Abstract
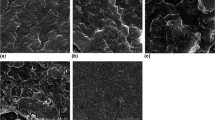
Polycaprolactone (PCL) is a biocompatible, biodegradable synthetic polymer which in combination with nanohydroxyapatite (nHAp) can give rise to a low cost, nontoxic bioactive product with excellent mechanical properties and slow degradation. Here we produced, characterized and evaluated in vivo the bone formation of PCL/nHAp scaffolds produced by the rotary jet spinning technique. The scaffolds produced were firstly soaked into simulated body fluid for 21 days to also obtain nHAp onto PCL/nHAp scaffolds. Afterwards, the scaffolds were characterized by scanning electron microscopy (SEM), energy dispersive spectroscopy and Raman spectroscopy. For in vivo experiments, 20 male Wistar rats were used and randomly divided in 4 experimental groups (n = 5). A critical defect of 3 mm in diameter was made in the tibia of the animals, which were filled with G1 control (clot); G2—PCL scaffold; G3—PCL/nHAp (5%) scaffold; G4—PCL/nHAp (20%) scaffold. All animals were euthanized 60 days after surgery, and the bone repair in the right tibiae were evaluated by radiographic analysis, histological analysis and histomorphometric analysis. While in the left tibias, the areas of bone repair were submitted to the flexural strength test. Radiographic and histomorphometric analyses no showed statistical difference in new bone formation between the groups, but in the three-point flexural tests, the PCL/nHAp (20%) scaffold positively influenced the flexural mode of the neoformed bone. These findings indicate that PCL/nHAp (20%) scaffold improve biomechanical properties of neoformed bone and could be used for bone medicine regenerative.






Similar content being viewed by others
References
Grabowski G, Cornett CA. Bone graft and bone graft substitutes in spine surgery: current concepts and controversies. JAAOS-J Am Acad Orthop Surg. 2013;21:51.
Amini AR, Laurencin CT, Nukavarapu SP. Bone tissue engineering: recent advances and challenges. Crit Rev Biomed Eng. 2012;40:363.
Chaudhury K, Kumar V, Kandasamy J, RoyChoudhury S. Regenerative nanomedicine: current perspectives and future directions. Int J Nanomed. 2014;9:4153. https://doi.org/10.2147/IJN.S45332.
Mohammadi M, Mousavi Shaegh SA, Alibolandi M, Ebrahimzadeh MH, Tamayol A, Jaafari MR, et al. Micro and nanotechnologies for bone regeneration: Recent advances and emerging designs. J Controlled Release. 2018;274:35. https://doi.org/10.1016/j.jconrel.2018.01.032.
Rezvani Z, Venugopal JR, Urbanska AM, Mills DK, Ramakrishna S, Mozafari M. A bird’s eye view on the use of electrospun nanofibrous scaffolds for bone tissue engineering: Current state‐of‐the‐art, emerging directions and future trends. Nanomed: Nanotechnol Biol Med. 2016;12:2181. https://doi.org/10.1016/j.nano.2016.05.014.
O’brien FJ. Biomaterials & scaffolds for tissue engineering. Mater Today. 2011;14:88.
Giannona S, Firkowska I, Rojas-Chapana J, Giersig M. Vertically aligned carbon nanotubes as cytocompatible material for enhanced adhesion and proliferation of osteoblast-like cells. J Nanosci Nanotechnol. 2007;7:1679.
Tabata Y. Biomaterial technology for tissue engineering applications. J R Soc interface. 2009;6:S311.
Kim S-S, Park MS, Jeon O, Choi CY, Kim B-S. Poly (lactide-co-glycolide)/hydroxyapatite composite scaffolds for bone tissue engineering. Biomaterials. 2006;27:1399.
Cristofaro F, Gigli M, Bloise N, Chen H, Bruni G, Munari A, et al. Influence of the nanofiber chemistry and orientation of biodegradable poly (butylene succinate)-based scaffolds on osteoblast differentiation for bone tissue regeneration. Nanoscale. 2018;10:8689
Dayer R, Badoud I, Rizzoli R, Ammann P. Defective Implant Osseointegration Under Protein Undernutrition: Prevention by PTH or Pamidronate. J Bone Miner Res. 2007;22:1526. https://doi.org/10.1359/jbmr.070610.
Aspenberg P, Genant HK, Johansson T, Nino AJ, See K, Krohn K, et al. Teriparatide for acceleration of fracture repair in humans: A prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J Bone Miner Res. 2010;25:404. https://doi.org/10.1359/jbmr.090731.
Sansone RA, Sansone LA. SSRIs: bad to the bone? Innov Clin Neurosci. 2012;9:42.
