Abstract
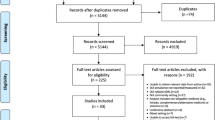
Background Drug interactions (DIs) are a significant cause of medication-related problems. The aging population, high chronic diseases prevalence and polypharmacy are closely associated factors. Aim of the review To study the prevalence, types and associated factors of DIs in multimorbidity patients of over 65 years of age in primary care. Methods Relevant studies on DI prevalence in this population were reviewed in PubMed, Cochrane Library and EMBASE (January 2000–December 2015). Independent variables (duration, target population, age, sex, mean of drugs and diseases, geographical localization, DI databases used and study designs) and dependent variables (prevalence, number of DIs per 100 patients and per patient, number of clinically-relevant DIs per 100 patients, most common DI and associated factors) were classified for each article. Results The search generated 749 articles and 46 duplicates were discarded. After reviewing, 10 articles were included. Seven studies were observational and 3 were quasi-experimental. Seven out of 10 used interaction databases. Only 2 studies described both actual and potential DIs. The prevalence of multimorbidity patients with DI ranged from 25.1 to 100% and the number of DIs per 100 patients was from 30 to 388.3. All the lower values correspond to the study conducted at the nursing home. This could be due to special care offered in these centres, where the medication is more controlled. The most frequent DIs were reported in five articles. However, these results could not be correlated since they were ranked using different methodologies. ACEIs, diuretics and NSAID were the most common therapeutic groups. Finally, 5 studies identified factors associated with the presence of potential DIs. The number of drugs and age were the most significant factors. Conclusions There is little evidence of prevalence of actual and potential DIs in elderly patients with multimorbidity in outpatient settings, showing widely heterogeneous results.

Similar content being viewed by others
References
Lenssen R, Heidenreich A, Schulz JB, Trautwein C, Fitzner C, Jaehde U, et al. Analysis of drug-related problems in three departments of a German University hospital. Int J Clin Pharm. 2016;38:119–26.
Sharifi H, Hasanloei MA, Mahmoudi J. Polypharmacy-induced drug-drug interactions; threats to patient safety. Drug Res (Stuttg). 2014;64:633–7.
Parker MG, Thorslund M. Health trends in the elderly population: gettingbetter and getting worse. Gerontologist. 2007;47:150–8.
Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294:716–24.
Opondo D, Eslami S, Visscher S, de Rooij SE, Verheij R, Korevaar JC, et al. Inappropriateness of medication prescriptions to elderly patients in the primary care setting: a systematic review. PLoS ONE. 2012;7(8):e43617.
Panagioti M, Stokes J, Esmail A, Coventry P, Cheraghi-Sohi S, Alam R, Bower P. Multimorbidity and patient safety incidents in primary care: a systematic review and meta-analysis. PLoS ONE. 2015;10(8):e0135947.
World Health Organisation. Definition of an older or elderly person. WHO, Geneva, Switzerland. 2010. http://www.who.int/healthinfo/survey/ageingdefnolder/en/index.html. Accessed 15 Aug 2016.
Orimo H, Ito H, Suzuki T, Araki A, Hosoi T, Sawabe M. Reviewing the definition of “elderly”. Geriatr Gerontol Int. 2006;6:149–58.
Nabovati E, Vakili-Arki H, Taherzadeh Z, Hasibian MR, Abu-Hanna A, Eslami S. Drug-drug interactions in inpatient and outpatient settings in Iran: a systematic review of the literature. Daru. 2014;25(22):52.
Doubova-Dubova SV, Reyes-Morales H, Torres-Arreola LP, Suárez-Ortega M. Potential drug drug and drug disease interactions in prescriptions for ambulatory patients over 50 years of age in family medicine clinics in Mexico City. BMC Health Serv Res. 2007;19(7):147.
Liao HL, Chen JT, Ma TC, Chang YS. Analysis of drug-drug interactions (DDIs) in nursing home in Central Taiwan. Arch Gerontol Geriatr. 2008;47:99–107.
Gagne JJ, Maio V, Rabinowitz C. Prevalence and predictors of potential drugdrug interactions in Regione EmiliaRomagna, Italy. J Clin Pharm Ther. 2008;33:14151.
Tulner LR, Frankfort SV, Gijsen GJ, van Campen JP, Koks CH, Beijnen JH. Drug drug interactions in a geriatric outpatient cohort: prevalence and relevance. Drugs Aging. 2008;25:3435.
Galindo-Ocaña J, Gil-Navarro MV, García-Morillo JS, Bernabeu-Wittel M, Ollero-Baturone M, Ortiz-Camuñez MA. Drug drug interactions in multicentre polypathological polymedicated patients. Rev Clin Esp. 2010;210:2708.
Fiss T, Dreier A, Meinke C, van den Berg N, Ritter CA, Hoffmann W. Detection of drug related problems in an interdisciplinary health care model for rural areas in Germany. Pharm World Sci. 2010;32:566–74.
Hoffmann W, van den Berg N, Thyrian JR, Fiss T. Frequency and determinants of potential drug drug interactions in an elderly population receiving regular home visits by Gps results of the home medication review in the AgnESstudies. Pharmacoepidemiol Drug Saf. 2011;20:13118.
