Abstract
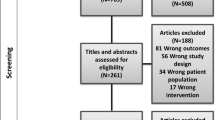
A lack of access to knowledgeable providers is the greatest reported barrier to care for transgender individuals. The purpose of this manuscript is to review the recent literature characterizing transgender medicine education for medical providers and to summarize effective interventions for improving education in transgender care. The PubMed database was searched for all literature that assessed transgender medical education among physicians or trainees and all papers that reported results of transgender-specific educational interventions. Literature that only evaluated general lesbian, gay, bisexual, and transgender (LGBT) educational interventions was excluded. The lack of education in transgender care continues among providers across all levels of medical education from medical students and physician trainees to primary care providers, endocrinologists and other specialists involved in transgender care. Several interventions have been shown to effectively improve transgender knowledge and cultural competency. Education among healthcare providers is deficient and is considered a major barrier to care for transgender individuals. Effective interventions should be applied to fundamental medical education. Additional focused education also should be taught with specialty-appropriate content to produce needed proficiency among providers of transgender care.

Similar content being viewed by others
References
Safer JD, Coleman E, Feldman J, Garofalo R, Hembree W, Radix A, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016 Apr;23(2):168–71.
Flores AR, Herman J, Gates GJ, Brown TNT. How many adults identify as transgender in the United States? UCLA: the Williams Institute. 2016. Available at: https://escholarship.org/uc/item/2kg9x2rk
Sanchez NF, Sanchez JP, Danoff A. Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in new York City. Am J Public Health. 2009;99(4):713–9.
Kenagy GP. Transgender health: findings from two needs assessment studies in Philadelphia. Health Soc Work. 2005 Feb;30(1):19–26.
Xavier JM, Simmons R. The Washington transgender needs assessment survey. 2000 Available at: http://www.glaa.org/archive/2000/tgneedsassessment1112.shtml.
Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013 Mar;13(3):214–22.
Grant JM, Mottet LA, Tanis J, Harrison J, Herman JL, Keisling M. Injustice at every turn: a report of the National Transgender Discrimination Survey. National Center for Transgender Equality and National Gay and Lesbian Task Force: Washington; 2011.
Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017 Nov 1;102(11):3869–903.
The World Professional Association for Transgender Health. The standards of Care for Transsexual, transgender, and gender nonconforming people, 7th version. Minneapolis, MN: the world professional Association for Transgender Health, Inc; 2011.
Implementing curricular and institutional climate changes to improve health care for individuals who are LGBT, gender nonconforming, or born with DSD. Available at: https://www.aamc.org/download/414172/data/lgbt.pdf?__hssc=&__hstc=&__hsfp=1645524416&hsCtaTracking=bd4a6b49-1c77-4054-8711-b55bde24e45b%7C090ff0e5-8d01-493d-8527-9fc74327757d.
Association of American Medical Colleges. Joint AAMC-GSA and AAMCOSR recommendations regarding institutional programs and educational activities to address the needs of gay, lesbian, bisexual and transgender (GLBT) students and patients. Washington, DC: Association of American Medical Colleges, 2007.
White W, Brenman S, Paradis E, Goldsmith ES, Lunn MR, Obedin-Maliver J, et al. Lesbian, gay, bisexual, and transgender patient care: medical students’ preparedness and comfort. Teach Learn Med. 2015;27(3):254–63.
Parameshwaran V, Cockbain BC, Hillyard M, Price JR. Is the lack of specific lesbian, gay, bisexual, transgender and queer/questioning (LGBTQ) health care education in medical school a cause for concern? Evidence from a survey of knowledge and practice among UK medical students. J Homosex. 2017;64(3):367–81.
Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011 Sep 7;306(9):971–7.
Chan B, Skocylas R, Safer JD. Gaps in transgender medicine content identified among Canadian medical school curricula. Transgend Health 2016 Jul 1;1(1):142–50.
Liang JJ, Gardner IH, Walker JA, Safer JD. Observed deficiencies in medical student knowledge of transgender and intersex health. Endocr Pract. 2017 Aug;23(8):897–906.
