Abstract
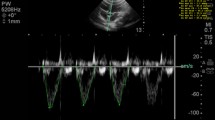
Aortic peak systolic velocity variation (ΔVpeakAo) is a reliable dynamic indicator of preload in mechanically ventilated children. However, easily measurable alternative parameters like carotid peak systolic velocity variation (ΔVpeakCa) and suprasternal peak systolic velocity variation (ΔVpeakSs) are not well evaluated in children. The aim of the study was to find correlation between ΔVpeakCa and ΔVpeakSs to ΔVpeakAo, as potential surrogate markers of fluid responsiveness. 52 children, 1–12 years old, undergoing major non-cardiac surgeries under general endotracheal anaesthesia were recruited for this single-centre prospective observational study. ΔVpeakAo, ΔVpeakCa and ΔVpeakSs were measured by pulsed wave Doppler in appropriate windows, measuring maximum and minimum peak flow velocity over a single respiratory cycle. Calculated parameters were compared by a repeated measures study design. Correlation coefficients were 0.82 between ΔVpeakAo and ΔVpeakSs and 0.73 between ΔVpeakAo and ΔVpeakCa. Bland–Altman analysis showed minimal bias of 1.86 percentage points with limits of agreement of 11.21 to − 7.49 (ΔVpeakAo and ΔVpeakSs) and 3.93 percentage points with limits of agreement of 14.04 to − 6.18 (ΔVpeakAo and ΔVpeakCa). ΔVpeakSs and ΔVpeakCa also showed good discrimination to predict ΔVpeakAo (lying in previously validated fluid responsive zones) with sensitivities and specificities of 82.25% and 85% with cut-off of 11% for ΔVpeakSs, and 88.52% and 70% with cut-off of 8.6% for ΔVpeakCa. Carotid peak systolic velocity variation (ΔVpeakCa) and suprasternal peak systolic velocity variation (ΔVpeakCa) can be potential surrogate markers for Aortic peak systolic velocity variation (ΔVpeakAo) in assessing fluid responsiveness in mechanically ventilated children.
Study registration: Clinicaltrials.gov ID NCT03155555.


Similar content being viewed by others
Data availability
The dataset used and analysed in the present study is available from the corresponding author on request.
References
Gan H, Cannesson M, Chandler JR, Ansermino JM. Predicting fluid responsiveness in children: a systematic review. Anesth Analg. 2013;117:1380–92.
Desgranges FP, Desebbe O, de Souza Neto PE, Raphael D, Chassard D. Respiratory variation in aortic blood flow peak velocity to predict fluid responsiveness in mechanically ventilated children: a systematic review and meta-analysis. Paediatr Anaesth. 2016;89:37–47.
Durand P, Chevret L, Essouri S, Haas V, Devictor D. Respiratory variations in aortic blood flow predict fluid responsiveness in ventilated children. Intensive Care Med. 2008;34:888–94.
Choi DY, Kwak HJ, Park HY, Kim YB, Choi CH, Lee JY. Respiratory variation in aortic blood flow velocity as a predictor of fluid responsiveness in children after repair of ventricular septal defect. Pediatr Cardiol. 2010;31:1166–70.
De Souza Neto EP, Grousson S, Duflo F, Ducreux C, Joly H, Convert J, et al. Predicting fluid responsiveness in mechanically ventilated children under general anaesthesia using dynamic parameters and transthoracic echocardiography. Br J Anaesth. 2011;106:856–64.
Renner J, Broch O, Duetschke P, Scheewe J, Höcker J, Moseby M, et al. Prediction of fluid responsiveness in infants and neonates undergoing congenital heart surgery. Br J Anaesth. 2012;108:108–15.
Byon HJ, Lim CW, Lee JH, Park YH, Kim HS, Kim CS, et al. Prediction of fluid responsiveness in mechanically ventilated children undergoing neurosurgery. Br J Anaesth. 2013;110:586–91.
Lee JY, Kim JY, Choi CH, Kim HS, Lee KC, Kwak HJ. The ability of stroke volume variation measured by a noninvasive cardiac output monitor to predict fluid responsiveness in mechanically ventilated children. Pediatr Cardiol. 2014;35:289–94.
