Abstract
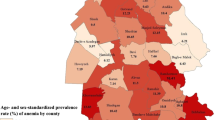
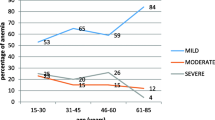
Currently, vast numbers of migrants with largely unknown health statuses have been entering Europe. To improve care taking strategies, prevalence, severity and types of anemia in a large refugee cohort were assessed. Blood counts were performed in n = 787 inhabitants from six German refugee centers. Most included migrants were young, male adults. Anemia was present in 22.5% of subjects with an age-dependent prevalence increase (7.9% > 18 years vs. 30.8% > 50 years). More females than males were anemic (27.1% vs. 20.4%). The majority of affected migrants had mild anemia (86.2%) of either normocytic/normochromic (55.9%) or microcytic/hypochromic (20.9%) type. Observed anemia frequencies are in accordance with global anemia prevalence recently estimated by the WHO. However, the observed high rates of anemia particularly in female and older refugees emphasize the need for adapted care taking strategies in refugee medicine. Further evaluation of causes of anemia in the migrating population is needed.



Similar content being viewed by others
References
McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B. Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutr. 2009;12(4):444–54.
Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243–60.
UNHCR. UNHCR strategic plan for anaemia prevention, control and reduction. reducing the global burden of anaemia in refugee populations. UNHCR; 2008–2010.
Sekhavat L, Davar R, Hosseinidezoki S. Relationship between maternal hemoglobin concentration and neonatal birth weight. Hematology 2011;16(6):373–6.
Rahman MM, Abe SK, Rahman MS, Kanda M, Narita S, Bilano V, et al. Maternal anemia and risk of adverse birth and health outcomes in low- and middle-income countries: systematic review and meta-analysis. Am J Clin Nutr. 2016;103(2):495–504.
Guilbert JJ. The world health report 2002 - reducing risks, promoting healthy life. Educ Health (Abingdon). 2003;16(2):230.
Intrauterine infections: problems and prevention. Lancet 1973;1(7808):868–9.
Killip S, Bennett JM, Chambers MD. Iron deficiency anemia. Am Fam Physician. 2007;75(5):671–8.
Akbari M, Moosazadeh M, Tabrizi R, Khatibi SR, Khodadost M, Heydari ST, et al. Estimation of iron deficiency anemia in Iranian children and adolescents: a systematic review and meta-analysis. Hematology 2017;22(4):231–9.
Parsons SK, Fleming MD, Nathan DG, Andrews NC. Iron deficiency anemia associated with an error of iron metabolism in two siblings: a thirty year follow up. Hematology 1996;1(1):65–73.
Ferrara M, Coppola L, Coppola A, Capozzi L. Iron deficiency in childhood and adolescence: retrospective review. Hematology 2006;11(3):183–6.
Mitchell Lewis S. Introduction–the global problem of nutritional anemias. Hematology 2005;10(Suppl 1):224–6.
Hossain MS, Raheem E, Sultana TA, Ferdous S, Nahar N, Islam S, et al. Thalassemias in South Asia: clinical lessons learnt from Bangladesh. Orphanet J Rare Dis. 2017;12(1):93.
Lam E, McCarthy A, Brennan M. Vaccine-preventable diseases in humanitarian emergencies among refugee and internally-displaced populations. Hum Vaccin Immunother. 2015;11(11):2627–36.
Castelli F, Tomasoni LR, El Hamad I. Migration and chronic noncommunicable diseases: is the paradigm shifting? J Cardiovasc Med (Hagerstown). 2014;15(9):693–5.
Castelli F, Sulis G. Migration and infectious diseases. Clin Microbiol Infect. 2017;23(5):283–9.
Henjum S, Barikmo I, Strand TA, Oshaug A, Torheim LE. Iodine-induced goitre and high prevalence of anaemia among Saharawi refugee women. Public Health Nutr. 2012;15(8):1512–8.
Blanck HM, Bowman BA, Serdula MK, Khan LK, Kohn W, Woodruff BA. Angular stomatitis and riboflavin status among adolescent Bhutanese refugees living in southeastern Nepal. Am J Clin Nutr. 2002;76(2):430–5.
Pavlopoulou ID, Tanaka M, Dikalioti S, Samoli E, Nisianakis P, Boleti OD, et al. Clinical and laboratory evaluation of new immigrant and refugee children arriving in Greece. BMC Pediatr. 2017;17(1):132.
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitam Miner Nutr Inf Syst 2011;WHO/NMH/NHD/MNM/11.1.
Matos JF, Dusse LM, Borges KB, de Castro RL, Coura-Vital W, Carvalho M. A new index to discriminate between iron deficiency anemia and thalassemia trait. Rev Bras Hematol Hemoter. 2016;38(3):214–9.
Mentzer WC Jr. Differentiation of iron deficiency from thalassaemia trait. Lancet 1973;1(7808):882.
Buber-Ennser I, Kohlenberger J, Rengs B, Al Zalak Z, Goujon A, Striessnig E, et al. Human capital, values, and attitudes of persons seeking refuge in Austria in 2015. PLoS ONE. 2016;11(9):e0163481.
