Abstract
Background The prognosis of patients with glioblastoma is very poor with a mean survival of 10–12 months. Currently available treatment options are multimodal, which include surgery, radiotherapy, and chemotherapy. However, these have been shown to improve survival only marginally in glioblastoma multiforme (GBM) patients. Methylated methylguanine methyltransferase (MGMT) promoter is correlated with improved progression-free and overall survival in patients treated with alkylating agents. Strategies to overcome MGMT-mediated chemoresistance are being actively investigated. Methods A retrospective analysis on 160 adult patients (≥16 years) treated for histologically confirmed GBM between 2003 and 2005 at our Institution was performed. All patients were treated with conventional fractionated radiotherapy and a combined chemotherapy treatment with Cisplatin (CDDP) (100 mg/sqm on day 1) and carmustine (BCNU) (160 mg/sqm on day 2); the treatment was repeated every 6 weeks for five cycles. Toxicity, progression free survival and overall survival were assessed. Results The median number of chemotherapy cycles delivered to each patient was 5 (range 3–6), with no patients discontinuing treatment because of refusal or toxicity. Dose reduction was required in 16 patients (10%), and all patients completed radiotherapy, whereas 5 patients discontinued chemotherapy before completing all planned cycles for disease progression. The primary toxicities were: neutropenia (grade 3–4: 23%), thrombocytopenia (grade 3–4: 18.5%), and nausea and vomiting (13%). Median progression-free survival times and 1-year progression free survival were 7.6 months (95% CI 6.6–8.5) and 17.3%, respectively. OS was 15.6 months (95% CI 14.1–17.1). Conclusions Our results for PFS and overall survival are comparable with those obtained with temozolomide, but the toxicity occurring in our series was more frequent and persistent. The toxicity, and mainly the modalities of administration associated with cisplatin and BCNU combination, argues against future use in the treatment of patients with GBM.
Similar content being viewed by others
Introduction
Glioblastoma multiforme (GBM) is among the most devastating and intractable of all brain tumors, and is associated with a median survival ranging from 12 to 15 months. Survival for patients with GBM has improved with the addition of temozolomide chemotherapy to post-operative radiotherapy. However, molecular studies have demonstrated that the benefit is mainly observed in patients whose tumors have a methylated methylguanine methyltransferase (MGMT) gene promoter, and are thus unable to repair some of the chemotherapy-induced DNA damage [1].
For those patients whose tumors are not MGMT methylated, alternative treatments with a different mechanism of action or methods of inhibiting MGMT should be developed.
The human MGMT gene is inducible by glucocorticoids, radiation and alkylating agents, although the role of this induction in the development of chemotherapeutic alkylating drug resistance remains unclear [2]. Modulation of MGMT expression in tumors and normal tissue is currently being investigated as a possible strategy for improving cancer therapy. Clinical findings and laboratory results suggest that platinum compounds may play a role in the down-regulation of MGMT mRNA expression as well as up-regulation of sensitivity to nitrosourea [3, 4]. In this context, it is of interest to review the results obtained by a combination of cisplatinum (CDDP) and carmustine (BCNU) administered in the first-line management of patients with GBM. In this study, we report both the safety and clinical results of CDDP and BCNU in combination in a homogenous group treated at our Institute before the temozolomide era.
Patients and methods
One hundred and sixty adult patients (≥16 years) treated for histologically confirmed GBM between 2003 and 2005 at the Fondazione IRCCS Istituto Neurologico Carlo Besta of Milan, Italy, were included in this retrospective analysis.
At the start of treatment, contraindications to inclusion were: active or uncontrolled infections, other malignancy, prior cranial radiation, chemotherapy or immunotherapy for a brain tumor, Karnofsky Performance Status (KPS) <70, significant history of congestive heart failure, pregnancy or lactation, or other significant medical or psychiatric illness that would preclude secure administration of combination therapy.
Data were collected from patients’ charts for analysis of the following items: demographic characteristics, histology, postoperative KPS, type of surgery, antiepileptic treatments, radio- and chemotherapy, side effects (graded according to the Common Terminology Criteria for Adverse Events; CTCAE version 3.0), PFS, OS, patterns of recurrence and treatment of recurrent disease.
