Abstract
A prospective disease group-based payment is a reimbursement rule used in a wide array of countries. It turns to be the hospital’s payment rule to imply. The secret of this payment is a fee payment as well as a hospital’s activity based payment. There is a consensus to consider this rule of payment as the least likely to be manipulated by the actors. However, the defined fee per group depends on recorded information that is then processed using complex algorithms. What if the data itself can be manipulated? The result would be a fee per group based on manipulated factors that would lead to an inefficient budget allocation between hospitals. Using a unique French longitudinal database with 145 million stays, I unambiguously demonstrate that the implementation of a finer classification led to an upcoding-learning effect. The end result has been a budget transfer from public non-research hospitals to for-profit hospitals. The 2009 policy lead to upcoding disconnected from any changes in the trend of production of care.

Similar content being viewed by others
Notes
In Health Economic literature, this shift is named upcoding.
Calculations based on the data used here yield the same results.
A transformation of the mean cost is actually used.
The French reimbursement system is discussed in Sect. 5.
Agence Technique de l’Information sur l’Hospitalisation (ATIH).
Details on the French DRG classification are given in “Appendix 2”.
In the robustness checks (Sect. 5), the model was run using a more restricted sample from the 2008–2010 period.
The only potential impact of the 2009 DRG change in coding on the actual production of care could have been through an increase in the length of stay (see “Appendix 2”). The empirical literature does not find support this assumption. A variety of papers have found a decrease of the length of stay over the observed period (DREES 2012a, b; Or et al. 2013; Gobillon and Milcent 2015).
Table 4 for coefficients and Table 5 for the marginal effects. Here, the marginal effect is an estimate of a population-averaged marginal effect. The reference is severity level 1, the lowest level. Note that a positive sign of any coefficients implies a higher probability of belonging to the higher category, corresponding in principle to greater severity.
Here, the marginal effect is an estimate of a population-averaged marginal effect.
For an overview of the methods used, see the IGF report, French Finance Ministry (2011), http://www.igf.finances.gouv.fr/webdav/site/igf/shared/NosRapports/documents/2012/2011-M-056-01.pdf.
The effect of “upcoding” behavior is standardised on the basis on the non-teaching public hospital “upcoding” behavior. Then, I compute the average “upcoding” behavior of the other hospital’s ownership compared with the nonteaching public hospital one. I multiplied this effect by average fee for patient coded as DRG level 2. I then got the average effect of the“upcoding” behavior for one patient coded as DRG level 1. To get the global effect, I multiplied this number by the number of patient coded as DRG level 1 admitted in hospitals except those admitted in the non-teaching public hospital.
This is known as the “tarif opposable de l’assurance maladie” [enforceable price to the national health insurance system], and is set for a given diagnosis-related group (DRG).
The base for calculating the costs of DRGs differs between the two groups. Doctors’ fees, as well as laboratory services, imaging, and function tests are included in the calculation of cost per DRG in the public sector, whereas they are not for the private sector. These prices are national and are published annually by the Ministry of Health.
As a robustness check, I also ran a least squares model including all admissions to acute care units. The results were unchanged (Table 9).
References
Barros, P., & Braun, G. (2017). Upcoding in a National Health Service: the evidence from Portugal. Health Economics, 26(5), 600–618.
Brekke, K. R., Siciliani, L., & Straume, O. R. (2011). Hospital competition and quality with regulated prices. Scandinavian Journal of Economics, 113(2), 444–469.
Brekke, K. R., Siciliani, L., & Straume, O. R. (2012). Quality competition with profit constraints. Journal of Economic Behavior & Organization, 84(2), 642–659.
Carter, G., & Ginsburg, P. (1985). The medicare case mix index increase: Medical practice changes, aging and DRG creep. The RAND Corporation. R-3292-HCFA.
Carter, G., Newhouse, J., & Relles, D. (1990). A. How much change in the case mix index is DRG creep? The RAND Corporation. R-3826-HCFA.
Chalkley, M., & Malcomson, J. M. (1998). Contracting for health services when patient demand does not reflect quality. Journal of Health Economics, 17, 1–19.
Dafny, L. S. (2005). How do hospitals respond to price changes? The American Economic Review, 95(5), 1525–1547.
DREES (Direction de la Recherche, Etudes, Evaluation et Statistiques). (2012a). Le panorama des établissements de santé, Editions 2012.
DREES (Direction de la Recherche, Etudes, Evaluation et Statistiques). (2012b). Evolution de l’offre et des prises en charge hospitalières entre 2001 et 2009: technicité croissante pour des séjours plus courts, Dossier Solidarité et Santé, 25.
Duggan, M. (2002). Hospital market structure and the behavior of not- for-profit hospitals. Rand Journal of Economics, 33(3), 433–446.
Ellis, R. P., & McGuire, T. (1986). Provider behavior under prospective reimbursement: Cost sharing and supply. Journal of Health Economics, 5, 129–151.