Achar SK, Sagar MS, Shetty R, Kini G, Samanth J, Nayak C, et al. Respiratory variation in aortic flow peak velocity and inferior vena cava distensibility as indices of fluid responsiveness in anaesthetised and mechanically ventilated children. Indian J Anaesth. 2016;60:121–6.
Morparia KG, Reddy SK, Olivieri LJ, Spaeder MC, Schuette JJ. Respiratory variation in peak aortic velocity accurately predicts fluid responsiveness in children undergoing neurosurgery under general anesthesia. J Clin Monit Comput. 2018;32:221–6.
Xu T, Zhang J. Perioperative fluid administration in children: is there consensus? Pediatr Anesth. 2017;27:4–6.
Song Y, Kwak YL, Song JW, Kim YJ, Shim JK. Respirophasic carotid artery peak velocity variation as a predictor of fluid responsiveness in mechanically ventilated patients with coronary artery disease. Br J Anaesth. 2014;113:61–6.
Ibarra-Estrada M, López-Pulgarín JA, Mijangos-Méndez JC, Díaz-Gómez JL, Aguirre-Avalos G. Respiratory variation in carotid peak systolic velocity predicts volume responsiveness in mechanically ventilated patients with septic shock: a prospective cohort study. Crit Ultrasound J. 2015;7:1–9.
Devauchelle P, de Queiroz Siqueira M, Lilot M, Chassard D, Desgranges FP. Suprasternal notch echocardiography: a potential alternative for the measurement of respiratory variation in aortic blood flow peak velocity in mechanically ventilated children. J Clin Monit Comput. 2018;32:589–91.
Senzaki H, Akagi M, Hishi T, Ishizawa A, Yanagisawa M, Masutani S, et al. Age-associated changes in arterial elastic properties in children. Eur J Pediatr. 2002;161:547–51.
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent J-L. Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med. 2005;31:517–23.
Bakdash JZ, Marusich LR. Repeated measures correlation. Front Psychol. 2017;8:1–13.
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez J, et al. pROC: an open-source package for R and S + to analyze and compare ROC curves. BMC Bioinform. 2011;12:77.
Carstensen B. Comparing clinical measurement methods [Internet]. Chichester: Wiley; 2010. http://doi.wiley.com/10.1002/9780470683019.
Papastamelos C, Panitch HB, England SE, Allen JL. Developmental changes in chest wall compliance in infancy and early childhood. J Appl Physiol. 1995;78:179–84.
Trinkmann F, Doesch C, Papavassiliu T, Weissmann J, Haghi D, Gruettner J, et al. A novel noninvasive ultrasonic cardiac output monitor: comparison with cardiac magnetic resonance. Clin Cardiol. 2010;33:8–14.
Stolz L, Mosier J, Gross A, Douglas M, Blaivas M, Adhikari S. Can emergency physicians perform common carotid doppler flow measurements to assess volume responsiveness? West J Emerg Med. 2015;16:255–9.
Benes J, Giglio M, Brienza N, Michard F. The effects of goal-directed fluid therapy based on dynamic parameters on post-surgical outcome: a meta-analysis of randomized controlled trials. Crit Care. 2014;18:1–11.
Cannesson M, Gan TJ. PRO: perioperative goal-directed fluid therapy is an essential element of an enhanced recovery protocol. Anesth Analg. 2016;122:1258–60.
Sümpelmann R, Becke K, Brenner S, Breschan C, Eich C, Höhne C, et al. Perioperative intravenous fluid therapy in children: guidelines from the Association of the Scientific Medical Societies in Germany. Paediatr Anaesth. 2017;27:10–8.
Warnert EA, Hart EC, Hall JE, Murphy K, Wise RG. The major cerebral arteries proximal to the Circle of Willis contribute to cerebrovascular resistance in humans. J Cereb Blood Flow Metab. 2016;36:1384–95.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to report.
Ethical approval
All procedures performed in studies involving human participants were reviewed and approved by the Institutional Ethical Committee and were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Institutional Ethical Committee approval (INT/IEC/2016/2525) was obtained.
Informed consent
Informed consent was obtained from the legal guardians of all individual participants included in the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Niyogi, S.G., Sen, I.M., Jayant, A. et al. Surrogate indices of aortic peak systolic velocity variation to monitor fluid responsiveness in pediatric non-cardiac surgery: a prospective observational study. J Clin Monit Comput 34, 1159–1166 (2020). https://doi.org/10.1007/s10877-019-00431-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00431-8