taste functions for sweet taste in obese rats. Am J Physiol Gastrointest Liver Physiol. 2010;299:G967–79.
Korner J, et al. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab. 2005;90:359–65.
le Roux CW, et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg. 2007;246:780–5.
Dickson SL, et al. The glucagon-like peptide 1 (GLP-1) analogue, exendin-4, decreases the rewarding value of food: A new role for mesolimbic GLP-1 receptors. J Neurosci. 2012;32:4812–20.
Hankir MK, et al. Gastric bypass surgery recruits a gut PPAR-α-striatal D1R pathway to reduce fat appetite in obese rats. Cell Metab. 2017;25:335–44.
Tellez LA, et al. A gut lipid messenger links excess dietary fat to dopamine deficiency. Science. 2013;341:800–2.
Romano A, et al. Oleoylethanolamide decreases frustration stress-induced binge-like eating in female rats: A novel potential treatment for binge eating disorder. Neuropsychopharmacology. 2020. https://doi.org/10.1038/s41386-020-0686-z.
Hankir MK, et al. Suppressed fat appetite after Roux-en-Y gastric bypass surgery associates with reduced brain μ-opioid receptor availability in diet-induced obese male rats. Front Neurosci. 2017;10:620.
Laleh P, Yaser K, Alireza O. Oleoylethanolamide: A novel pharmaceutical agent in the management of obesity-an updated review. J Cell Physiol. 2019;234:7893–902.
Karimian Azari E, et al. Vagal afferents are not necessary for the satiety effect of the gut lipid messenger oleoylethanolamide. Am J Physiol-Regul Integr Comp Physiol. 2014;307:R167–78.
Hutch CR, et al. Oea signaling pathways and the metabolic benefits of vertical sleeve gastrectomy. Ann Surg. 2020;271:509–18.
Goldstein N, et al. Hypothalamic detection of macronutrients via multiple gut-brain pathways. Cell Metab. 2021;33:676-687.e5.
Nielsen MS, Schmidt JB, le Roux CW, Sjödin A. Effects of Roux-en-Y Gastric bypass and sleeve gastrectomy on food preferences and potential mechanisms involved. Curr Obes Rep. 2019;8:292–300.
Seeley RJ, et al. The role of CNS glucagon-like peptide-1 (7–36) amide receptors in mediating the visceral illness effects of lithium chloride. J Neurosci. 2000;20:1616–21.
Dischinger U, et al. GLP-1 and PYY3-36 reduce high-fat food preference additively after Roux-en-Y gastric bypass in diet-induced obese rats. Surg Obes Relat Dis. 2019;15:1483–92.
Ahmad N, Pfalzer A, Kaplan L. Roux-en-Y gastric bypass normalizes the blunted postprandial bile acid excursion associated with obesity. Int J Obes. 2013;2005(37):1553–9.
Deems RO, Friedman MI. Macronutrient selection in an animal model of cholestatic liver disease. Appetite. 1988;11:73–80.
Perino A, et al. Central anorexigenic actions of bile acids are mediated by TGR5. Nat Metab. 2021;3:595–603.
Castellanos-Jankiewicz A, et al. Hypothalamic bile acid-TGR5 signaling protects from obesity. Cell Metab. 2021;33:1483-1492.e10.
Bensalem A, et al. Bile acid receptor TGR5 is critically involved in preference for dietary lipids and obesity. J Nutr Biochem. 2020;76:108298.
Nielsen MS, et al. Factors associated with favorable changes in food preferences after bariatric surgery. Obes Surg. 2021;31:3514–24.
Heitmann BL, Lissner L. Dietary underreporting by obese individuals–is it specific or non-specific? BMJ. 1995;311:986–9.
Nielsen MS, et al. Bariatric surgery does not affect food preferences, but individual changes in food preferences may predict weight loss. Obesity. 2018;26:1879–87.
Frank S, et al. Altered brain activity in severely obese women may recover after Roux-en Y gastric bypass surgery. Int J Obes. 2014;38:341–8.
Ochner CN, et al. Selective reduction in neural responses to high calorie foods following gastric bypass surgery. Ann Surg. 2011;253:502–7.
Ochner CN, et al. Neural responsivity to food cues in fasted and fed states pre and post gastric bypass surgery. Neurosci Res. 2012;74:138–43.