Progression-free survival was calculated from the day of the first tumor surgery–biopsy until the demonstration of tumor progression on neuroimaging according to the Macdonald criteria or until the day of last follow-up without progression. Overall survival was assessed from the time of first operation. Survival curves were constructed according to Kaplan and Meier. The influence of different therapy-independent factors (female vs male, age less than 50 years, quality of surgery) on time to tumor progression and overall survival was determined using univariate Cox proportional hazards analyses.
Treatment scheme
Chemotherapy
-
A)
Cisplatin (100 mg/sq m over 2 h intravenous infusion) was administered on day 1, with 2,500 ml hydration of saline solution with 40 mEq KCl, 40 mEq MgSO4, 125 ml mannitol 18%, and 25 mg furosemide. Antiemetic prophylaxis consisted of ondasteron (4 mg) plus alizapride (200 mg) and dexamethazone (8 mg).
-
B)
BCNU (160 mg/sq m over 90 min intravenous infusion) was administered on day 2, with 500 ml hydration of glucosate solution. Antiemetic prophylaxis for the second day of chemotherapy consisted of ondasteron (4 mg). The treatment was repeated every 6 weeks for five cycles. The median time from surgery–biopsy to the start of chemotherapy was 10 days (range 4–15).
Radiotherapy
All patients were treated with conventional fractionated radiotherapy, which consisted of 1.8–2.0 grays (Gy) administered daily, with a median tumor dose of 60 Gy (range 59–61 Gy). Radiotherapy was delivered to the gross tumor volume with a 2- to 3-cm margin for the clinical target volume. Treatment was planned with dedicated computed tomography (CT) and three-dimensional planning systems; focal radiotherapy was delivered with linear accelerators with nominal energy of 6 MV. No patients were treated with stereotactic radiotherapy. The median time from surgery–biopsy to the start of radiotherapy was 28 days (range 22–41) (Fig. 1).
Radiotherapy and chemotherapy were not administered contemporarily: in particular, radiotherapy started after the first cycle of chemotherapy. The second cycle of chemotherapy was started at the end of the radiotherapy.
The protocol was approved by our Institutional Review Board and each patient provided written informed consent before initiation of treatment.
Results
One hundred and sixty patients (110 men and 50 women) aged 18–68 years (mean age 52.9 years) with primary GBM (Table 1) were treated with a combination of cisplatin and BCNU. Tumor locations (including multilobar tumors = 46) were as follows: frontal lobe (n = 44), temporal lobe (n = 24), parietal lobe (n = 14), occipital lobe (n = 12), insula (n = 8), and thalamus (n = 4).
Patients' performance status (Karnofsky scale) ranged from 70 to 100 (median 80) at the time of start of chemotherapy. In total, 87.5% of patients (140/160) received anticonvulsant therapy involving only non-enzyme inductor antiepileptic drugs (NEIAD) (levetiracetam, valproate, topimarate, lamotrigine). Almost all patients received steroids at the initiation of chemotherapy; the median dosage of dexamethasone was 8 mg/day.
Regarding surgery, 4 patients (2.5%) underwent biopsy only, and of the remaining 156 patients, 46.4 and 26.2% underwent total-gross and partial resection, respectively (Table 1).
The median number of chemotherapy cycles delivered to each patient was 5 (range 3–6), with no patients discontinuing treatment because of refusal or toxicity. Dose reduction was required in 16 patients (10%), and all patients completed radiotherapy, whereas 5 patients discontinued chemotherapy before completing all planned cycles for disease progression.
Toxicity
Treatment-related toxicities are listed in Table 2. The primary toxicities were: neutropenia (grade 3–4: 23%), thrombocytopenia (grade 3–4: 18.5%) and nausea and vomiting (13%).
Four patients developed G3 anemia and required treatment with erythropoietin alpha.
Hearing loss and sensory neuropathy were observed in 8% (13/160) of the patients, but they were mild and generally not clinically significant.
