Abstract
Purpose
To predict the cellular-level epithelial absorbed dose from deposited inhaled corticosteroid (ICS) particles in a model of an expanding and contracting small airway segment for different particle forms.
Methods
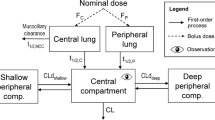
A computational fluid dynamics (CFD)-based model of drug dissolution, absorption and clearance occurring in the surface liquid of a representative small airway generation (G13) was developed and used to evaluate epithelial dose for the same deposited drug mass of conventional microparticles, nanoaggregates and a true nanoaerosol. The ICS medications considered were budesonide (BD) and fluticasone propionate (FP). Within G13, total epithelial absorption efficiency (AE) and dose uniformity (microdosimetry) were evaluated.
Results
Conventional microparticles resulted in very poor AE of FP (0.37%) and highly nonuniform epithelial absorption, such that <5% of cells received drug. Nanoaggregates improved AE of FP by a factor of 57-fold and improved dose delivery to reach approximately 40% of epithelial cells. True nanoaerosol resulted in near 100% AE for both drugs and more uniform drug delivery to all cells.
Conclusions
Current ICS therapies are absorbed by respiratory epithelial cells in a highly nonuniform manner that may partially explain poor clinical performance in the small airways. Both nanoaggregates and nanoaerosols can significantly improve ICS absorption efficiency and uniformity.










Similar content being viewed by others
References
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of COPD. 2014. http://www.goldcopd.org/.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2016. http://ginasthma.org/2016-gina-report-global-strategy-for-asthma-management-and-prevention/.
Rubin BK, Fink JB. Novel medications for asthma: a look at the future. Expert Opin Investig Drugs. 2007;16:889–97.
The Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromial in children with asthma. New England J Med. 2000;343:1054–63.
Contoli M, Bousquet J, Fabbri LM, Magnussen H, Rabe KF, Siafakas NM, et al. The small airways and distal lung compartment in asthma and COPD: a time for reappraisal. Allergy. 2010;65:141–51.
Barnes PJ. Severe asthma: advances in current management and future therapy. J Allergy Clin Immunol. 2012;129:48–59.
Usmani OS, Barnes PJ. Assessing and treating small airways disease in asthma and chronic obstructive pulmonary disease. Ann Med. 2012;44:146–56.
Sumi Y, Hamid Q. Airway remodeling in asthma. Allergol Int. 2007;56:341–8.
Chapman KR, Boulet LP, Rea RM, Franssen E. Suboptimal asthma control: prevalence, detection and consequences in general practice. Eur Respir J. 2008;31:320–5.
Croisant S. Epidemiology of asthma: Revalence and burden of disease. In: Brasier AR, editor. Heterogeneity in Asthma. New York: Springer; 2014.
Usmani OS, Singh D, Spinola M, Bizzi A, Barnes PJ. The prevalence of small airways disease in adult asthma: a systematic literature review. Respir Med. 2016;116:19–27.
Van den Berge M, Ten Hacken NHT, Van der Wiel E, Postma DS. Treatment of the bronchial tree from beginning to end: targeting small airway inflammation in asthma. Allergy. 2013;68:16–26.
Walenga RL, Longest PW. Current inhalers deliver very small doses to the lower tracheobronchial airways: assessment of healthy and constricted lungs. J Pharm Sci. 2016;105:147–59.
Wagner EM, Liu MC, Weinmann GG, Permutt S, Bleecker ER. Peripheral lung resistance in normal and asthmatic subjects. Am Rev Respir Dis. 1990;141:584.
Tgavalekos NT, Tawhai M, Harris RS, Mush G, Vidal-Melo M, Venegas JG, et al. Identifying airways responsible for heterogeneous ventilation and mechanical dysfunction in asthma: an image functional modeling approach. J Appl Physiol. 2005;99:2388–97.
