Abstract
Background
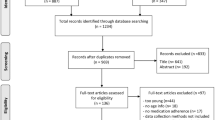
Although much is known about cardiovascular patients’ medication adherence, the extent to which clinicians perceive non-adherence as a barrier in clinical practice is little explored. Objective To evaluate knowledge and awareness about potential barriers to medication adherence, and to evaluate strategies used in clinical practice by Portuguese clinicians on how to foster medication adherence of patients undergoing secondary cardiovascular prevention. Setting Nominal Group Technique (NGT) at the University of Lisbon; online survey addressed to physicians working in primary and secondary care in Portugal. Method A narrative literature review was conducted in Pubmed to identify studies describing interventions targeted at physicians to manage medication adherence. The NGT included 12 allied healthcare professionals with recognized expertise in medication adherence and was organised in four phases, resulting in survey development. The survey was used in a cross-sectional national study where clinicians reported their knowledge and perceptions about patients’ medication adherence and their daily practice. Main outcome measures Knowledge and awareness about barriers to medication adherence; and practice patterns. Results A total of 296 papers were identified, 26 of which were included. Four main topics were selected to be used in the NGT: adherence determinants, detecting non-adherence, fostering adherence, and educating physicians. NGT resulted in a survey, reaching 451 physicians, mostly practicing in primary care. Most had specific education on medication adherence and considered patient interviews and prescription records the most useful assessment methods. Nonetheless, many recognised often using clinical judgement to evaluate adherence in practice. Barriers to medication adherence were perceived to occur often during implementation. Most perceived reasons for uncontrolled hypertension were non-adherence to lifestyle recommendations and to medication. Less than half the physicians asked their patients if medication was taken. More useful enabling strategies included reducing daily doses, reviewing therapeutic options and motivational interventions. Conclusions Clinicians seem well informed about the importance of medication adherence and aware of problems encountered in practice. Limited time during medical appointment may be a barrier for better patient support.



Similar content being viewed by others
References
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al, on behalf of GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736–1788.
World Health Organization. Global status report on noncommunicable diseases 2014: “Attaining the nine global noncommunicable diseases targets; a shared responsibility.” Geneva: World Health Organization; 2014.
Patnode CD, Evans CV, Senger CA, Redmond N, Lin JS. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults without known cardiovascular disease risk factors: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017;318(2):175–93.
Parappilly BP, Field TS, Mortenson WB, Sakakibara BM, Eng JJ. Effectiveness of interventions involving nurses in secondary stroke prevention: a systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2018;8(17):728–36.
Alshehri AA, Jalal Z, Cheema E, Haque MS, Jenkins D, Yahyouche A. Impact of the pharmacist-led intervention on the control of medical cardiovascular risk factors for the primary prevention of cardiovascular disease in general practice: a systematic review and meta-analysis of randomised controlled trials. Br J Clin Pharmacol. 2020;86(1):29–38.
Xu R, Xie X, Li S, Chen X, Wang S, Hu C, et al. Interventions to improve medication adherence among Chinese patients with hypertension: a systematic review and meta-analysis of randomized controlled trials. Int J Pharm Pract. 2018;26(4):291–301.
Fuller RH, Perel P, Navarro-Ruan T, Nieuwlaat R, Haynes RB, Huffman MD. Improving medication adherence in patients with cardiovascular disease: a systematic review. Heart. 2018;104(15):1238–43.
Palmer MJ, Barnard S, Perel P, Free C. Mobile phone-based interventions for improving adherence to medication prescribed for the primary prevention of cardiovascular disease in adults. Cochrane Database Syst Rev. 2018;6(6):CD012675.
Martins SF, van Mil JWF, Alves da Costa F. The organizational framework of community pharmacies in Europe. Int J Clin Pharm. 2015;37(5):896–905.
Soares IB, Imfeld-Isenegger TL, Makovec UN, Horvat N, Kos M, Arnet I, et al. A survey to assess the availability, implementation rate and remuneration of pharmacist-led cognitive services throughout Europe. Res Social Adm Pharm. 2020;16(1):41–7.
Ministério da Saúde. Portaria n.º 97/2018. Diário da República n.º 69/2018, Série I de 2018-04-09. Defines pharmaceutical services to be made available in community pharmacies. https://data.dre.pt/eli/port/97/2018/04/09/p/dre/pt/html.
Kulkarni J, Reeve-Parker K. Psychiatrists’ awareness of partial-and non-adherence to antipsychotic medication in schizophrenia: results from the Australian ADHES survey. Australas Psychiatry. 2015;23:258–64.
Barfoed BL, Paulsen MS, Christensen PM, Halvorsen PA, Kjær T, Larsen ML, et al. Associations between patients’ risk attitude and their adherence to statin treatment—a population based questionnaire and register study. BMC Fam Pract. 2016;17:28.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84. https://doi.org/10.1136/jech.52.6.377.