We did not observe pulmonary toxicity or neurocortical deterioration attributed to treatment. However, the short survival of patients with GBM and the absence in this study of a systematic neurocognitive assessment do not permit conclusions concerning potential delayed neurocognitive toxicity.
Progression-free survival
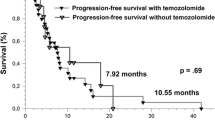
Median progression-free survival times and 1-year progression free survival were 7.6 months (95% CI 6.6–8.5) and 17.3%, respectively (Table 3, Fig. 2).
At recurrence, 20 patients underwent a second surgery and all patients were treated by a second line temozolomide-based chemotherapy.
Overall survival
OS was 15.6 months (95% CI 14.1–17.1), and 81% (95% CI 71–93%) and 44% (95% CI 31–63%) of the patients were alive at 6 and 12 months, respectively (Table 3, Fig. 2).
None of the tested prognostic factors were significantly associated with survival.
Discussion
In 2005, a large phase III trial was completed in Europe and Canada on newly diagnosed patients with GBM, randomised to either radiation alone or radiation with concomitant temozolomide (TMZ, 75 mg/sq m/day) followed by six cycles of conventional TMZ (150–200 mg/sq m/day for 5 days, each month) [5]. This study demonstrated a significant benefit of TMZ plus radiotherapy versus radiotherapy alone on median survival and survival at 2 years. Actually, on the basis of these results, temozolomide in combination with radiotherapy has become the “gold standard” therapy for patients with GBM at first diagnosis. In Italy, temozolomide was permitted for use in patients with primary GBM in 2005. In the present study, we reported a series of 160 patients with GBM treated at our institution between 2003 and 2005, before the worldwide acceptance of temozolomide use. This group of patients were treated by a combination of cisplatin and BCNU.
Nitrosoureas and particularly BCNU were the mainstay of GBM treatment for more than 30 years before the availability of temozolomide. Carmustine was generally used as adjuvant treatment after radiotherapy (RT) [6–8]. Several trials investigated the combination of carmustine and TMZ, but unfortunately with frequently severe, prolonged and cumulative hematotoxicity as the main limitation [9, 10].
Cisplatin administered concurrently with RT has resulted in improved survival in patients with solid tumors. Several studies have suggested that cisplatin has the same anti-tumor effects as those observed in malignant glioma patients [11].
In the past, we reported on three studies using platinum-based chemotherapy in the treatment of anaplastic astrocytoma, and for both primary and recurrent GBM [12, 13]. These studies demonstrated an acceptable toxicity profile when platinum was combined both with nitrosourea or temozolomide. In addition, results in terms of response and PFS were interesting, in particular regarding the salvage treatment of recurrent GBM by a combination of cisplatinum and temozolomide [13, 14].
In the study described here, a clinical benefit was suggested for cisplatinum and BCNU combination, with progression-free survival and overall survival times of 7.6 and 15.6 months, respectively (Table 3).
These results are very close to the results reported by Stupp et al. [5] using temozolomide as adjunctive and concomitant treatment with surgery and external beam radiotherapy in newly diagnosed patients with GBM. Unfortunately, encouraging results have been frequently reported in non-randomised studies, but only a few phase III studies have demonstrated some advantages for chemotherapy in patients with GBM.
Recently, Buckner et al. [15] reported the results of a phase III study, comparing carmustine and cisplatin versus carmustine alone in patients with primary GBM treated with radiotherapy. In this study, cisplatin and BCNU administered before and during RT demonstrated no clinically significant improvement in survival compared with BCNU or RT alone. Moreover, the combination was associated with significant toxicity. Median progression-free survival times and median survival time were considered substandard at 6.2 and 10.4 months, respectively, and the 2-year survival rates were lower (12.9%) than reported in an EORTC-NCI trial [15]. In our study, we observed a relatively long period of survival after disease progression (approximately 8 months). This extended survival could reflect patient selection, but also the partial efficacy of salvage treatments. At recurrence, a large percentage of our patients were reoperated and the whole group of recurrent patients were treated with temozolomide (150–200 mg/sq m days 1–5 every 28 days). This is interesting, because it suggests that temozolomide could maintain this activity, with a good profile of toxicity, as well as in patients previously treated with nitrosourea. On the contrary, the use of nitrosoureas as salvage chemotherapy after temozolomide treatment was reported to be frequently associated with severe toxicities [16].