Gupta A, Osadchiy V, Mayer EA. Brain–gut–microbiome interactions in obesity and food addiction. Nat Rev Gastroenterol Hepatol. 2020;17:655–72.
Ravichandran S, et al. Alterations in reward network functional connectivity are associated with increased food addiction in obese individuals. Sci Rep. 2021;11:1–15.
Weygandt M, Schaefer A, Schienle A, Haynes J-D. Diagnosing different binge-eating disorders based on reward-related brain activation patterns. Hum Brain Mapp. 2012. https://doi.org/10.1002/hbm.21345.
van Bloemendaal L, et al. Brain reward-system activation in response to anticipation and consumption of palatable food is altered by glucagon-like peptide-1 receptor activation in humans. Diabetes Obes Metab. 2015;17:878–86.
van Bloemendaal L, et al. Emotional eating is associated with increased brain responses to food-cues and reduced sensitivity to GLP-1 receptor activation. Obesity. 2015;23:2075–82.
Wood SMW, et al. Emotional eating and routine restraint scores are associated with activity in brain regions involved in urge and self-control. Physiol Behav. 2016;165:405–12.
Chechlacz M, et al. Diabetes dietary management alters responses to food pictures in brain regions associated with motivation and emotion: A functional magnetic resonance imaging study. Diabetologia. 2009;52:524–33.
Killgore WDS, Yurgelun-Todd DA. Affect modulates appetite-related brain activity to images of food. Int J Eat Disord. 2006;39:357–63.
Wagner DD, Boswell RG, Kelley WM, Heatherton TF. Inducing negative affect increases the reward value of appetizing foods in dieters. J Cogn Neurosci. 2012. https://doi.org/10.1162/jocn_a_00238.
Eiler WJA, Dzemidzic M, Case KR, Considine RV, Kareken DA. Correlation between ventromedial prefrontal cortex activation to food aromas and cue-driven eating: An fMRI study. Chemosens Percept. 2012;5:27–36.
Bohon C, Stice E. Negative affect and neural response to palatable food intake in bulimia nervosa. Appetite. 2012;58:964–70.
Thanarajah SE, et al. Food intake recruits orosensory and post-ingestive dopaminergic circuits to affect eating desire in humans. Cell Metab. 2019;29:695-706.e4.
Dunn JP, et al. Decreased dopamine type 2 receptor availability after bariatric surgery: Preliminary findings. Brain Res. 2010;1350:123–30.
Steele KE, et al. Alterations of central dopamine receptors before and after gastric bypass surgery. Obes Surg. 2010;20:369–74.
Hankir MK, Ashrafian H, Hesse S, Horstmann A, Fenske WK. Distinctive striatal dopamine signaling after dieting and gastric bypass. Trends Endocrinol Metab. 2015;26:223–30.
Reddy IA, et al. Striatal dopamine homeostasis is altered in mice following Roux-en-Y gastric bypass surgery. ACS Chem Neurosci. 2014;5:943–51.
van der Zwaal EM, et al. Striatal dopamine D2/3 receptor availability increases after long-term bariatric surgery-induced weight loss. Eur Neuropsychopharmacol. 2016;26:1190–200.
Han W, et al. Striatal dopamine links gastrointestinal rerouting to altered sweet appetite. Cell Metab. 2016;23:103–12.
Goldstone AP, et al. Link between increased satiety gut hormones and reduced food reward after gastric bypass surgery for obesity. J Clin Endocrinol Metab. 2016;101:599–609.
ten Kulve JS, et al. Endogenous GLP1 and GLP1 analogue alter CNS responses to palatable food consumption. J Endocrinol. 2016;229:1–12.
Sweeney P, Yang Y. Neural circuit mechanisms underlying emotional regulation of homeostatic feeding. Trends Endocrinol Metab. 2017;28:437–48.
Bartra O, McGuire JT, Kable JW. The valuation system: A coordinate-based meta-analysis of BOLD fMRI experiments examining neural correlates of subjective value. Neuroimage. 2013;76:412–27.
Frost G, et al. The short-chain fatty acid acetate reduces appetite via a central homeostatic mechanism. Nat Commun. 2014;5:3611.
Byrne CS, et al. Increased colonic propionate reduces anticipatory reward responses in the human striatum to high-energy foods. Am J Clin Nutr. 2016;104:5–14.