Manoharan A, Anderson WJ, Lipworth J, Ibrahim I, Lipworth BJ. Small airway dysfunction is associated with poorer asthma control. Eur Respir J. 2014;44:1353–5.
Berry M, Hargadon B, Morgan A, Shelley M, Richter J, Shaw D, et al. Alveolar nitric oxide in adults with asthma: evidence of distal lung inflammation in refractory asthma. Eur Respir J. 2005;25:986–91.
Gelb AF, Taylor CF, Nussbaum E, Gutierrez C, Schein A, Shinar CM, et al. Alveolar and airway sites of nitric oxide inflammation in treated asthma. Am J Respir Crit Care Med. 2004;170:737–41.
Verbanck S, Schuermans DL, Paiva M, Vincken W. The functional benefit of anti-inflammatory aerosols in the lung periphery. J Allergy Clin Immunol. 2006;118:340–6.
Goldin JG, Tashkin DP, Kleerup EC, Greaser LE, Haywood UM, Sayre JW, et al. Comparative effects of hydrofluoroalkane and chlorofluorocarbon beclomethasone dipropionate inhalation on small airways: assessment with functional helical thin-section computed tomography. J Allergy Clin Immunol. 1999;104:s258–67.
Yamaguchi M, Niimi A, Ueda T, Takemura M, Matsuoka H, Jinnai M, et al. Effect of inhaled corticosteroids on small airways in asthma: investigation using impulse oscillometry. Pulm Pharmacol Ther. 2009;22:326–32.
Hoshino M. Comparison of effectiveness in ciclesonide and fluticasone propionate on small airway function in mild asthma. Allergol Int. 2010;59:59–66.
Tian G, Longest PW, Su G, Walenga RL, Hindle M. Development of a stochastic individual path (SIP) model for predicting the tracheobronchial deposition of pharmaceutical aerosols: effects of transient inhalation and sampling the airways. J Aerosol Sci. 2011;42:781–99.
Longest PW, Tian G, Walenga RL, Hindle M. Comparing MDI and DPI aerosol deposition using in vitro experiments and a new stochastic individual path (SIP) model of the conducting airways. Pharm Res. 2012;29:1670–88.
Longest PW, Tian G, Delvadia R, Hindle M. Development of a stochastic individual path (SIP) model for predicting the deposition of pharmaceutical aerosols: effects of turbulence, polydisperse aerosol size, and evaluation of multiple lung lobes. Aerosol Sci Technol. 2012;46:1271–85.
Khajeh-Hosseini-Dalasm N, Longest PW. Deposition of particles in the alveolar airways: inhalation and breath-hold with pharmaceutical aerosols. J Aerosol Sci. 2015;79:15–30.
Tian G, Hindle M, Lee S, Longest PW. Validating CFD predictions of pharmaceutical aerosol deposition with in vivo data. Pharm Res. 2015;32:3170–87.
Longest PW, Tian G, Khajeh-Hosseini-Dalasm N, Hindle M. Validating whole-airway CFD predictions of DPI aerosol deposition at multiple flow rates. J Aerosol Med Pulm Drug Deliv. 2016; doi:10.1089/jamp.2015.1281.
Longest PW, Holbrook LT. In silico models of aerosol delivery to the respiratory tract - Development and applications. Adv Drug Deliv Rev. 2012;64:296–311.
Patton JS, Brain JD, Davies LA, Fiegel J, Gumbleton M, Kim KJ, et al. The particle has landed-characterizing the fate of inhaled pharmaceuticals. J Aerosol Med Pulm Drug Deliv. 2010;23:S71–87.
Kuehl C, El-Gendy N, and Berkland C. NanoClusters surface area allows nanoparticle dissolution with microparticle properties. J Pharm Sci 2014;103:1787–1798.
Siepmann J, Siepmann F. Modeling of diffusion controlled drug delivery. J Control Release. 2012;161:351–62.
Ritger PL, Peppas NA. A simple equation for description of solute release I. Fickian and non-Fickian release from non-swellable devices in the form of slabs, spheres, cylinders or discs. J Control Release. 1987;5:23–36.