Mountziaris PM, Mikos AG. Modulation of the inflammatory response for enhanced bone tissue regeneration. Tissue Eng Part B: Rev. 2008;14:179.
Kim H-W, Knowles JC, Kim H-E. Hydroxyapatite/poly(ε-caprolactone) composite coatings on hydroxyapatite porous bone scaffold for drug delivery. Biomaterials. 2004;25:1279. https://doi.org/10.1016/j.biomaterials.2003.07.003.
Dwivedi R, Kumar S, Pandey R, Mahajan A, Nandana D, Katti DS, et al. Polycaprolactone as biomaterial for bone scaffolds: review of literature. J Oral Biol Craniofacial Res. 2020;10:381
Ganesh N, Ashokan A, Rajeshkannan R, Chennazhi K, Koyakutty M, Nair SV. Magnetic resonance functional nano-hydroxyapatite incorporated poly (caprolactone) composite scaffolds for in situ monitoring of bone tissue regeneration by MRI. Tissue Eng Part A. 2014;20:2783.
Koutsopoulos S. Synthesis and characterization of hydroxyapatite crystals: a review study on the analytical methods. J Biomed Mater Res. 2002;62:600. https://doi.org/10.1002/jbm.10280.
de Castro JG, Rodrigues BVM, Ricci R, Costa MM, Ribeiro AFC, Marciano FR, et al. Designing a novel nanocomposite for bone tissue engineering using electrospun conductive PBAT/polypyrrole as a scaffold to direct nanohydroxyapatite electrodeposition. RSC Adv. 2016;6:32615. https://doi.org/10.1039/C6RA00889E.
Siqueira IAWB, Corat MAF, Cavalcanti BdN, et al. In vitro and in vivo studies of novel poly(d,l-lactic acid), superhydrophilic carbon nanotubes, and nanohydroxyapatite scaffolds for bone regeneration. ACS Appl Mater Interfaces. 2015;7:9385. https://doi.org/10.1021/acsami.5b01066.
Rogalski JJ, Bastiaansen CW, Peijs T. Rotary jet spinning review–a potential high yield future for polymer nanofibers. Nanocomposites. 2017;3:97.
Rogalski J, Bastiaansen C, Peijs T. PA6 nanofibre production: a comparison between rotary jet spinning and electrospinning. Fibers. 2018;6:37.
Badrossamay MR, McIlwee HA, Goss JA, Parker KK. Nanofiber assembly by rotary jet-spinning. Nano Lett. 2010;10:2257.
Baji A, Mai Y-W, Wong S-C, Abtahi M, Chen P. Electrospinning of polymer nanofibers: effects on oriented morphology, structures and tensile properties. Compos Sci Technol. 2010;70:703.
Ramakrishna S. An introduction to electrospinning and nanofibers. Singapore: World Scientific; 2005.
Badrossamay MR, Balachandran K, Capulli AK, Golecki HM, Agarwal A, Goss JA, et al. Engineering hybrid polymer-protein super-aligned nanofibers via rotary jet spinning. Biomaterials. 2014;35:3188. https://doi.org/10.1016/j.biomaterials.2013.12.072.
Golecki HM, Yuan H, Glavin C, Potter B, Badrossamay MR, Goss JA, et al. Effect of solvent evaporation on fiber morphology in rotary jet spinning. Langmuir. 2014;30:13369. https://doi.org/10.1021/la5023104.
Basile MA, d’Ayala GG, Malinconico M, Laurienzo P, Coudane J, Nottelet B, et al. Functionalized PCL/HA nanocomposites as microporous membranes for bone regeneration. Mater Sci Eng C-Mater Biol Appl. 2015;48:457. https://doi.org/10.1016/j.msec.2014.12.019.
Son S-R, Linh N-TB, Yang H-M, Lee B-T. In vitro and in vivo evaluation of electrospun PCL/PMMA fibrous scaffolds for bone regeneration. Sci Technol Adv Mater. 2013;14:015009.
Andrade TM, Mello DCR, Elias CMV, Abdala JMA, Silva E, Vasconcellos LMR, et al. In vitro and in vivo evaluation of rotary-jet-spun poly(ɛ-caprolactone) with high loading of nano-hydroxyapatite. J Mater Sci: Mater Med. 2019;30:19. https://doi.org/10.1007/s10856-019-6222-1.
Barrere F, van Blitterswijk CA, de Groot K, Layrolle P. Influence of ionic strength and carbonate on the Ca-P coating formation from SBF×5 solution. Biomaterials. 2002;23:1921. https://doi.org/10.1016/S0142-9612(01)00318-0.
