Abstract
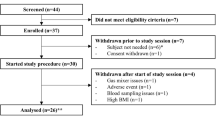
The ability of practitioners to assess the adequacy of global oxygen delivery is dependent on an accurate measurement of central venous saturation. Traditional techniques require the placement of invasive central venous access devices. This study aimed to compare two non-invasive technologies for the estimation of regional venous saturation (reflectance plethysmography and near infrared spectroscopy [NIRS]), using venous blood gas analysis as gold standard. Forty patients undergoing cardiac surgery were recruited in two groups. In the first group a reflectance pulse oximeter probe was placed on the skin overlying the internal jugular vein. In the second group, a Somanetics INVOS oximeter patch was placed on the skin overlying the internal jugular vein and overlying the ipsilateral cerebral hemisphere. Central venous catheters were placed in all patients. Oxygen saturation estimates from both groups were compared with measured saturation from venous blood. Twenty patients participated in each group. Data were analyzed by the limits of agreement technique suggested by Bland and Altman and by linear regression analysis. In the reflectance plethysmography group, the mean bias was 4.27% and the limits of agreement were 58.3 to −49.8% (r2 = 0.00, p = 0.98). In the NIRS group the mean biases were 10.8% and 2.0% for the sensors attached over the cerebral hemisphere and over the internal jugular vein, respectively, and the limits of agreement were 33.1 to −11.4 and 19.5 to −15.5% (r2 = 0.22, 0.28; p = 0.04, 0.03) for the cerebral hemisphere and internal jugular sites, respectively. While transcutaneous regional oximetry and NIRS have both been used to estimate venous and tissue oxygen saturation non-invasively, the correlation between estimates of ScvO2 and SxvO2 were statistically significant for near infrared spectroscopy, but not for transcutaneous regional oximetry. Placement of cerebral oximetry patches directly over the internal jugular vein (as opposed to on the forehead) appeared to approximate internal jugular venous saturation better (lower mean bias and tighter limits of agreement), which suggests this modality may with refinement offer the practitioner additional clinically useful information regarding global cerebral oxygen supply and demand matching.



Similar content being viewed by others
References
Mihm FG, Halperin BD. Noninvasive detection of profound arterial desaturations using a pulse oximetry device. Anesthesiology. 1985;62(1):85–7.
Committee ASOASAPP. Standards For Basic Anesthetic Monitoring. Am Soc Anesthesiol. 2011;2010:1–3.
Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77.
Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med. 2008;36:296–327.
Walton ZD, Kyriacou PA, Silverman DG, Shelley KH. Measuring venous oxygenation using the photoplethysmograph waveform. J Clin Monit Comput. 2010;24(4):295–303.
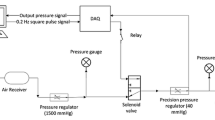
Thiele RH, Tucker-Schwartz JM, Lu Y, Gillies GT, Durieux ME. Transcutaneous regional venous oximetry. Anesth Analg. 2011;112(6):1353–7.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995;346(8982):1085–7.
Pearse R, Dawson D, Fawcett J, et al. Changes in central venous saturation after major surgery, and association with outcome. Crit Care. 2005;9(6):R694–9.
Collaborative Study Group on Perioperative ScvO2 Monitoring. Multicentre study on peri- and postoperative central venous oxygen saturation in high-risk surgical patients. Crit Care 2006;10(6):R158.
Pölönen P, Hippeläinen M, Takala R, Ruokonen E, Takala J. Relationship between intra- and postoperative oxygen transport and prolonged intensive care after cardiac surgery: a prospective study. Acta Anaesthesiol Scand. 1997;41(7):810–7.
Routsi C, Vincent JL, Bakker J, et al. Relation between oxygen consumption and oxygen delivery in patients after cardiac surgery. Anesth Analg. 1993;77(6):1104–10.
Schmidt CR, Frank LP, Forsythe SB, Estafanous FG. Continuous S-vO2 measurement and oxygen transport patterns in cardiac surgery patients. Crit Care Med. 1984;12(6):523–7.
