Abstract
Introduction
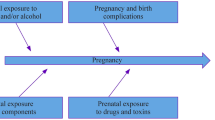
Attention deficit/hyperactivity disorder (ADHD) is a neurobehavioral problem found in 2–5% of adults. Stimulants and drugs that affect the dopaminergic, noradrenergic and/or serotonergic systems are effective treatment and are increasingly prescribed to women at child bearing age. It is consequently important that reliable information on the safety of these drugs in pregnancy is available so that appropriate therapeutic choices can be made.
Results
The data on stimulants (methylphenidate and amphetamines) are generally showing that there is no increase in the rate of major congenital anomalies. There are very little data on the use of atomoxetine and guanfacine in pregnancy. There are no data on the use of clonidine for ADHD but the data on its use as an antihypertensive drug have not revealed any serious adverse effect. Bupropion, when used as an antidepressant, does not seem to increase the rate of congenital anomalies. There are practically no data on the possible long-term neurodevelopmental effects of any of these drugs. Most of them are secreted in human milk, but the concentrations in infant’s blood, except for clonidine and amphetamines, have been very low. Breast feeding with clonidine and amphetamines is therefore contraindicated, but there seems to be no safety concerns for the other drugs.
Conclusion
The drugs used for the treatment of ADHD are apparently not teratogenic, but due to paucity of data, especially on the long-term neurodevelopmental outcome, the treating physician should reconsider the need of treatment during pregnancy. If needed, methylphenidate, amphetamines and bupropion are preferred drugs.
Similar content being viewed by others
Abbreviations
- ADHD:
-
Attention deficit/Hyperactivity disorder
- aOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- CPTs:
-
Computerized attentional performance tests
- DSM 5:
-
Diagnostic statistical manual 5
- DTI:
-
Diffusion tensor imaging
- MDMA:
-
Methylenedeoxymetamphetamine
- MRI:
-
Magnetic resonance imaging
- SNRIs:
-
Serotonin norepinephrine reuptake inhibitors
- OR:
-
Odds ratio
- Ritalin IR:
-
Ritalin immediate release
- Ritalin LA:
-
Ritalin long acting
- Ritalin SR:
-
Ritalin sustained release
- SGA:
-
Small for gestational age
- SSRIs:
-
Serotonin reuptake inhibitors
- VSD:
-
Ventricular septal defect
References
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. American psychiatric association Association. 2013; pp59–66.
Yochman A, Ornoy A, Parush S. Co-occurrence of developmental delays among preschool children with Attention Deficit Hyperactivity Disorder. Develop Med Child Neurol. 2006;48:483–6.
Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016;387:1240–50.
Biederman J, Faraone SV. Attention Deficit hyperactivity disorder. Lancet. 2005;366:23.
Curry AE, Metzger KB, Pfeifer MR, Elliott MR, Winston FK, Power TJ. Motor vehicle crash risk among adolescents and young adults with attention deficit/hyperactivity disorder. JAMA Pediatr. 2017:E1–8.
Sauver JL, Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Early life risk factors for Attention Deficit Hyperactivity Disorder: A population-based cohort study. Mayo Clinic Proc. 2004;79:1124–31.
De Ridder A, De Graeve D. Healthcare use, social burden and costs of children with and without ADHD in Flanders. Belgium Clin Drug Investig. 2006;26(2):75–90.
Pelham WE, Foster M, Robb JA. The economic impact of Attention-Deficit/Hyperactivity disorder in children and adolescents. Ambul Pediatr. 2007;18:121–31.
Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of Attention-Deficit/Hyperactivity Disorder. A systematic review and meta-analysis. Pediatrics. 2015;135:e994–e1001.
Ornoy A, Ovadia M, Rivkin D, Milshtein E, Barlev L. Prevalence of ADHD among 7-9 years old children in Israel. A comparison between the Jewish and Arab populations. Isr J Psychiatry. 2016;53(2):3–8.
Simon V, Czobor P, Balint S, Meszaros A, Bitter I. Prevalence and correlates of adult attention- deficit hyperactivity disorder: meta-analysis. Br J Psych. 2009;194(3):204–11.
Besag FM. ADHD treatment and pregnancy. Drug Saf. 2014;37(6):397–408.
Louik C, Ker S, Kelley KE, Mitchell AA. Increasing use of ADHD medications in pregnancy. Pharmacoepidemiol Drugs Saf. 2015;24(2):218–20.
Heal DJ, Cheetham SC. Smith SL The neuropharmacology of ADHD drugs in vivo: insights on efficacy and safety. Neuropharmacology. 2009;57(7–8):608–18.