Sakagami M. In vivo, in vitro and ex vivo models to assess pulmonary absorption and disposition of inhaled therapeutics for systemic delivery. Adv Drug Deliv Rev. 2006;58:1030–60.
Arora D, Shah KA, Halquist MS, Sakagami M. In vitro aqueous fluid-capacity-limited dissolution testing of respirable aerosol drug particles generated from inhaler products. Pharm Res. 2010;27:786–95.
Bur M, Huwer H, Muys L, Lehr C-M. Drug transport across pulmonary epithelial cell monolayers: effects of particle size, apical liquid volume, and deposition technique. J Aerosol Med Pulm Drug Deliv. 2010;23:119–27.
Wiedmann TS, Bhatia R, Wattenberg LW. Drug solubilization in lung surfactant. J Control Release. 2000;65:43–7.
Buttini F, Miozzi M, Balducci AG, Royall PG, Brambilla G, Colombo P, et al. Differences in physical chemistry and dissolution rate of solid particle aerosols from solution pressurised inhalers. Int J Pharm. 2014;465:42–51.
Blume C, Davies DE. In vitro and ex vivo models of human asthma. Eur J Pharm Biopharm. 2013;84:394–400.
Rygg A, Hindle M, Longest PW. Absorption and clearance of pharmaceutical aerosols in the human nose: effects of nasal spray suspension particle size and properties. Pharm Res. 2016;33:909–21.
Rygg A, Hindle M, Longest PW. Linking suspension nasal spray drug deposition patterns to pharmacokinetic profiles: a proof-of-concept study using computational fluid dynamics. J Pharm Sci. 2016;105:1995–2004.
Rygg A, Longest PW. Absorption and clearance of pharmaceutical aeorsols in the human nose: Development of a CFD model. J Aerosol Med Pulm Drug Deliv. 2015; doi:10.1089/jamp.2015.1252.
Shah SA, Berger RL, McDermott J, Gupta P, Monteith D, Connor A, et al. Regional deposition of mometasone furoate nasal spray suspension in humans. Allergy Asthma Proceed. 2015;36:48–57.
Longest PW, Vinchurkar S, Martonen TB. Transport and deposition of respiratory aerosols in models of childhood asthma. J Aerosol Sci. 2006;37:1234–57.
Xi J, Longest PW, Martonen TB. Effects of the laryngeal jet on nano- and microparticle transport and deposition in an approximate model of the upper tracheobronchial airways. J Appl Physiol. 2008;104:1761–77.
Xi J, Longest PW. Evaluation of a novel drift flux model for simulating submicrometer aerosol dynamics in human upper tracheobronchial airways. Ann Biomed Eng. 2008;36:1714–34.
Zhang Z, Kleinstreuer C, Donohue JF, Kim CS. Comparison of micro- and nano-size particle depositions in a human upper airway model. J Aerosol Sci. 2005;36:211–33.
Shi H, Kleinstreuer C, Zhang Z, Kim CS. Nanoparticle transport and deposition in bifurcating tubes with different inlet conditions. Phys Fluids. 2004;16:2199–213.
Balashazy I, Hofmann W, Heistracher T. Computation of local enhancement factors for the quantification of particle deposition patterns in airway bifurcations. J Aerosol Sci. 1999;30:185–203.
Schroeter JD, Kimbell JS, Gross EA, Willson GA, Dorman DC, Tan Y-M, et al. Application of physiological computational fluid dynamics models to predict interspecies nasal dosimetry of inhaled acrolein. Inhal Toxicol. 2008;20:227–43.
Corley RA, Kabilan S, Kuprat AP, Carson JP, Minard KR, Jacob RE, et al. Comparative computational modeling of airflows and vapor dosimetry in the respiratory tracts of rat, monkey, and human. Toxicol Sci. 2012;128:500–16.