Donati A, Loggi S, Preiser J-C, et al. Goal-directed intraoperative therapy reduces morbidity and length of hospital stay in high-risk surgical patients. Chest. 2007;132(6):1817–24.
Pölönen P, Ruokonen E, Hippeläinen M, Pöyhönen M, Takala J. A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg. 2000;90(5):1052–9.
Gehring H, Duembgen L, Peterlein M, Hagelberg S, Dibbelt L. Hemoximetry as the “Gold Standard?” Error Assessment Based on Differences Among Identical Blood Gas Analyzer Devices of Five Manufacturers. Anesth Analg. 2007;105(On Line Suppl.):S24–30.
Sarrazin F, Tessler MJ, Kardash K, McNamara E, Holcroft C. Blood gas measurements using the Bayer Rapid Point 405: are we basing our decisions on accurate data? J Clin Monit Comput. 2007;21(4):253–6.
Tortoriello TA, Stayer SA, Mott AR, et al. A noninvasive estimation of mixed venous oxygen saturation using near-infrared spectroscopy by cerebral oximetry in pediatric cardiac surgery patients. Pediatric Anesth. 2005;15(6):495–503.
Knirsch W, Stutz K, Kretschmar O, et al. Regional cerebral oxygenation by NIRS does not correlate with central or jugular venous oxygen saturation during interventional catheterisation in children. Acta Anaesthesiol Scand. 2008;52(10):1370–4.
McQuillen PS, Nishimoto MS, Bottrell CL, et al. Regional and central venous oxygen saturation monitoring following pediatric cardiac surgery: concordance and association with clinical variables*. Pediatric Crit Care Med. 2007;8(2):154–60.
Ranucci M, Isgro G, La Torre DeT, et al. Near-infrared spectroscopy correlates with continuous superior vena cava oxygen saturation in pediatric cardiac surgery patients. Pediatric Anesth. 2008;18(12):1163–9.
Bhutta AT, Ford JW, Parker JG, et al. Noninvasive cerebral oximeter as a surrogate for mixed venous saturation in children. Pediatr Cardiol. 2007;28(1):34–41.
Weiss M, Dullenkopf A, Kolarova A, et al. Near-infrared spectroscopic cerebral oxygenation reading in neonates and infants is associated with central venous oxygen saturation. Pediatric Anesth. 2005;15(2):102–9.
Abdul-Khaliq H, Troitzsch D, Berger F, Lange PE. Regional transcranial oximetry with near infrared spectroscopy (NIRS) in comparison with measuring oxygen saturation in the jugular bulb in infants and children for monitoring cerebral oxygenation. Biomed Tech (Berl). 2000;45(11):328–32.
Dullenkopf A, Baulig W, Weiss M, Schmid ER. Cerebral near-infrared spectroscopy in adult patients after cardiac surgery is not useful for monitoring absolute values but may reflect trends in venous oxygenation under clinical conditions. J Cardiothorac Vasc Anesth. 2007;21(4):535–9.
Schön J, Heringlake M, Berger K, et al. Relationship between mixed venous oxygen saturation and regional cerebral oxygenation in awake, spontaneously breathing cardiac surgery patients. Minerva Anestesiol. 2011;77(10):952–8.
Paarmann H, Heringlake M, Heinze H, et al. Non-invasive cerebral oxygenation reflects mixed venous oxygen saturation during the varying haemodynamic conditions in patients undergoing transapical transcatheter aortic valve implantation. Interact Cardiovasc Thorac Surg; 2011.
Somanetics Corporation. Promotional Materials; 2011.
Menssen J, Colier W, Hopman J, Liem D, de Korte C. A method to calculate arterial and venous saturation from near infrared spectroscopy (NIRS). Adv Exp Med Biol. 2009;645:135–40.
Critchley LA, Lee A, Ho AM-H. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111(5):1180–92.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Colquhoun, D.A., Tucker-Schwartz, J.M., Durieux, M.E. et al. Non-invasive estimation of jugular venous oxygen saturation: a comparison between near infrared spectroscopy and transcutaneous venous oximetry. J Clin Monit Comput 26, 91–98 (2012). https://doi.org/10.1007/s10877-012-9338-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-012-9338-0