Crescenzo FD, Cortese S, Adamo N, Janiri L. Pharmacological and non-pharmacological treatment of adults with ADHD: a meta-review Evid Based Ment Health 2017; 20(1):4–11.
Stuhec M, Munda B, Svab V, Locatelli I. Comparative efficacy and acceptability of atomoxetine, lisdexamfetamine, bupropion and methylphenidate in treatment of attention deficit hyperactivity disorder in children and adolescents: a meta-analysis with focus on bupropion. J Affect Disord. 2015;178:149–59.
Kliegman RM, Stanton BF, Geme JW, Schor NF editors. Nelson textbook of Pediatrics, Elsevier Pubpl 20ieth edition. 2016; pp200–204.
Peters HT, Strange LG, Brown SD, Pond BB. The pharmacokinetic profile of methylphenidate use in pregnancy: A study in mice. Neurotoxicol Teratol. 2016;54:1–4.
Teo S, Khetani V, O'Neil R. Developmental toxicity of d-methylphenidate and dl-methylphenidate in rabbits following oral intubation. Toxicologist. 2001;60:219.
Teo SK, Stirling DI, Hoberman AM, Christian MS, Thomas SD, Khetani VD, et al. Birth Defects Res (Part B). 2003;68:162–71.
Stewart BE, Stump DG, Johnson PA, Working PK. Methylphenidate HCl is not a developmental toxicant in the rat. Toxicologist. 2001;60:219–20.
Beckman DA, Schneider M, Youreneff M, Tse FL. Developmental toxicity assessment of d,l-methylphenidate and d-methylphenidate in rats and rabbits. Birth Defects Res B, Dev Reprod Toxicol. 2008;83:489–501.
Golub M, Costa L, Crofton K, Frank D, Fried P, Gladen B, et al. NTP-CERHR Expert Panel report on the reproductive and developmental toxicity of methylphenidate. Birth Defects Res (B). 2005;74:300–81.
Bolea-Alamanac BM, Green A, Verma G, Maxwell P, Davies SJ. Methylphenidate use in pregnancy and lactation: a systematic review of evidence. Br J Clin Pharmacol. 2014;77(1):96–101.
Debooy VD, Seshia MM, Tenenbein M, Casiro OG. Intravenous pentazocine and methylphenidate abuse during pregnancy. Maternal lifestyle and infant outcome. Am J Dis Child. 1993;147(10):1062–5.
Dideriksen D, Pottegard A, Hallas J, Aagaard L, Damkier P. First trimester exposure to methylphenidate Basic Clin. Pharm Toxicol. 2013;112(2):73–6.
Kallen B, Borg N, Reis M. The use of central nervous system active drugs during pregnancy. Pharmaceuticals. 2013;6(10):1221–86.
Pottegård A, Hallas J, Andersen JT, Løkkegaard EC, Dideriksen D, Aagaard L, et al. First-trimester exposure to methylphenidate: a population-based cohort study. J Clin Psychiatry. 2014;75(1):e88–93.
Haervig KB, Mortensen LH, Hansen AV, Strandberg-Larsen K. Use of ADHD medication during pregnancy from 1999 to 2010: a Danish register-based study. Pharmacoepidemiol Drug Saf. 2014;23(5):526–33.
Diav-Citrin O, Shechtman S, Arnon J, Wajnberg R, Borisch C, Beck E, et al. Methylphenidate in pregnancy: A multicenter, prospective, comparative, observational study. J. Clin. Psychiatry. 2016;77(9):1176–81.
Bro SP, Kjaersgaard MI, Parner ET, Sørensen MJ, Olsen J, Bech BH, et al. Adverse pregnancy outcomes after exposure to methylphenidate or atomoxetine during pregnancy. Clin Epidemiol. 2015;7:139–47.
Hackett LP, Kristensen JH, Hale TW, Paterson R, Ilett KF. Methylphenidate and breast feeding. Ann Pharmacother. 2006;40:1890–1.
Spigset O, Brede WR, Zahken K. Excretion of methylphenidate in breast milk. Am J Psych. 2007;164:348–54.
Schaefer C, Peters P, Miller RK editors: Drugs during pregnancy and lactation, third edition. Elsevier publ. 2015; methylphenidate pp 768–769.
Golub M, Costa L, Crofton K, Frank D, Fried P, Gladen B, et al. NTP-CERHR expert panel report on the reproductive and developmental toxicity of amphetamine and methamphetamine. Birth Defects Res (Part B). 2005;74:471–584.