Silva E, Pereira VF, Vasconcellos LMR, Oliveira FE, Brandão AAH. Quality of bone repair in ovariectomized rats with bone lesions treated with phytotherapic and homeopathic Arnica montana. Braz Dent Sci. 2017;20:25.
Vida TA, Motta AC, Santos AR Jr, Cardoso GBC, Brito CCD, Zavaglia CADC. Fibrous PCL/PLLA scaffolds obtained by rotary jet spinning and electrospinning. Mater Res. 2017;20:910.
Meyer RA Jr, Tsahakis PJ, Martin DF, Banks DM, Harrow ME, Kiebzak GM. Age and ovariectomy impair both the normalization of mechanical properties and the accretion of mineral by the fracture callus in rats. J Orthop Res. 2001;19:428.
Oliveira FC, Carvalho JO, Gusmão SBS, Gonçalves LS, Soares Mendes LM, Freitas SAP, et al. High loads of nano-hydroxyapatite/graphene nanoribbon composites guided bone regeneration using an osteoporotic animal model. Int J Nanomed. 2019;14:865.
Polo-Corrales L, Latorre-Esteves M, Ramirez-Vick JE. Scaffold design for bone regeneration. J Nanosci Nanotechnol. 2014;14:15.
Fan X, Ren H, Luo X, Wang P, Lv G, Yuan H, et al. Mechanics, degradability, bioactivity, in vitro, and in vivo biocompatibility evaluation of poly (amino acid)/hydroxyapatite/calcium sulfate composite for potential load-bearing bone repair. J Biomater Appl. 2016;30:1261.
Brown EC, Perrien DS, Fletcher TW, Irby DJ, Aronson J, Gao GG, et al. Skeletal toxicity associated with chronic ethanol exposure in a rat model using total enteral nutrition. J Pharmacol Exp Ther. 2002;301:1132.
Gürdal P, Akdeniz B. Comparison of two methods for radiometric evaluation of resin-based restorative materials. Dentomaxillofacial Radiol. 1998;27:236.
Harikrishnan P, Islam H, Sivasamy A. Biocompatibility studies of nanoengineered polycaprolactone and nanohydroxyapatite scaffold for craniomaxillofacial bone regeneration. J Craniofacial Surg. 2019;30:265.
Gao X, Song J, Ji P, Zhang X, Li X, Xu X, et al. Polydopamine-templated hydroxyapatite reinforced polycaprolactone composite nanofibers with enhanced cytocompatibility and osteogenesis for bone tissue engineering. ACS Appl Mater interfaces. 2016;8:3499.
Buyuksungur S, Tanir TE, Buyuksungur A, Bektas EI, Kose GT, Yucel D, et al. 3D printed poly (ε-caprolactone) scaffolds modified with hydroxyapatite and poly (propylene fumarate) and their effects on the healing of rabbit femur defects. Biomater Sci. 2017;5:2144.
Pramanik S, Ataollahi F, Pingguan-Murphy B, Oshkour AA, Osman NAA. In vitro study of surface modified poly (ethylene glycol)-impregnated sintered bovine bone scaffolds on human fibroblast cells. Sci Rep. 2015;5:9806.
Chon C-S, Yun H-S, Kim HS, Ko C. Elastic modulus of osteoporotic mouse femur based on femoral head compression test. Appl Bionics Biomech. 2017;2017:7201769. https://doi.org/10.1155/2017/7201769.
Vicente-Rodríguez G, Urzanqui A, Mesana MI, Ortega FB, Ruiz JR, Ezquerra J, et al. Physical fitness effect on bone mass is mediated by the independent association between lean mass and bone mass through adolescence: a cross-sectional study. J Bone Miner Metab. 2008;26:288. https://doi.org/10.1007/s00774-007-0818-0.
Author contributions
All authors contributed to the design of the study, write and discussion of the manuscript. JMAA and TMA produced the scaffolds. LMRV, GBM and JCR conducted the in vivo experiments and radiographic, histologic, histomorphometric and biomechanical analyzes. CMEV, SBSG and BCV characterized all produced scaffolds. LMRV, FRM, and AOL supervised all students. All authors read and approved the final manuscript.
Funding
This work was supported by the National Council for Scientific and Technological Development (CNPq, #303752/2017-3 and #404683/2018-5 to AOL and #304133/2017-5 and #424163/2016-0 to FRM) and FAPESP (2016/20820-0 to GBM).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Vasconcellos, L.M.R., Elias, C.d.M.V., Minhoto, G.B. et al. Rotary-jet spun polycaprolactone/nano-hydroxyapatite scaffolds modified by simulated body fluid influenced the flexural mode of the neoformed bone. J Mater Sci: Mater Med 31, 72 (2020). https://doi.org/10.1007/s10856-020-06403-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-020-06403-8