Focusing on the Buckner trial, an additional factor could have contributed to the limited activity of the BCNU and CDDP combination; notably, in this study, more than 65% of the patients were treated with enzyme-inducing antiepileptic drugs (EIAD) [15]. It is well known that the simultaneous administration of CYP3A-inducing antiepileptics impairs chemotherapy CNS delivery, and alters pharmacokinetic metabolism leading to an inadequate intratumoral drug concentration [17]. Conversely, in our series, all patients were treated with non enzyme-inducing antiepileptic drugs (NIAED) and principally with VPA (70). In this regard, some authors have suggested a potential antitumour role of VPA in GBM tumor cells [18].
Recently, Sher et al. [19] reported the result of a retrospective study designed to determine the relative contribution of concomitant temozolomide in newly diagnosed patients with GBM treated by concurrent and adjuvant TMZ versus adjuvant TMZ alone. In this study, concurrent and adjuvant TMZ was associated with improved survival compared to adjuvant TMZ alone, highlighting the potentiation of radiation effect by temozolomide. Both cisplatinum and BCNU are not suitable for prolonged administration during conventional radiotherapy and this could lead to a theoretical limitation in their efficacy [19].
The dilemma of expected survival gain versus treatment toxicity and relative impact upon QOL remains a crucial point for all chemotherapy treatments [20, 21]. in the EORTC-NCIC trial [5], grade 3/4 hematological toxicity was observed in only 7% of patients during concomitant temozolomide and radiotherapy treatment and in 14% of patients during adjuvant temozolomide treatment. Over the entire study period, grade 3/4 hematologic toxicity included: leukopenia in 7%, thrombocytopenia in 12% and anemia in 1%, respectively.
There was no evidence of cumulative hematological toxicity and only 9% of therapy cycles required a dose reduction, basically due to thrombocytopenia. Nausea and vomiting usually were well controlled by standard antiemetic prophylaxis.
Temozolomide treatment was very well tolerated in comparison to other alkylating agents, although, as for temozolomide, there are few studies on long-term toxicity.
In our study, the limiting side effects were of a haematologic nature. Grade 3–4 leukopenia and thrombocytopenia were observed in 23 and 18.5% of the patients, respectively; however, only 5% of the patients developed grade 4 toxicity. Reasonably, the most significant haematological toxicities (i.e., leukopenia, thrombocytopenia) were related to the BCNU administration, but interestingly the incidence of these side effects was lower than reported using monotherapy BCNU. In effect, in this study BCNU was administered at a lower dose (160 mg/sqm) in comparison to the dose usually prescribed for monotherapy (240 mg/sq m) and this could be the reason for the relatively low incidence of severe haematological toxicity.
In addition, the nausea and vomiting frequently associated with cisplatin-based schedules were not observed in our patients, as these symptoms can be problematic and long lasting with 5-HT 3R-antagonists prophylaxis.
Neurotoxicities related to cisplatin were observed in only 13 patients, but both ototoxicity and sensory neuropathy were mild and generally clinically insignificant. The development of neuropathy was cumulative and dose-related [22]. In our group of patients, electrophysiological examination was performed only in symptomatic patients and demonstrated decreased sensory nerve action potential amplitude with relatively preserved conduction velocities and motor responses.
Neurocognitive outcomes are being increasingly incorporated into recent clinical trials [23], but unfortunately, in this retrospective series, neurocognitive battery tests were not systematically included in clinical examination, and thus, an appropriate interpretation of this aspect was impossible. However, late neurotoxicity could become a greater concern if chemotherapy should be used in patients who have a more favourable prognosis in terms of survival.