Thomas DD, Safer JD. A simple intervention raised resident-physician willingness to assist transgender patients seeking hormone therapy. Endocr Pract. 2015 Oct;21(10):1134–42.
Johnston CD, Shearer LS. Internal medicine resident attitudes, prior education, comfort, and knowledge regarding delivering comprehensive primary care to transgender patients. Transgend Health. 2017 Jul 1;2(1):91–5.
Shires DA, Stroumsa D, Jaffee KD, Woodford MR. Primary care providers’ willingness to continue gender-affirming hormone therapy for transgender patients. Fam Pract [Internet]. 2017 Dec 9; Available from: https://doi.org/10.1093/fampra/cmx119
Irwig MS. Transgender care by endocrinologists in the United States. Endocr Pract. 2016 Jul;22(7):832–6.
Davidge-Pitts C, Nippoldt TB, Danoff A, Radziejewski L, Natt N. Transgender health in endocrinology: current status of endocrinology fellowship programs and practicing clinicians. J Clin Endocrinol Metab. 2017 Apr 1;102(4):1286–90.
Unger CA. Care of the transgender patient: a survey of gynecologists’ current knowledge and practice. J Women's Health. 2015 Feb;24(2):114–8.
Morrison SD, Dy GW, Chong HJ, Holt SK, Vedder NB, Sorensen MD, et al. Transgender-related education in plastic surgery and urology residency programs. J Grad Med Educ. 2017 Apr;9(2):178–83.
Dy GW, Osbun NC, Morrison SD, Grant DW, Merguerian PA. Transgender education study group. Exposure to and attitudes regarding transgender education among urology residents. J Sex Med. 2016 Oct;13(10):1466–72.
Morrison SD, Chong HJ, Dy GW, Grant DW, Wilson SC, Brower JP, et al. Educational exposure to transgender patient Care in Plastic Surgery Training. Plast Reconstr Surg. 2016 Oct;138(4):944–53.
Canner JK, Harfouch O, Kodadek LM, Pelaez D, Coon D, Offodile AC 2nd, et al. Temporal Trends in Gender-Affirming Surgery Among Transgender Patients in the United States. JAMA Surg [Internet]. 2018 Feb 28; Available from: https://doi.org/10.1001/jamasurg.2017.6231.
Rutherford K, McIntyre J, Daley A, Ross LE. Development of expertise in mental health service provision for lesbian, gay, bisexual and transgender communities. Med Educ. 2012 Sep;46(9):903–13.
Park JA, Safer JD. Clinical exposure to transgender medicine Improves students’ preparedness above levels seen with didactic teaching alone: a key addition to the Boston University model for teaching transgender healthcare. Transgend Health. 2018 Jan 1;3(1):10–6.
Vance SR Jr, Deutsch MB, Rosenthal SM, Buckelew SM. Enhancing pediatric trainees’ and Students' knowledge in providing care to transgender youth. J Adolesc Health. 2017 Apr;60(4):425–30.
Braun HM, Garcia-Grossman IR, Quiñones-Rivera A, Deutsch MB. Outcome and impact evaluation of a transgender health course for health profession students. LGBT Health. 2017 Feb;4(1):55–61.
Eriksson SES, Safer JD. Evidence-based curricular content improves student knowledge and changes attitudes towards transgender medicine. Endocr Pract. 2016 Jul;22(7):837–41.
Kidd JD, Bockting W, Cabaniss DL, Blumenshine P. Special-“T” training: extended follow-up results from a residency-wide professionalism workshop on transgender health. Acad Psychiatry. 2016 Oct;40(5):802–6.
Safer JD, Pearce EN. A simple curriculum content change increased medical student comfort with transgender medicine. Endocr Pract. 2013 Jul;19(4):633–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state that they have no Conflict of Interest (COI).
Rights and permissions
About this article
Cite this article
Korpaisarn, S., Safer, J.D. Gaps in transgender medical education among healthcare providers: A major barrier to care for transgender persons. Rev Endocr Metab Disord 19, 271–275 (2018). https://doi.org/10.1007/s11154-018-9452-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-018-9452-5