Chambers ES, et al. Effects of targeted delivery of propionate to the human colon on appetite regulation, body weight maintenance and adiposity in overweight adults. Gut. 2015;64:1744–54.
Torres-Fuentes C, et al. Short-chain fatty acids and microbiota metabolites attenuate ghrelin receptor signaling. FASEB J. 2019;33:13546–59.
Dong TS, et al. A distinct brain-gut-microbiome profile exists for females with obesity and food addiction. Obesity. 2020;28:1477–86.
Sanmiguel CP, et al. Surgically induced changes in gut microbiome and hedonic eating as related to weight loss: Preliminary findings in obese women undergoing bariatric surgery. Psychosom Med. 2017;79:880–7.
Dong TS, et al. Improvement in uncontrolled eating behavior after laparoscopic sleeve gastrectomy is associated with alterations in the brain–gut–microbiome axis in obese women. Nutrients. 2020;12(10):2924.
Hong J, et al. Reversal of functional brain activity related to gut microbiome and hormones after VSG surgery in patients with obesity. J Clin Endocrinol Metab. 2021. https://doi.org/10.1210/clinem/dgab297.
Herman A, Bajaka A. The role of the intestinal microbiota in eating disorders – bulimia nervosa and binge eating disorder. Psychiatry Res. 2021;300:113923.
Jennis M, et al. Microbiota-derived tryptophan indoles increase after gastric bypass surgery and reduce intestinal permeability in vitro and in vivo. Neurogastroenterol Motil. 2018;30:e13178.
Osadchiy V, et al. Correlation of tryptophan metabolites with connectivity of extended central reward network in healthy subjects. PLoS One. 2018;13(8):e0201772.
Yano JM, et al. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell. 2015;161:264–76.
Finch L & Tomiyama AJ. Stress-induced eating dampens physiological and behavioral stress responses. In Nutrition in the prevention and treatment of abdominal obesity. 2019. Ch. 18; p. 189–195. https://doi.org/10.1016/B978-0-12-816093-0.00015-X.
van Strien T, et al. Emotional eating and food intake after sadness and joy. Appetite. 2013;66:20–5.
Tryon MS, Carter CS, DeCant R, Laugero KD. Chronic stress exposure may affect the brain’s response to high calorie food cues and predispose to obesogenic eating habits. Physiol Behav. 2013;120:233–42.
Wingenfeld K, et al. Stress reactivity and its effects on subsequent food intake in depressed and healthy women with and without adverse childhood experiences. Psychoneuroendocrinology. 2017;80:122–30.
Gluck ME, Geliebter A, Hung J, Yahav E. Cortisol, hunger, and desire to binge eat following a cold stress test in obese women with binge eating disorder. Psychosom Med. 2004;66:876–81.
Tomiyama AJ, Dallman MF, Epel ES. Comfort food is comforting to those most stressed: Evidence of the chronic stress response network in high stress women. Psychoneuroendocrinology. 2011;36:1513–9.
Dietrich A, Hollmann M, Mathar D, Villringer A, Horstmann A. Brain regulation of food craving: Relationships with weight status and eating behavior. Int J Obes. 2016;40:982–9.
García-García I, et al. Reward processing in obesity, substance addiction and non-substance addiction. Obes Rev. 2014;15:853–69.
Higgs S, Spetter MS. Cognitive control of eating: The role of memory in appetite and weight gain. Curr Obes Rep. 2018;7:50–9.
Demos KE, Heatherton TF, Kelley WM. Individual differences in nucleus accumbens activity to food and sexual images predict weight gain and sexual behavior. J Neurosci. 2012;32:5549–52.
Hankir MK, et al. Homeostatic, reward and executive brain functions after gastric bypass surgery. Appetite. 2020;146:104419.
Hankir MK, Seyfried F, Miras AD, Cowley MA. Brain feeding circuits after Roux-en-Y gastric bypass. Trends Endocrinol Metab. 2018;29:218–37.
Smitka K, et al. Current aspects of the role of autoantibodies directed against appetite-regulating hormones and the gut microbiome in eating disorders. Front Endocrinol. 2021;12:293.
Skonieczna-Żydecka K, et al. Gut Biofactory—Neurocompetent Metabolites within the Gastrointestinal Tract. A Scoping Review. Nutrients. 2020;12(11):3369.