Nora JJ, Vargo TA, Nora AH, Love KE, McNamara DG. Dexamphetamine: a possible environmental trigger in cardiovascular malformations. Lancet. 1970;1(7659):1290–1.
Milkovich L, Van den Berg BJ. Effects of antenatal exposure to anorectic drugs. Am J Obstet Gynecol. 1977;129:637–42.
Heinonen OP. Birth Defects and Drugs in Pregnancy. Littleton: Publishing Sciences Group Inc; 1977.
Little BB, Snell LM, Gilstrap LC 3rd. Methamphetamine abuse during pregnancy: outcome and fetal effects. Obstet Gynecol. 1988;72:541–4.
Draper ES, Rankin J, Tonks AM, Abrams KR, Field DJ, Clarke M, et al. Recreational drug use: a major risk factor for gastroschisis? Am J Epidemiol. 2008;167(4):485–91.
Felix RJ, Chambers CD, Dick LM, Johnson KA, Jones KL. Prospective pregnancy outcome in women exposed to amphetamines. Teratology. 2000;61:441. Abstract
Wright TE, Schueter R, Tellei J, Sauvage L. Methamphetamine and pregnancy outcome. J Addict Med. 2015;9(2):111–7.
Eriksson M, Larsson G, Zetterström R. Amphetamine addiction and pregnancy II. Pregnancy, delivery and the neonatal period. Socio-medical aspects. Acta Obstet Gynecol Scand. 1981;60:253–9.
Nguyen D, Smith LM, Lagasse LL, Derauf C, Grant P, Shah R, et al. Intrauterine growth of infants exposed to prenatal methamphetamine: results from the infant development, environment, and lifestyle study. J Pediatr. 2010;157(2):337–9.
Smith L, Yonekura ML, Wallace T, Berman N, Kuo J, Berkowitz C. Effects of prenatal metamphetamine exposure on fetal growth and drug withdrawal symptoms in infants born at term. J Dev Behav Ped. 2003;24:17–23.
Gorman MC, Orme KS, Nguyen NT, Kent EJ 3rd, Caughey AB. Outcomes in pregnancies complicated by methamphetamine use. Am J Obstet Gynecol. 2014;211(4):429.e1–7.
Colby JB, Smith L, O'Connor MJ, Bookheimer SY, Van Horn JD, Sowell ER. White matter microstructural alterations in children with prenatal methamphetamine/polydrug exposure. Psychiatry Res. 2012;204(2–3):140–8.
Roos A, Jones G, Howells FM, Stein DJ, Donald KA. Structural brain changes in prenatal methamphetamine-exposed children. Metab Brain Dis. 2014;29(2):341–9.
Derauf C, Lester BM, Neyzi N, Kekatpure M, Gracia L, Davis J, et al. Subcortical and cortical structural central nervous system changes and attention processing deficits in preschool-aged children with prenatal methamphetamine and tobacco exposure. Dev Neurosci. 2012;34(4):327–41.
Roos A, Kwiatkowski MA, Fouche JP, Narr KL, Thomas KG, Stein DJ, et al. White matter integrity and cognitive performance in children with prenatal methamphetamine exposure. Behav Brain Res. 2015;279:62–7.
Chang L, Cloak C, Jiang CS, Farnham S, Tokeshi B, Buchthal S, et al. Altered neurometabolites and motor integration in children exposed to methamphetamine in utero. NeuroImage. 2009;48(2):391–7.
LaGasse LL, Wouldes T, Newman E, Smith LM, Shah RZ, Derauf C, et al. Prenatal methamphetamine exposure and neonatal neurobehavioral outcome in the USA and New Zealand. Neurotoxicol Teratol. 2011;33(1):166–75.
Smith LM, LaGasse LL, Derauf C, Newman E, Shah R, Haning W, et al. Motor and cognitive outcomes through three years of age in children exposed to prenatal methamphetamine. Neurotoxicol Teratol. 2011;33(1):176–84.
Smith LM, Diaz S, LaGasse LL, Wouldes T, Derauf C, Newman E, et al. Developmental and behavioral consequences of prenatal methamphetamine exposure: A review of the Infant Development, Environment, and Lifestyle (IDEAL) study. Neurotoxicol Teratol. 2015;51:35–44.
Ornoy A, Segal J, Bar-Hamburger R, Greenbaum C. The developmental outcome of school age children born to heroin- dependent mothers: Importance of environmental factors. Dev Med Child Neurol. 2001;43:668–75.