Georgescu, I., & Hartmann, F. G. H. (2013). Sources of financial pressure and up coding behavior in French public hospitals. Health Policy, 110(2–3), 156–163.
Gilman, B. H. (2000). Hospital response to DRG refinements: The impact of multiple Reim- bursement incentives on inpatient length of stay? Health Economics, 9(4), 277–294.
Gobillon, L.,& Milcent, C. (2015). The competition effect of a French reform on hospital quality. Working Paper PSE.
Hafsteinsdottir, E. J. G., & Siciliani, L. (2009). DRG prospective payment systems: refine or not refine? Health Economics, 19(10), 1226–1239.
Häkkinen, U., Chiarello, P., Cots, F., Peltola, M., Rättö, H., & EuroDRG group. (2012). Patient classification and hospital costs of care for acute myocardial infarction in nine European countries. Health Economics, 21(Suppl 2), 19–29.
Hsia, D. C., Krushat, W., Fagan, A., Tebbutt, J., & Kusserow, R. (1988). Accuracy of diagnostic coding for medicare patients under the prospective payment system. The New England Journal of Medicine, 318(6), 352–355.
Kimberly, J.R., de Pouvourville, G., & D’Aunno, T. (Eds.). (2008). The Globalization of Managerial Innovation in Health Care. Cambridge: Cambridge University Press.
Kuhn, M., & Siciliani L. (2008). Upcoding and optimal auditing in health care (or the economics of DRG creep). CEPR Discussion Paper, N°.6689.
Ma, C. (1994). Health care payment systems: Cost and quality incentives? Journal of Economics and Management Strategy, 3, 93–112.
Ma, C. (1998). Cost and quality incentive in health care: A reply. Journal of Economics and Management Strategy, 7, 139–142.
Manuel des GHM —groupes Homogenes de Malades (2012). 11eme version de la classification, 3eme revision (11d) Version 13.11d de la fonction groupage, Bulletin Officiel, Fascicule special, n2012/5bis
Mason, A., Zeynep, O., Renaud, Th, Street, A., Thuilliez, J., & Ward, P. (2012). How Well do diagnosis- related groups for appendectomy explain variations in resource use? An analysis of patient-level data from 10 European countries. Health Economics, 21(Suppl. 2), 30–40.
MedPAC. (2005). A DataBook: Healthcare spending and the medicare program (Washington: Med- PAC, June 2005), 102.
Milcent, C. (2017). Premier bilan de la T2A sur la variabilité des coûts hospitaliers. Economie et Prévision. 210.
Mougeot, M., & Naegelen, F. (2008). Supply-side risk adjustment and outlier payment policy. Journal of Health Economics, 27(5), 1196–1200.
Newhouse, J. P. (2002). Pricing the priceless: A health care conundrum. Cambridge: MIT Press.
Newhouse, J. P. (2003). Reimbursing for health care services? Economie Publique, 13, 3–31.
Or, Z., Bonastre, J., Journeau, F., & Nestrigue C. (2013). Production, Productivity and Care Quality in French Hospitals Before and After the Introduction of Activity Based Payment, Document de travail n? 56 - Irdes - Avril.
Pohlman, J. T., & Leitner, D. W. (2003). A comparison of ordinary least squares and logistic regression. The Ohio Journal of Science, 103(5), 118–125.
Pope, G. (1989). Hospital nonprice competition and medicare reimbursement policy. Journal of Health Economics, 8, 147–172.
Scanlon, W. J. (2006). The future of medicare hospital payment modest proposals in light of medicare’s challenges. Health Affairs, 25(1), 70–80.
Shleifer, A. (1985). A theory of yardstick competition. The Rand Journal of Economics, 16(3), 319–327.
Siciliani, L. (2006). Selection of treatment under prospective payment systems in the hospital sec- tor? Journal of Health Economics, 25(3), 479–499.
Silverman, E., & Skinner, J. (2004). Medicare upcoding and hospital ownership. Journal of Health Economics, 23(2), 369–389.
Silverman, E., Skinner, J., & Fisher, E. (1999). The Association between for-profit Hospital Ownership and Increased Medicare Spending. The New England Journal of Medicine, 341(6), 420–426.
Simborg, D. W. (1981). DRG creep: a new hospital-acquired disease. New England Journal of Medicine, 304, 1602–1604.
Steinbusch, P. J., Oostenbrink, J. B., Zuurbier, J. J., & Schaepkens, F. J. (2007). The risk of up-coding in casemix systems: A comparative study. Health Policy, 81, 289–299.
Steinwald, B., & Dummit, L. (1989). Hospital case-mix change: Sicker patients or DRG creep? Health Affairs, 8, 35–47.
Xirasagar, S., & Lin, H.-C. (2006). Effects of payment incentives, hospitals ownership and competition on hospitalization decisions for ambulatory surgical procedure. Health Policy, 76, 26–37.