Tavares GA, et al. Early weaning leads to disruption of homeostatic and hedonic eating behaviors and modulates serotonin (5HT) and dopamine (DA) systems in male adult rats. Behav Brain Res. 2020;383:112531.
Haahr ME, et al. Central 5-HT neurotransmission modulates weight loss following gastric bypass surgery in obese individuals. J Neurosci. 2015;35:5884–9.
Leyrolle Q, et al. Specific gut microbial, biological, and psychiatric profiling related to binge eating disorders: A cross-sectional study in obese patients. Clin Nutr. 2021;40:2035–44.
Clarke G, et al. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol Psychiatry. 2013;18:666–73.
Rea K, Dinan TG, Cryan JF. The microbiome: A key regulator of stress and neuroinflammation. Neurobiol Stress. 2016;4:23–33.
Navarro-Tapia E, et al. Effects of microbiota imbalance in anxiety and eating disorders: Probiotics as novel therapeutic approaches. Int J Mol Sci. 2021;22:2351.
Yang Y, Shields GS, Guo C, Liu Y. Executive function performance in obesity and overweight individuals: A meta-analysis and review. Neurosci Biobehav Rev. 2018;84:225–44.
Monica D, et al. Assessment of executive functions in obese individuals with binge eating disorder. Braz J Psychiatry. 2010;32:381–8.
Manasse SM, et al. Executive functioning in overweight individuals with and without loss-of-control eating. Eur Eat Disord Rev. 2014;22:373–7.
Han JE, Boachie N, Garcia-Garcia I, Michaud A, Dagher A. Neural correlates of dietary self-control in healthy adults: A meta-analysis of functional brain imaging studies. Physiol Behav. 2018;192:98–108.
Lavagnino L, Arnone D, Cao B, Soares JC, Selvaraj S. Inhibitory control in obesity and binge eating disorder: A systematic review and meta-analysis of neurocognitive and neuroimaging studies. Neurosci Biobehav Rev. 2016;68:714–26.
Balodis IM, Grilo CM, Potenza MN. Neurobiological features of binge eating disorder. CNS Spectr. 2015;20:557–65.
Hege MA, et al. Attentional impulsivity in binge eating disorder modulates response inhibition performance and frontal brain networks. Int J Obes. 2015;2005(39):353–60.
Burger KS, Stice E. Relation of dietary restraint scores to activation of reward-related brain regions in response to food intake, anticipated intake, and food pictures. Neuroimage. 2011;55:233–9.
Coletta M, et al. Brain activation in restrained and unrestrained eaters: An fMRI study. J Abnorm Psychol. 2009;118:598–609.
DelParigi A, et al. Successful dieters have increased neural activity in cortical areas involved in the control of behavior. Int J Obes. 2007;31:440–8.
Hollmann M, et al. Neural correlates of the volitional regulation of the desire for food. Int J Obes. 2012;36:648–55.
Born JM, et al. Differences between liking and wanting signals in the human brain and relations with cognitive dietary restraint and body mass index. Am J Clin Nutr. 2011;94:392–403.
Demos KE, Kelley WM, Heatherton TF. Dietary restraint violations influence reward responses in nucleus accumbens and amygdala. J Cogn Neurosci. 2011;23:1952–63.
Zoon HFA, et al. Altered neural inhibition responses to food cues after Roux-en-Y Gastric Bypass. Biol Psychol. 2018;137:34–41.
Goldman RL, et al. Executive control circuitry differentiates degree of success in weight loss following gastric-bypass surgery. Obesity. 2013;21:2189–96.
Hu Y. Laparoscopic sleeve gastrectomy improves brain connectivity in obese patients. J Neurol. 2020;10.
Weygandt M, et al. Interactions between neural decision-making circuits predict long-term dietary treatment success in obesity. Neuroimage. 2019;184:520–34.
Liu L, et al. Structural changes in brain regions involved in executive-control and self-referential processing after sleeve gastrectomy in obese patients. Brain Imaging Behav. 2019;13(3):830–40.
Hu Y, et al. Brain connectivity, and hormonal and behavioral correlates of sustained weight loss in obese patients after laparoscopic sleeve gastrectomy. Cereb Cortex. 2021;31:1284–95.