Derauf C, LaGasse L, Smith L, Newman E, Shah R, Arria A, et al. Infant temperament and high-risk environment relate to behavior problems and language in toddlers. J Dev Behav Pediatr. 2011;32(2):125–35.
LaGasse LL, Derauf C, Smith LM, Newman E, Shah R, Neal C, et al. Prenatal methamphetamine exposure and childhood behavior at 3 and 5 years of age. Pediatrics. 2012;129(4):681–8.
Derauf C, Lagasse LL, Smith LM, Newman E, Shah R. Neal CR Prenatal methamphetamine exposure and inhibitory control among young school-age children. J Pediatr. 2012;161(3):452–9.
Kirlic N, Newman E, Lagasse LL, Derauf C, Shah R, Smith LM, et al. Cortisol reactivity in two year old children prenatally exposed to metamphetamine. J Stud Alcohol Drugs. 2013;74(3):447–51.
Steiner E, Villén T, Hallberg M, Rane A. Amphetamine secretion in breast milk. Eur J Clin Pharmacol. 1984;27:123–4.
Ayd FJ. Excretion of psychotropic drugs in human milk. Int Drug Ther News Bull. 1973;8:33–40.
Ilett KF, Hackett LP, Kristensen JH, Kohan R. Transfer of dexamphetamine into breast milk during treatment for attention deficit hyperactivity disorder. Br J Clin Pharmacol. 2007;63:371–5.
Schaefer C, Peters P, Miller RK editors: Drugs during pregnancy and lactation, third edition. Elsevier publ. 2015; dexamphetamine pp 836.
Committee on drugs, American Academy of Pediatrics: the transfer of drugs and other chemicals into human breast milk. Pediatrics, 2001; 108:776–789.
Christman AK, Fermo JD, Markowitz JS. Atomoxetine, a novel treatment for attention-deficit-hyperactivity disorder. Pharmacotherapy. 2004;24(8):1020–36.
http://www.accessdata.fda.gov/drugsatfda_docs/nda/2002/21-411_Strattera.cfm, see Pharmacology Reviews.
Boutroy MJ, Gisonna CR, Legagneur M. Clonidine: Placental transfer and neonatal adaption. Early Hum Dev. 1988;17:275–86.
Buchanan ML, Easterling TR, Carr DB, Shen DD, Risler LJ, Nelson WL, et al. Clonidine pharmacokinetics in pregnancy. Drug Metab Dispos. 2009;37(4):702–5.
Rothberger S, Carr D, Brateng D, Hebert M, Easterling TR. Pharmacodynamics of clonidine therapy in pregnancy: a heterogeneous maternal response impacts fetal growth. Am J Hypertens. 2010;23(11):1234–40.
Remuzzi G, Ruggenenti P. Prevention and treatment of pregnancy- associated hypertension: what have we learned in the last 10 years? Am J Kidney Dis. 1991;18(3):285–305.
Horvath JS, Phippard A, Korda A, Henderson-Smart DJ, Child A, Tiller DJ. Clonidine hydrochloride: a safe and effective antihypertensive agent in pregnancy. Obstet Gynecol. 1985;66:634–8.
Tuimala R, Punnonen R, Kauppila E. Clonidine in the treatment of hypertension during pregnancy. Ann Chir Gynaecol. 1985;74(Suppl. 197):47–50.
Tsai TH, Beitman RE, Gibson JP, Larson EJ. Teratologic and reproductive studies of lofexidine. Arzneim Forsch. 1982;32:962–6.
Bamford OS, Dawes GS, Denny R, Ward RA. Effects of the alpha2 – adrenergic agonist clonidine and its antagonist idazoxan on the fetal lamb. J Physiol. 1986;381:29–37.
Ornoy A, Reece AE, Pavlinkova G, Kappen C, Miller RK. Effect of maternal diabetes on the embryo, fetus and children: congenital anomalies, genetic and epigenetic changes and developmental outcomes. Birth Defects Res Part C. 2015;105(1):53–72.
Hartikainen-Sorri AL, Heikkinen JE, Koivisto M. Pharmacokinetics of clonidine during pregnancy and nursing. Obstet Gynecol. 1987;69:598–600.
Sevrez C, Lavocat MP, Mounier G, Elefant E, Magnin S, Teyssier G, et al. Transplacental or breast milk intoxication to clonidine: a case of neonatal hypotonia and drowsiness. Arch Pediatr. 2014;21(2):198–200.
Bunjes R, Schaefer C, Holzinger D. Clonidine and breast-feeding. Clin Pharm. 1993;12:178–9.