Lamers et al. [24] reported the result of a study comparing the cost-effectiveness of concomitant and adjuvant temozolomide + RT for the treatment of patients with GBM versus initial radiotherapy alone. In this study, the total amount for drugs, procedures, laboratory, imaging, radiotherapy, and hospital expenses per day were analysed. The authors reported a cost of €37,361 per life-year gained. Despite the high TMZ acquisition costs, the costs per life-year gained are basically comparable to several other accepted first-line treatments with chemotherapy in cancer patients [24]. In our study, we did not perform a cost analysis, but if it is reasonable to consider worldwide similar costs for laboratory tests, imaging and radiotherapy, our combination requires hospital admission of the patients every 6 weeks and this reflects an objective rise in hospital and social costs.
Moreover, the hospital admission and the i.v. administration of the two agents, that requires a strong hydration, represents a distress for both patients and care givers.
In summary, our results for PFS and overall survival are in effect comparable with those obtained with temozolomide, but the toxicity occurring in our series was more frequent and persistent. The toxicity, and mainly the modalities of administration associated with cisplatin and BCNU combination, argues against future use in the treatment of patients with GBM.
Further research has supported the effectiveness of temozolomide, but we also believe in alternative chemotherapeutic agents. The crucial point for the development of both new studies and combinations will be represented by investigation into particular areas such as genetic markers, patient and carer quality of life, and in patient views on survival advantages versus treatment disadvantages.
References
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JE, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R (2005) MGMT gene silencing and benefit from temozolomide in GBM. N Engl J Med 352(10):997–1003. doi:10.1056/NEJMoa043331
Kaina B, Christmann M, Naumann S, Roos WP (2007) MGMT: key node in the battle against genotoxicity, carcinogenicity and apoptosis induced by alkylating agents. DNA Repair (Amst) 6(8):1079–1099. doi:10.1016/j.dnarep.2007.03.008
Tanaka S, Kobayashi I, Utsuki S, Oka H, Yasui Y, Fujii K (2005) Down-regulation of O6-methylguanine-DNA methyltransferase gene expression in gliomas by platinum compounds. Oncol Rep 14(5):1275–1280
D’Atri S, Graziani G, Lacal PM, Nisticò V, Gilberti S, Faraoni I, Watson AJ, Bonmassar E, Margison GP (2000) Attenuation of O(6)-methylguanine-DNA methyltransferase activity and mRNA levels by cisplatin and temozolomide in jurkat cells. J Pharmacol Exp Ther 294(2):664–671
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups; National Cancer Institute of Canada Clinical Trials Group (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996. doi:10.1056/NEJMoa043330
Walker MD, Alexander E Jr, Hunt WE et al (1978) Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial. J Neurosurg 49:333–343
Walker MD, Green SB, Byar DP et al (1980) Randomized comparisons of radiotherapy and nitrosoureas for the treatment of malignant glioma after surgery. N Engl J Med 303:1323–1329
Brandes AA, Tosoni A, Amista P et al (2004) How effective is BCNU in recurrent GBM in the modern era? A phase II trial. Neurology 63:1281–1284
Chang SM, Prados MD, Yung WK et al (2004) Phase II study of neoadjuvant 1,3-bis (2-chloroethyl)-1-nitrosourea and temozolomide for newly diagnosed anaplastic glioma: a North American Brain Tumor Consortium trial. Cancer 100:1712–1716. doi:10.1002/cncr.20157
Raizer JJ, Malkin MG, Kleber M et al (2004) Phase 1 study of 28-day, low-dose temozolomide and BCNU in the treatment of malignant gliomas after radiation therapy. Neuro-oncol 6:247–252. doi:10.1215/S1152851704000122