Costa FA, Scullin C, Al-Taani G, Hawwa AF, Anderson C, Bezverhni Z, et al. Provision of pharmaceutical care by community pharmacists across Europe: is it developing and spreading? J Eval Clin Pract. 2017;23(6):1336–47.
Clyne W, Mshelia C, McLachlan S, Jones P, De Geest S, Ruppar T, et al. A multinational cross-sectional survey of the management of patient medication adherence by European healthcare professionals. BMJ Open. 2016;6:e009610.
R Development Core Team. R: a language and environment for statistical computing. Vienna, Austria. R Foundation for Statistical Computing, 2008. ISBN 3-900051-07-0.
Vrijens B, DeGeest S, Hughes DA, Kardas P, Demonceau J, Ruppar T, et al. A new taxonomy for describing and defining dherence to medications. Brit J Clin Pharmacol. 2012;73:691–705.
Nogueira JD. Duração da Consulta: Perspectivas dos Médicos e dos Pacientes. [Duration of the medical appointment: physicians and patients’ perspectives]. Rev Port Clin Geral. 2002;18:303–12.
Granja M, Ponte C, Cavadas LF. What keeps family physicians busy in Portugal? A multicentre observational study of work other than direct patient contacts. BMJ Open. 2014;4:e005026.
Hauser K, Matthes J. Medical students’ medication communication skills regarding drug prescription—a qualitative analysis of simulated physician-patient consultations. Eur J Clin Pharmacol. 2017. https://doi.org/10.1007/s002.
Härtl A, Bachmann C, Blum K, Höfer S, Peters T, Preusche I, et al. Desire and reality—teaching and assessing communicative competencies in undergraduate medical education in German-speaking Europe—a survey. GMS Z Med Ausbild. 2015;32:Doc56.
Lavanya SH, Kalpana L, Veena RM, Bharath Kumar VD. Role-play as an educational tool in medication communication skills: students’ perspectives. Indian J Pharmacol. 2016;48:33–6.
Costa FA, Pedro AR, Teixeira I, Bragança F, Silva JA, Cabrita J. Primary non-adherence in Portugal: findings and implications. Int J Clin Pharm. 2015;37:626–35.
Blaschke TF, Osterberg L, Vrijens B, Urquhart J. Adherence to medications: insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu Rev Pharmacol Toxicol. 2012;52:275–301.
Costa FA, Teixeira I, Duarte-Ramos F, Proença L, Pedro AR, Furtado C, Silva JA, Cabrita J. Effects of economic recession on elderly patients’ perceptions of access to health care and implications on their medicines-taking behaviour in Portugal. Int J Clin Pharm. 2016;39:104–12.
Jeffery RA, Navarro T, Wilczynski NL, Iserman EC, Keepanasseril A, Sivaramalingam B, et al. Adherence measurement and patient recruitment methods are poor in intervention trials to improve patient adherence. J Clin Epidemiol. 2014;67(10):1076–82.
Winters A, Esse T, Bhansali A, Serna O, Mhatre S, Sansgiry S. Physician perception of patient medication adherence in a cohort of medicine advantage plans in Texas. J Managed Care Spec Pharm. 2016;22:305–12.
Makoul G, Arntson P, Schofield T. Health promotion in primary care: physician–patient communication and decision making about prescription medications. Soc Sci Med. 1995;41:1241–54.
Stevenson FA, Barry CA, Britten N, Barber N, Bradley CP. Doctor–patient communication about drugs: the evidence for shared decision making. Soc Sci Med. 2000;50:829–40.
Richard C, Lussier M-T. Nature and frequency of exchanges on medications during primary care encounters. Patient Educ Couns. 2006;64:207–16.
Saba M, Diep J, Saini B, Dhippayom T. Meta-analysis of the effectiveness of smoking cessation interventions in community pharmacy. J Clin Pharm Ther. 2014;39(3):240–7.
Um IS, Krass I, Armour C, Gill T, Chaar BB. Developing and testing evidence-based weight management in Australian pharmacies: a Healthier Life Program. Int J Clin Pharm. 2015;37(5):822–33.
Milosavljevic A, Aspden T, Harrison J. Community pharmacist-led interventions and their impact on patients’ medication adherence and other health outcomes: a systematic review. Int J Pharm Pract. 2018;26(5):387–97.
Acknowledgements
To all the physicians who cooperated with this study by answering the survey.
Funding
The study was financed by Ferrer S.A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
FAC reports non-financial support from Bayer Global outside the submitted work. The remaining authors declare no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aguiar, J., Ribeiro, M., Pedro, A.R. et al. Awareness about barriers to medication adherence in cardiovascular patients and strategies used in clinical practice by Portuguese clinicians: a nationwide study. Int J Clin Pharm 43, 629–636 (2021). https://doi.org/10.1007/s11096-020-01174-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01174-2