Schaefer C, Peters P, Miller RK editors: Drugs during pregnancy and lactation, third edition. Elsevier publ. 2015; Clonidine: pp 203,716.
Huisjes HJ, Hadders-Algra M, Touwen BC. Is clonidine a behavioural teratogen in the human? Early Hum Dev. 1986;14:43–8.
Sayer GR, McGough JJ, Levitt J, Cowen J, Sturm A, Castelo E, et al. Acute and Long-Term Cardiovascular Effects of Stimulant, Guanfacine, and Combination Therapy for Attention-Deficit/Hyperactivity Disorder. J Child Adolesc Psychopharmacology. 2016;26(10):882–8.
Faraone SV, Mcburnett K, Sallee FR, Steeber J, Lopez FA. Guanfacine extended release: a novel treatment for attention-deficit/hyperactivity disorder in children and adolescents. Clin The. 2013;35(11):1778–93.
WWW. Reprotox, Guanfacine. Upated 19 June 2017.
Philipp E. Guanfacine in the treatment of hypertension due to pre-eclamptic toxemia in thirty women. Br J Clin Pharmacol. 1980;10:137S–40S.
Tenex product labeling, 2013.
Fava M, Rush AJ, Thase ME, Clayton A, Stahl SM, Pradko JF, et al. “15 years of clinical experience with bupropion HCl: from bupropion to bupropion SR to bupropion XL”. J Clin Psychiatry 2005;7(3):106–113.
Tha Deang K, Sidi H, Zakaria H, Lope Adam R, Das S, Hazwani Hatta N, et al. The novelty of bupropion as a dopaminergic antidepressant for the treatment of adult attention deficit hyperactive disorder. Curr Drug Targets. 2017; https://doi.org/10.2174/1389450118666170511145628.
The Bupropion Pregnancy Registry. Final report. 1 September 1997 through 31 March 2008. Issued August, 2008. Kendle International, Inc., Wilmington, North Carolina.
Cole JA, Modell JG, Haight BR, Cosmatos IS, Stoler JM, Walker AM. Bupropion in pregnancy and the prevalence of congenital malformations. Pharmacoepidemiol Drug Saf. 2007;16:474–84.
Chun-Fai-Chan B, Koren G, Fayez I, Kalra S, Voyer-Lavinge S, Bosier A, et al. Pregnancy outcome of women exposed to bupropion during pregnancy: a prospective comparative study. Amer J Obstet & Gynecol. 2005;192(3):932–6.
Einarson A, Choi C, Einarson TR, Koren G. Incidence of major malformations in infants following antidepressant exposure in pregnancy: results of a large prospective cohort study. Can J Psychiatr. 2009;54(4):242–6.
Alwan S, Reefhuis J, Botto LD, Rasmussen SA, Correa A, Friedman JM. Maternal use of bupropion and risk for congenital heart defects. Am J Obstet Gynecol. 2010;203(1):52 e1–6.
Louik C, Kerr S, Mitchell AA. First-trimester exposure to bupropion and risk of cardiac malformations. Pharmacoepidemiol Drug Saf. 2014;23(10):1066–75.
Huybrechts KF, Palmsten K, Avorn J, Cohen LS, Holmes LB, Franklin JM, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370:2397–407.
Figueroa R. Use of antidepressants during pregnancy and risk of attention-deficit/hyperactivity disorder in the offspring. J Dev Behav Pediatr. 2010;31(8):641–8.
Baab SW, Peindl KS, Piontek CM, Wisner KL. Serum bupropion levels in 2 breastfeeding mother-infant pairs. J Clin Psychiatry. 2002;63:910–1.
Haas JS, Kaplan CP, Barenboim D, Jacob P 3rd, Benowitz NL. Bupropion in breast milk: an exposure assessment for potential treatment to prevent post-partum tobacco use. Tob Control. 2004;13:52–6.
www.reprotox: bupropion; updated Sept 2017.
Schaefer C, Peters P, Miller RK editors: Drugs during pregnancy and lactation, third edition. Elsevier publ. 2015; Bupropion: pp 555,745,763.
Ornoy A, Koren G. Selective Serotonin Reuptake Inhibitors during pregnancy: do we have now more definite answers related to prenatal exposure. Birth Defects Res Part C. 2017;109(12):898–908.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editor: Sara Eyal
Rights and permissions
About this article
Cite this article
Ornoy, A. Pharmacological Treatment of Attention Deficit Hyperactivity Disorder During Pregnancy and Lactation. Pharm Res 35, 46 (2018). https://doi.org/10.1007/s11095-017-2323-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-017-2323-z