Tian G, Longest PW. Application of a new dosimetry program TAOCS to assess transient vapor absorption in the upper airways. Inhal Toxicol. 2010;22:1047–63.
Kimbell JS, Overton JH, Subramaniam RP, Schlosser PM, Morgan KT, Conolly RB, et al. Dosimetry modeling of inhaled formaldehyde: binning nasal flux predictions for quantitative risk assessments. Toxicol Sci. 2001;64:111–21.
Cohen Hubal EA, Schlosser PM, Conolly RB, Kimbell JS. Comparison of inhaled formaldehyde dosimetry predictions with DNA-protein cross-link measurements in the rat nasal passages. Toxicol Appl Pharmacol. 1997;143:47–55.
Daley-Yates P, Kunka R, Yin Y, Andrews S, Callejas S, Ng C. Bioavailability of fluticasone propionate and mometasone furoate aqueous nasal sprays. Eur J Clin Pharmacol. 2004;60:265–8.
El-Gendy N, Gorman EM, Munson EJ, Berkland C. Budesonide nanoparticle agglomerates as dry powder aerosols with rapid dissolution. J Pharm Sci. 2009;98:2731–46.
El-Gendy N, Pornputtapitak W, Berkland C. Nanoparticle agglomerates of fluticasone propionate in combination with albuterol sulfate as dry powder aerosols. Eur J Pharm Sci. 2011;44:522–33.
Finlay WH. The mechanics of inhaled pharmaceutical aerosols. San Diego: Academic Press; 2001.
Wanner A, Salathe M, O'Riordan TG. Mucociliary clearance in the airways. Am J Respir Crit Care Med. 1996;154:1868–902.
ICRP. Human respiratory tract model for radiological protection. New York: Elsevier Science Ltd.; 1994.
Knowles MR, Boucher RC. Mucus clearance as a primary innate defense mechanism for mammalian airways. J Clin Invest. 2002;109:571–7.
Van As A. Pulmonary airway clearance mechanisms: a reappraisal. Am Rev Respir Dis. 1977;115:721–6.
Sturm R, Hofmann W. Stochastic modeling predictions for the clearance of insoluble particles from the tracheobronchial tree of the human lung. Bull Math Biol. 2007;69:395–415.
Sung JC, Pulliam BL, Edwards DA. Nanoparticles for drug delivery to the lungs. Trends Biotechnol. 2007;25:563–70.
Kuehl C, El-Gendy N, Berkland C. NanoClusters surface area allows nanoparticle dissolution with microparticle properties. J Pharm Sci. 2014;103:1787–98.
Lai SK, Wang Y-Y, Hanes J. Mucus-penetrating nanoparticles for drug and gene delivery to mucosal tissues. Adv Drug Deliv Rev. 2009;61:158–71.
Longest PW, Kleinstreuer C. Computational models for simulating multicomponent aerosol evaporation in the upper respiratory airways. Aerosol Sci Technol. 2005;39:124–38.
Longest PW, Hindle M. CFD simulations of enhanced condensational growth (ECG) applied to respiratory drug delivery with comparisons to in vitro data. J Aerosol Sci. 2010;41:805–20.
Longest PW, Kleinstreuer C, Buchanan JR. Efficient computation of micro-particle dynamics including wall effects. Comput Fluids. 2004;33:577–601.
Morsi SA, Alexander AJ. An investigation of particle trajectories in two-phase flow systems. J Fluid Mech. 1972;55:193–208.
Longest PW, Xi J. Effectiveness of direct Lagrangian tracking models for simulating nanoparticle deposition in the upper airways. Aerosol Sci Technol. 2007;41:380–97.
Longest PW, Tian G, Li X, Son Y-J, Hindle M. Performance of combination drug and hygroscopic excipient submicrometer particles from a softmist inhaler in a characteristic model of the airways. Ann Biomed Eng. 2012;40:2596–610.
Clift R, Grace JR, Weber ME. Bubbles, drops, and particles. New York: Academic Press; 1978.