Marusic S, BacicVrca V, Obreli Neto PR, Franic M, Erdeljic V, GojoTomic N. Actual drugdrug interactions in elderly patients discharged from internal medicine clinic: a prospective observational study. Eur J Clin Pharmacol. 2013;69:171724.
Fiß T, MeinkeFranze C, van den Berg N. Hoffmann W Effects of a three party healthcare network on the incidence levels of drug related problems. Int J Clin Pharm. 2013;35:76371.
Bazargan M, Yazdanshenas H, Han S, Orum G. Inappropriate medication use among underserved elderly African Americans. J Aging Health. 2016;28:118–38.
Malone DC, Abarca J, Hansten PD, Grizzle AJ, Armstrong EP, Van Bergen RC, Duncan-Edgar BS, Solomon SL, Lipton RB. Identification of serious drug–drug interactions: results of the partnership to prevent drug–drug interactions. J Am Pharm Assoc. 2004;44:142–51.
Samsa GP, Hanlon JT, Schmader KE. A summated score for theMedication Appropriateness Index: development and assessment of clinimetric properties including content validity. J Clin Epidemiol. 1994;47:891–6.
Charlson ME, Pompei P, Ales KA, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies. J Chron Dis. 1987;40:373–83.
Maio V, Yuen EJ, Novielli K, Smith KD, Louis DZ. Potentially inappropriate medication prescribing for elderly outpatients in Emilia Romagna, Italy: a population-based cohort study. Drugs Aging. 2006;23:915–24.
Clark DO, Von Korff M, Saunders K, Baluch WM, Simon GE. A chronic disease score with empirically derived weights. Med Care. 1995;33:783–95.
Mallet L, Spinewine A, Huang A. The challenge of managing drug interactions in elderly people. Lancet. 2007;370:185–91.
Dechamont S, Maphanta S, Butthum B, Kongkew C. Hospital admissions/visits associated with drug-drug interactions: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. 2014;23:489–97.
Björkman IK, Fastbom J, Schmidt IK, Bernsten CB, the Pharmaceutical Care of the Elderly in Europe Research (PEER) Group. Drug–drug interactions in the elderly. Ann Pharmacother. 2002;36:1675–81.
Abarca J, Malone DC, Armstrong EP, Grizzle AJ, Hansten PD, Van Bergen RC, Lipton RB. Concordance of severity ratings provided in four drug interaction compendia. J Am Pharm Assoc. 2003;2004(44):136–41.
Rodríguez-Terol A, Caraballo MO, Palma D, Santos-Ramos B, Molina T, Desongles T, et al. Quality of interaction database management systems. Farm Hosp. 2009;33:134–46.
Zhang Y, Baicker K, Newhouse JP. Geographic variation in the quality of prescribing. N Engl J Med. 2010;363:1985–8.
Cusack BJ. Pharmacokinetics in older persons. Am J Geriatr Pharmacother. 2004;2:274–302.
Perazella MA, Mahnensmith RL. Hyperkalemia in the elderly: drugs exacerbate impaired potassium homeostasis. J Gen Intern Med. 1997;12:646–56.
Uijtendaal EV, Zwart-van Rijkom JE, van Solinge WW, Egberts TC. Frequency of laboratory measurement and hyperkalaemia in hospitalised patients using serum potassium; oncentration increasing drugs. Eur J Clin Pharmacol. 2011;67:933–40.
Zwart-van Rijkom JE, Uijtendaal EV, ten Berg MJ, van Solinge WW, Egberts AC. Frequency and nature of drug–drug interactions in a Dutch university hospital. Br J Clin Pharmacol. 2009;68:187–93.
Cruciol-Souza JM, Thomson JC. Prevalence of potential drugdrug interactions and its associated factors in a Brazilian teaching hospital. Pharm Pharm Sci. 2006;9:427–33.
Janchawee B, Wongpoowarak W, Owatranporn T, Chongsuvivatwong V. Pharmacoepidemiologic study of potential drug interactions in outpatients of a university hospital in Thailand. J Clin Pharm Ther. 2005;30:13–20.
Johnell K, Klarin I. The relationship between number of drugs and potential drug-drug interactions in the elderly. Drug Saf. 2007;30:911–8.
Viktil KK, Blix HS, Moger TA, Reikvam A. Polypharmacy as commonly defined is an indicator of limited value innthe assessment of drug-related problems. Br J Clin Pharmacol. 2007;63:187–95.
Magro L, Moretti U, Leone R. Epidemiology and characteristics of adverse drug reactions caused by drug-drug interactions. Expert Opin Drug Saf. 2012;11:83–94.
Steinman MA, Hanlon JT. Managing medications in clinically complex elders: “There’s got to be a happy medium”. JAMA. 2010;304:1592–601.
National Institute for Health and Care Excellence (NICE). Multimorbidity: clinical assessment and management. London, United Kingdom, 2016. https://www.nice.org.uk/guidance/ng56. Accessed 15 Dec 2016.
Funding
None.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sánchez-Fidalgo, S., Guzmán-Ramos, M.I., Galván-Banqueri, M. et al. Prevalence of drug interactions in elderly patients with multimorbidity in primary care. Int J Clin Pharm 39, 343–353 (2017). https://doi.org/10.1007/s11096-017-0439-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-017-0439-1