Prinz P, et al. Plasma bile acids show a positive correlation with body mass index and are negatively associated with cognitive restraint of eating in obese patients. Front Neurosci. 2015;9:199.
Delzenne NM, Cani PD, Daubioul C, Neyrinck AM. Impact of inulin and oligofructose on gastrointestinal peptides. Br J Nutr. 2005;93:S157–61.
Delbès A-S, et al. Prebiotics supplementation impact on the reinforcing and motivational aspect of feeding. Front Endocrinol. 2018;9:273.
Association AP. Feeding and eating disorders: DSM-5® selections. American Psychiatric Pub; 2015.
Sarwer DB, Allison KC, Bailer BA, Faulconbridge LF. Psychosocial characteristics of bariatric surgery candidates. The ASMBS textbook of bariatric surgery: Volume 2: Integrated Health 2014. pp. 3–9.
Marek RJ, Ben-Porath YS, Ashton K, Heinberg LJ. Minnesota multiphasic personality inventory-2 restructured form (MMPI-2-RF) scale score differences in bariatric surgery candidates diagnosed with binge eating disorder versus BMI-matched controls. Int J Eat Disord. 2014;47:315–9.
Mitchell JE, et al. Long-term follow-up of patients’ status after gastric bypass. Obes Surg. 2001;11:464–8.
Conceição EM, Goldschmidt A. Disordered eating after bariatric surgery: Clinical aspects, impact on outcomes, and intervention strategies. Curr Opin Psychiatry. 2019;32:504–9.
Niego SH, Kofman MD, Weiss JJ, Geliebter A. Binge eating in the bariatric surgery population: A review of the literature. Int J Eat Disord. 2007;40:349–59.
White MA, Kalarchian MA, Masheb RM, Marcus MD, Grilo CM. Loss of control over eating predicts outcomes in bariatric surgery patients: A prospective, 24-month follow-up study. J Clin Psychiatry. 2009;70:0–0.
Saunders R. ‘Grazing’: A high-risk behavior. Obes Surg. 2004;14:98–102.
Lydecker JA, Ivezaj V, Grilo CM. Secretive eating and binge eating following bariatric surgery. Int J Eat Disord. 2019;52:935–40.
Conceição EM, et al. Picking and nibbling: Frequency and associated clinical features in bulimia nervosa, anorexia nervosa and binge eating disorder. Int J Eat Disord. 2013;46:815–8.
Conceição EM, et al. Stability of problematic eating behaviors and weight loss trajectories after bariatric surgery: A longitudinal observational study. Surg Obes Relat Dis. 2017;13:1063–70.
Allison KC, et al. Night eating syndrome and binge eating disorder among persons seeking bariatric surgery: Prevalence and related features. Obesity. 2006;14:77S-82S.
de Zwaan M, Marschollek M, Allison KC. The night eating syndrome (NES) in bariatric surgery patients. Eur Eat Disord Rev. 2015;23:426–34.
Brode CS, Mitchell JE. Problematic eating behaviors and eating disorders associated with bariatric surgery. Psychiatr Clin North Am. 2019;42:287–97.
Brown RM. Addiction-like synaptic impairments in diet-induced obesity. Biol. Psychiatry. 2015;81:797-806. https://doi.org/10.1016/j.biopsych.2015.11.019.
Sevinçer GM. Food addiction and the outcome of bariatric surgery at 1-year: Prospective observational study. Psychiatry Res. 2016;6.
Funding
EGH is supported by a Melbourne Research Scholarship. CJF is supported by a National Health and Medical Research Council Ideas Grant (2001722). RMB is supported by ARC DECRA (DE190101244). PS is supported by a National Health and Medical Research Council Investigator Grant (1178482).
Author information
Authors and Affiliations
Contributions
EGH, PS, RMB conceived the idea and researched data for the manuscript. EGH wrote the first draft with assistance from PS and RMB. All authors reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Conflicts of interest
PS reports fees from Novo Nordisk for participation in advisory boards and a lecture unrelated to the submitted work. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guerrero-Hreins, E., Foldi, C.J., Oldfield, B.J. et al. Gut-brain mechanisms underlying changes in disordered eating behaviour after bariatric surgery: a review. Rev Endocr Metab Disord 23, 733–751 (2022). https://doi.org/10.1007/s11154-021-09696-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-021-09696-4