Acknowledgements
I would like to thank the team of the ATIH French Statistical Agency for Hospital database and EMR, Ministry of Health for their expert advice and support throughout this project.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
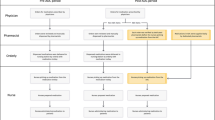
Appendix 2: French DRG 2009-classification and DRG based payment
Description of the new French DRG coding system
2009-French DRG classification system is organized in a nested fashion. DRGs are coded by a series of 6 characters. The first two characters define the pathology; the third defines the type of medical practice (medical, surgical, or exploratory); the fourth and fifth characters define the subfields of a given pathology; and the sixth character defines the level of severity of which there are four. The level of severity is independent of the procedures performed on the patient.
The “root” of a DRG consists of the first 5 characters in the corresponding code. There are 617 root DRGs in 2009-classification. Among these roots, 76.2% (470) are subdivided into 4 levels of severity. In addition, certain DRG roots are not subdivided into four severity levels, or are not subdivided by severity at all. Moreover, there exist, in some specific cases, other types of subdivisions that replace or complement subdivision by severity (Manuel des GHM 2012).
This classification defines four levels of severity
-
Level 1: stays without associated complications or morbidity (ACM) belonging to a list validated by consultative and decisional bodies of the national health statistics agency. In what follows, this level is called low or non-severe.
-
Level 2, 3 or 4: The list of ACMs contains three sub-lists corresponding to three levels of severity. An ACM always belongs to a single severity level, which does not change. In certain cases, death can also play the role of ACM. In the grouping algorithm, the order of priority is as follows. – Existence of an ACM and its placement at a given level (2, 3, or 4);—Patient’s age (< 2 years, > 69 years and > 79 years); – Death if neither of the two preceding conditions is satisfied; – Duration of stay, which is a mandatory condition.
-
Other types of subdivisions
-
The letter “Z” indicates an exploratory stay, with no coding of severity. These stays are almost exclusively chemotherapy sessions and dialysis sessions;
-
The letter “E” indicates stays ending in death;
-
The letter “J” identifies ambulatory surgical stays (no overnight stay);
-
The letter “T” corresponds to short stays, between 1 and 3 days. These must be distinguished from stays coded by a “J”. These are almost exclusively medical stays.
In the primitive 2009-classification of the coding system (before any marginal adaptive changes), used here, stays were classified into 2192 DRGs.
DRG prospective payment system
DRGs are used as a tool to measure the relative resource requirements for hospital care of the population. Hospitals are paid a fixed price for each patient admitted in hospital. At discharge, every patient’s stay is assigned to one of the DRGs based on their routinely registered primary diagnosis. At each DRG is associated a weight reflecting the average cost of patients in the given DRG relative to that of the average patient reimbursed by the system (MedPAC 2005). The price for each patient treated is obtained by multiplying the relevant DRG weight by a fixed monetary value. With the DRG system, hospitals are expected to reduce costs and under certain conditions, to incent increase in activity.
They were first adopted in 1983 for the reimbursement of care provided to elderly patients under the US Medicare Program. Since then, the development of DRG systems and DRG-based hospital payments has become an international phenomenon (Kimberly et al. 2008). In Europe, prospective payment based on DRGs was first introduced in Portugal in the late 1980s, and more recently in other European countries such as England, France, and Germany. The principal reason for the popularity of DRG-based hospital payment systems is that they are supposed to lead to eciency: reduced costs for the optimum level of quality.
DRG-based hospital payment creates three main incentives.
-
One of the incentives of DRG-based payment is for hospitals to reduce costs per patient. This can happen through: (i) reductions in lengths of stay; (ii) reductions in the intensity of services provided; and (iii) patient selection. Using French data, the empirical literature showed that in public hospitals both the number of cases treated and case-mix-adjusted production increased significantly between 2004 and 2009. This coincided with a decrease in lengths of stay (DREES 2012a, b; Or et al. (2013), Gobillon and Milcent 2015).
-
The second incentive is to increase the number of patients: the reduction of the waiting list, splitting care episodes into multiple admissions, admitting patients for unnecessary services (known as induced demand), and improving hospital reputation. According to DREES (2012a, b), the volume of admissions increased by about 14.6% over the period 2001–2009.
-
The third is to increase revenue per stay. Hospitals can achieved this using one of two strategies: (i) changes in coding practices, or (ii) changes in practice patterns. The aim of both strategies is to reclassify patients into higher-severity DRGs with a higher associated payment rate, a phenomenon known as “upcoding”. With the data used here, which includes 15 million observations, the effect of changes in coding practices can be isolated and assessed purely independently of all other incentives.
Rights and permissions
About this article
Cite this article
Milcent, C. From downcoding to upcoding: DRG based payment in hospitals. Int J Health Econ Manag. 21, 1–26 (2021). https://doi.org/10.1007/s10754-020-09287-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-020-09287-x