Abstract
Background
Circulating primary bile acid was involved in the regulation of cardiac ionic channel currents and ventricular myocyte apoptosis, but it was unknown whether or not it played a role in structural remodeling of AF. This study was aimed to testify the hypothesis that elevated chenodeoxycholic acid (CDCA) concentration correlated with left atrial low voltage area (LVA) and could induce apoptosis of atrial myocytes in AF.
Methods and results
Serum concentrations of 12 types of bile acids were determined in patients with paroxysmal (n = 21), persistent AF (n = 20), and type A pre-excitation and paroxysmal supraventricular tachycardia (PSVT) (n = 19) and were correlated with LVA in AF, which was obtained by electroanatomical mapping during ablation. Additionally, the impact of CDCA incubation on apoptosis of mouse atrial myocytes was evaluated. Serum levels of CDCA and cholic acid were significantly higher in AF than in PSVT. CDCA serum concentration was significantly higher in persistent AF than in paroxysmal AF. CDCA serum level was positively correlated with the size (r = 0.78, P < 0.05) and proportion of LVA (r = 0.89, P < 0.05) in AF patients. CDCA (75 μM, 100 μM) promoted atrial myocyte apoptosis in a concentration-dependent manner.
Conclusions
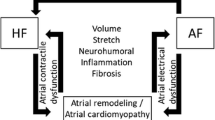
The higher circulating level of CDCA in AF than in PSVT, positive correlation of CDCA with LVA in AF, and incubation dose-dependent increase of mouse atrial myocyte apoptosis indicated that CDCA might play a significant role in the progress of structural remodeling of AF.

Similar content being viewed by others
References
Dzeshka MS, Lip GY, Snezhitskiy V, Shantsila E. Cardiac fibrosis in patients with atrial fibrillation: mechanisms and clinical implications. J Am Coll Cardiol. 2015;66:943–59.
Mahnkopf C, Badger TJ, Burgon NS, Daccarett M, Haslam TS, Badger CT, et al. Evaluation of the left atrial substrate in patients with lone atrial fibrillation using delayed-enhanced MRI: implications for disease progression and response to catheter ablation. Heart Rhythm. 2010;7:1475–81.
Wang XH, Li Z, Mao JL, He B. A novel individualized substrate modification approach for the treatment of long-standing persistent atrial fibrillation: preliminary results. Int J Cardiol. 2014;175:162–8.
Wang XH, Li Z, Mao JL, Zang MH, Pu J. Low voltage areas in paroxysmal atrial fibrillation: the prevalence, risk factors and impact on the effectiveness of catheter ablation. Int J Cardiol. 2018;269:139–44.
Vlachos K, Efremidis M, Letsas KP, Bazoukis G, Martin R, Kalafateli M, et al. Low-voltage areas detected by high-density electroanatomical mapping predict recurrence after ablation for paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol. 2017;28:1393–402.
Rainer PP, Primessnig U, Harenkamp S, Doleschal B, Wallner M, Fauler G, et al. Bile acids induce arrhythmias in human atrial myocardium—implications for altered serum bile acid composition in patients with atrial fibrillation. Heart. 2013;99:1685–92.
Desai MS, Penny DJ. Bile acids induce arrhythmias: old metabolite, new tricks. Heart. 2013;99:1629–30.
Pu J, Yuan A, Shan P, Gao E, Wang X, Wang Y, et al. Cardiomyocyte-expressed farnesoid-X-receptor is a novel apoptosis mediator and contributes to myocardial ischaemia/reperfusion injury. Eur Heart J. 2013;34:1834–45.
Zhao W, Zhao T, Chen Y, Ahokas RA, Sun Y. Oxidative stress mediates cardiac fibrosis by enhancing transforming growth factor-beta 1 in hypertensive rats. Mol Cell Biochem. 2008;317:43–50.
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. 2018;20:e1–e160.
Hofmann AF. The continuing importance of bile acids in liver and intestinal disease. Arch Intern Med. 1999;159:2647–58.
Rolf S, Kircher S, Arya A, Eitel C, Sommer P, Richter S, et al. Tailored atrial substrate modification based on low-voltage areas in catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol. 2014;7:825–33.
Wong KC, Sadarmin PP, De Bono J, Qureshi N, Jones M, Rajappan K, et al. Local activation times at the high posterior wall of the left atrium during left atrial appendage pacing predict roof line block with high specificity and sensitivity. Europace. 2011;13:1243–9.
Gorelik J, Harding SE, Shevchuk AI, Koralage D, Lab M, de Swiet M, et al. Taurocholate induces changes in rat cardiomyocyte contraction and calcium dynamics. Clin Sci (Lond). 2002;103:191–200.
Gorelik J, Shevchuk A, de Swiet M, Lab M, Korchev Y, Williamson C. Comparison of the arrhythmogenic effects of tauro- and glycoconjugates of cholic acid in an in vitro study of rat cardiomyocytes. BJOG. 2004;111:867–70.
Williamson C, Gorelik J, Eaton BM, Lab M, de Swiet M, Korchev Y. The bile acid taurocholate impairs rat cardiomyocyte function: a proposed mechanism for intra-uterine fetal death in obstetric cholestasis. Clin Sci (Lond). 2001;100:363–9.
Makishima M, Okamoto AY, Repa JJ, Tu H, Learned RM, Luk A, et al. Identification of a nuclear receptor for bile acids. Science. 1999;284:1362–5.
Bishop-Bailey D, Walsh DT, Warner TD. Expression and activation of the farnesoid X receptor in the vasculature. Proc Natl Acad Sci U S A. 2004;101:3668–73.
Hageman J, Herrema H, Groen AK, Kuipers F. A role of the bile salt receptor FXR in atherosclerosis. Arterioscler Thromb Vasc Biol. 2010;30:1519–28.
Swales KE, Korbonits M, Carpenter R, Walsh DT, Warner TD, Bishop-Bailey D. The farnesoid X receptor is expressed in breast cancer and regulates apoptosis and aromatase expression. Cancer Res. 2006;66:10120–1012.
Funding
This work was sponsored by Shanghai Natural Science Foundation Project (Grant No. 18ZR1423400), National Science Fund for Distinguished Young Scholars (81625002) and Shanghai Outstanding Academic Leaders Program (18XD1402400).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Rights and permissions
About this article
Cite this article
Wang, Xh., Li, Z., Zang, Mh. et al. Circulating primary bile acid is correlated with structural remodeling in atrial fibrillation. J Interv Card Electrophysiol 57, 371–377 (2020). https://doi.org/10.1007/s10840-019-00540-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00540-z