Fruehauf JP, Brem H, Brem S, Sloan A, Barger G, Huang W, Parker R (2006) In vitro drug response and molecular markers associated with drug resistance in malignant gliomas. Clin Cancer Res 12(15):4523–4532. doi:10.1158/1078-0432.CCR-05-1830
Boiardi A, Eoli M, Salmaggi A, Pollo B, Milanesi I, Broggi G, Silvani A (2000) Cisplatin and BCNU chemotherapy for anaplastic oligoastrocytomas. J Neurooncol 49(1):71–75. doi:10.1023/A:1006489919811
Silvani A, Eoli M, Salmaggi A, Lamperti E, Maccagnano E, Broggi G, Boiardi A (2004) Phase II trial of cisplatin plus temozolomide, in recurrent and progressive malignant glioma patients. J Neurooncol 66(1–2):203–208. doi:10.1023/B:NEON.0000013479.64348.69
Esteller M, Garcia-Foncillas J, Andion E, Goodman SN, Hidalgo OF, Vanaclocha V, Baylin SB, Herman JG (2000) Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med 343(19):1350–1354. doi:10.1056/NEJM200011093431901
Buckner JC, Ballman KV, Michalak JC, Burton GV, Cascino TL, Schomberg PJ, Hawkins RB, Scheithauer BW, Sandler HM, Marks RS, O’Fallon JR (2006) North Central Cancer Treatment Group 93-72-52; Southwest Oncology Group 9503 Trials. Phase III trial of carmustine and cisplatin compared with carmustine alone and standard radiation therapy or accelerated radiation therapy in patients with glioblastoma multiforme: North Central Cancer Treatment Group 93-72-52 and Southwest Oncology Group 9503 Trials. J Clin Oncol 24(24):3871–3879. doi:10.1200/JCO.2005.04.6979
Frenay M, Giroux B, Khoury S, Derlon JM, Namer M (1991) Phase II study of fotemustine in recurrent supratentorial malignant gliomas. Eur J Cancer 27(7):852–856
Fetell MR, Grossman SA, Fisher JD et al (1997) Preirradiation paclitaxel in GBM multiforme: efficacy, pharmacology, and drug interactions. New Approaches to Brain Tumor Therapy Central Nervous System Consortium. J Clin Oncol 15:3121–3128
Ciusani E, Balzarotti M, Calatozzolo C, de Grazia U, Boiardi A, Salmaggi A, Croci D (2007) Valproic acid increases the in vitro effects of nitrosureas on human glioma cell lines. Oncol Res 16(10):453–463. doi:10.3727/096504007783338340
Sher DJ, Henson JW, Avutu B, Hochberg FH, Batchelor TT, Martuza RL, Barker FG II, Loeffler JS, Chakravarti A (2008) The added value of concurrently administered temozolomide versus adjuvant temozolomide alone in newly diagnosed GBM. J Neurooncol 88(1):43–50
Osoba D, Brada M, Yung WK, Prados M (2000) Health-related quality of life in patients treated with temozolomide versus procarbazine for recurrent GBM multiforme. J Clin Oncol 18(7):1481–1491
Taphoorn MJ, Stupp R, Coens C, Osoba D, Kortmann R, van den Bent MJ, Mason W, Mirimanoff RO, Baumert BG, Eisenhauer E, Forsyth P, Bottomley A, EORTC Radiotherapy Group; National Cancer Institute of Canada Clinical Trials Group (2005) Health-related quality of life in patients with GBM: a randomised controlled trial. Lancet Oncol 6(12):937–944. doi:10.1016/S1470-2045(05)70432-0
Sghirlanzoni A, Silvani A, Scaioli V, Pareyson D, Marchesan R, Boiardi A (1992) Cisplatin neuropathy in brain tumor chemotherapy. Ital J Neurol Sci 13(4):311–315. doi:10.1007/BF02223095
Meyers CA, Brown PD (2006) Role and relevance of neurocognitive assessment in clinical trials of patients with CNS tumors. J Clin Oncol 24:1305–1309. doi:10.1200/JCO.2005.04.6086
Lamers LM, Stupp R, van den Bent MJ, Al MJ, Gorlia T, Wasserfallen JB, Mittmann N, Jin Seung S, Crott R, Uyl-de Groot CA (2008) Cost-effectiveness of temozolomide for the treatment of newly diagnosed GBM multiforme: a report from the EORTC 26981/22981 NCI-C CE3 Intergroup Study. Cancer 112(6):1337–1344. doi:10.1002/cncr.23297
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silvani, A., Gaviani, P., Lamperti, E.A. et al. Cisplatinum and BCNU chemotherapy in primary glioblastoma patients. J Neurooncol 94, 57–62 (2009). https://doi.org/10.1007/s11060-009-9800-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-009-9800-0