Jablonka A, Happle C, Grote U, Schleenvoigt BT, Hampel A, Dopfer C, et al. Measles, mumps, rubella, and varicella seroprevalence in refugees in Germany in 2015. Infection 2016;44(6):781–7.
Jablonka A, Behrens GM, Stange M, Dopfer C, Grote U, Hansen G, et al. Tetanus and diphtheria immunity in refugees in Europe in 2015. Infection 2017;45(2):157–64.
Le CH. The prevalence of anemia and moderate-severe anemia in the US population (NHANES 2003–2012). PLoS ONE. 2016;11(11):e0166635.
J. Z. Population movement is a challenge for refugees and migrants as well as for the receiving population. http://www.eurowhoint/en/health-topics/health-determinants/migration-and-health/news/news/2015/09/population-movement-is-a-challenge-for-refugees-and-migrants-as-well-as-for-the-receiving-population. 2015.
Carrico RM, Goss L, Wiemken TL, Bosson RS, Peyrani P, Mattingly WA, et al. Infection prevention and control and the refugee population: experiences from the University of Louisville Global Health Center. Am J Infect Control. 2017;45(6):673–6.
Johnston V, Smith L, Roydhouse H. The health of newly arrived refugees to the Top End of Australia: results of a clinical audit at the Darwin Refugee Health Service. Aust J Prim Health. 2012;18(3):242–7.
UNHCR. http://www.unhcr.org/figures-at-a-glance.html. 2017.
WHO U, ONU. Iron deficiency anemia: assessment, prevention and control, a guide for programme managers. Geneva (CH) World Health Organization Report No: WHO/NHD/013. 2001.
Morrone A, Nosotti L, Piombo L, Scardella P, Spada R, Pitidis A. Iron deficiency anaemia prevalence in a population of immigrated women in Italy. Eur J Public Health. 2012;22(2):256–62.
Redditt VJ, Graziano D, Janakiram P, Rashid M. Health status of newly arrived refugees in Toronto, Ont: Part 2: chronic diseases. Can Fam Physician. 2015;61(7):e310–5.
Seal AJ, Creeke PI, Mirghani Z, Abdalla F, McBurney RP, Pratt LS, et al. Iron and vitamin A deficiency in long-term African refugees. J Nutr. 2005;135(4):808–13.
Tomashek KM, Woodruff BA, Gotway CA, Bloland P, Mbaruku G. Randomized intervention study comparing several regimens for the treatment of moderate anemia among refugee children in Kigoma Region, Tanzania. Am J Trop Med Hyg. 2001;64(3–4):164–71.
Shah AY, Suchdev PS, Mitchell T, Shetty S, Warner C, Oladele A, et al. Nutritional status of refugee children entering DeKalb County, Georgia. J Immigr Minor Health. 2014;16(5):959–67.
Hershko C, Nesher G, Yinnon AM, Zandman-Goddard G, Klutstein M, Abrahamov A, et al. Medical problems in Ethiopian refugees airlifted to Israel: experience in 131 patients admitted to a general hospital. J Trop Med Hyg. 1986;89(3):107–12.
Rondinelli AJ, Morris MD, Rodwell TC, Moser KS, Paida P, Popper ST, et al. Under- and over-nutrition among refugees in San Diego County, California. J Immigr Minor Health. 2011;13(1):161–8.
Acknowledgements
The authors would like to thank all doctors and medical personnel involved in medical care of the refugees for their exceptional work. We would furthermore like to thank Christian Berger, Don-Philipp Dratschke, Matthias Joachim, Jean-Luc Kruppa, Henrick Langner, Bianca Schnake, Arne Steinbrück and Kai Zaengel for the organization of medical care, Annika Hampel for data processing and Torsten Bergemann of Nexave for the extraction from the electronic database. We thank Timothy Price for proof reading of the manuscript.
Funding
This study was supported by Deutsches Zentrum für Infektionsforschung (Grant No. Structural Fond), Medizinischen Hochschule Hannover (Grant No. Junge Akademie). Alexandra Jablonka was funded by the Young Academy Clinician/Scientist program of Hannover Medical School, Germany. Christine Happle received funding from the Young Academy Clinician/Scientist foundation and HiLF funding of Hannover Medical School, Germany.
Author information
Authors and Affiliations
Contributions
Research design: Alexandra Jablonka, Georg MN Behrens, Reinhold RE Schmidt. Sample collection and analyses: Routine clinical care. Data analysis: Alexandra Jablonka, Martin Wetzke, Christian Dopfer, Georgios Sogkas, Christine Happle. Writing and contributing to writing of the manuscript: All authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interests to specify.
Rights and permissions
About this article
Cite this article
Jablonka, A., Wetzke, M., Sogkas, G. et al. Prevalence and Types of Anemia in a Large Refugee Cohort in Western Europe in 2015. J Immigrant Minority Health 20, 1332–1338 (2018). https://doi.org/10.1007/s10903-018-0725-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-018-0725-6