Longest PW, Hindle M. Evaluation of the Respimat soft mist inhaler using a concurrent CFD and in vitro approach. J Aerosol Med Pulm Drug Deliv. 2009;22:99–112.
Leach CL, Davidson PJ, Hasselquist BE, Boudreau RJ. Lung deposition of hydrofluoroalkane-134a beclomethasone is greater than that of chlorofluorocarbon fluticasone and chlorofluorocarbon beclomethasone: a cross-over study in healthy volunteers. CHEST Journal. 2002;122:510–6.
Leach CL, Davidson PJ, Hasselquist BE, Boudreau RJ. Influence of particle size and patient dosing technique on lung deposition of HFA-beclomethasone from a metered dose inhaler. J Aerosol Med. 2005;18:379–85.
Usmani OS, Biddiscombe MF, Barnes PJ. Regional lung deposition and bronchodilator response as a function of beta(2)-agonist particle size. Am J Respir Crit Care Med. 2005;172:1497–504.
Newman SP. Use of gamma scintigraphy to evaluate the performance of new inhalers. J Aerosol Med. 1999;12:S25–31.
Newman S, Salmon A, Nave R, Drollmann A. High lung depostion of 99mTc-labeled ciclesonide administered via HFA-MDI to patients with asthma. Respir Med. 2006;100:375–84.
Tian G, Longest PW, Li X, Hindle M. Targeting aerosol deposition to and within the lung airways using excipient enhanced growth. J Aerosol Med Pulm Drug Deliv. 2013;26:248–65.
Tian G, Hindle M, Longest PW. Targeted lung delivery of nasally administered aerosols. Aerosol Sci Technol. 2014;48:434–49.
Usmani OS. Treating the small airways. Respiration. 2012;84:441–53.
Fu HJ, Patel AC, Holtzman MJ, Chen DR. A new electrospray aerosol generator with high particle transmission efficiency. Aerosol Sci Technol. 2011;45:1176–83.
Longest PW, Vinchurkar S. Inertial deposition of aerosols in bifurcating models during steady expiratory flow. J Aerosol Sci. 2009;40:370–8.
Zhang Z, Kleinstreuer C, Kim CS. Airflow and nanoparticle deposition in a 16-generation tracheobronchial airway model. Ann Biomed Eng. 2008;36:2095–110.
Zhang Z, Kleinstreuer C. Computational analysis of airflow and nanoparticle deposition in a combined nasal-oral-tracheobronchial airway model. J Aerosol Sci. 2011;42:174–94.
Kolanjiyil AV, Kleinstreuer C. Nanoparticle mass transfer from lung airways to systemic regions-part I: whole-lung Aerosol dynamics. J Biomech Eng. 2013;135:121003.
Geiser M, Schurch S and Gehr P. Influence of surface chemistry and topography of particles on their immersion into the lung's surface-lining layer J Appl Physiol 2003;94:1793–1801.
Martonen TB, Katz IM. Deposition patterns of aerosolized drugs within human lungs - effects of Ventilatory parameters. Pharm Res. 1993;10:871–8.
Hilding AC. Ciliary streaming in the lower respiratory tract. Am J Physiol--Legacy Content. 1957;191:404–10.
Tian G, Longest PW. Development of a CFD boundary condition to model transient vapor absorption in the respiratory airways. ASME J Biomech Eng. 2010;132:051003.
Acknowledgments and Disclosures
Alex Rygg is gratefully acknowledged for developing a previous version of the CFD-based DAC model while working as a postdoc in the Longest Lab at VCU. This study was supported by Award U01 FD004570 from the US FDA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the US FDA. The authors are developing techniques for pharmaceutical nanoparticle production and improved small airway targeting, which if licensed, may provide a future financial interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Longest, P.W., Hindle, M. Small Airway Absorption and Microdosimetry of Inhaled Corticosteroid Particles after Deposition. Pharm Res 34, 2049–2065 (2017). https://doi.org/10.1007/s11095-017-2210-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-017-2210-7