Abstract
John Davis (New Methuselahs: The Ethics of Life Extension, The MIT Press, Cambridge, 2018) advances a novel ethical analysis of longevity science that employs a three-fold methodology of examining the impact of life extension technologies on three distinct groups: the “Haves”, the “Have-nots” and the “Will-nots”. In this essay, I critically examine the egalitarian analysis Davis deploys with respect to its ability to help us theorize about the moral significance of an applied gerontological intervention. Rather than focusing on futuristic scenarios of radical life extension, I offer a rival egalitarian analysis that takes seriously (1) the health vulnerabilities of today’s aging populations, (2) the health inequalities of the “aging status quo” and, (3) the prospects for the fair diffusion of an aging intervention over the not-so-distant future. Despite my reservations about Davis’s focus on “life-extension” vs. increasing the human “healthspan”, I agree with his central conclusion that an aging intervention would be, on balance, a good thing and that we should fund such research aggressively. But, I make an even stronger case and conjecture that an intervention that slows down the rate of molecular and cellular decline from the inborn aging process will likely be one of the most important public health advancements of the twenty-first century. This is so because aging is the most prevalent risk factor for chronic disease, frailty and disability, and it is estimated that there will be over 2 billion persons age > 60 by the year 2050.
Similar content being viewed by others
Introduction
In his recent book New Methuselahs: The Ethics of Life Extension, John Davis advances a novel ethical analysis of longevity science that employs a three-fold methodology of examining the impact of life extension on three distinct groups. Davis categorizes these groups as follows:
-
(1)
the “Haves”: people who have access to life extension because they can afford it;
-
(2)
the “Have-nots”: people who do not have access to life extension because they cannot afford it; and
-
(3)
the “Will-nots”: people who have access to life extension but chose not to take it.
The scope and depth of Davis’s analyses are impressive and worthy of serious engagement as we contemplate what would constitute a socially responsible regulation of potential “aging” interventions. In terms of his central conclusion in New Methuselahs— namely, “that developing life extension is, on balance, a good thing and that we should fund life extension research aggressively" (Davis, 2018, p. 4)—I am in complete agreement. But I would go further by adding that an intervention that retards human aging will likely be one of this century’s most significant public health interventions.Footnote 1 This is the case because aging is the largest risk factor for diseases like heart disease and stroke, cancer, diabetes, and Alzheimer’s, as well as COVID-19 mortality, and frailty and disability.
Rather than characterizing, as Davis does, an aging intervention as a form of “life extension”, in this article, I argue that an ethical analysis of an aging intervention should focus on what the primary health impact of such an intervention would likely have on population health— namely, increasing the human healthspan so that the risks of disease, frailty and disability would be reduced in late life. A by-product of such an intervention is that it may increase the number of years people also live. Referring to an applied gerontological intervention as a radical or even a moderate form of “life extension” is vague and presents numerous problems and limitations in terms of developing a sage ethical analysis of such a technology.
While the concept of the human “healthspan” is contentious and has its limitations (Kaeberlein et al., 2018), it is recognized by advocates of biogerontology/geroscienceFootnote 2 as an effective way to frame the benefits of altering aging to broader scientific and lay communities. Any reference to “healthspan” in this article is meant to refer to “the period of life spent in good health, free from the chronic diseases and disabilities of aging” (Kaeberlein, 2018, p. 363). By contrast, “life extension” is a vague concept because it is not clear if it simply means delaying death by keeping a person of advanced age alive by managing disease, frailty and severe disability vs. increasing the years of healthy life and delaying and compressing the period of frailty, disease and disability in late life. The former merely increases the lifespan, whereas the latter is an increase in the healthspan.
Furthermore, there are significant epistemic constraints on any ethical analysis of a technology that has the potential to add hundreds of years to life expectancy—namely, we would not know:
-
(1)
that such a technology was even capable of adding hundreds of years of life until after hundreds of years had actually passed and at least some individuals who took the aging intervention were still alive to confirm that the intervention was an effective form of radical life extension.
-
(2)
how the general moral landscape will have been altered from its current state to the new realities of a future 2–300 years from now.
Rather than deploying an egalitarian analysis into the far future of a potential new longevity-caste society, I believe it is more prudent and practical to deploy such an ethical analysis to the intrinsic health inequalities that exist between persons at different stages of the human lifespan [e.g., between young adults (age 20–30) and older persons (age > 85)], as well as the health inequalities that already exist with respect to variations in the rate of biological aging.
In this essay, I will deploy a comprehensive “present-day” (vs. futuristic) egalitarian analysis that highlights the health consequences of the “status quo” of biological aging, including the health inequalities that exist between persons with “accelerated” aging (e.g., progeria), “normal” aging, and “retarded” aging (e.g., centenarians and supercentenarians). Doing so can help re-frame the ethical arguments concerning intervening in aging, so that an applied gerontological intervention is recognized as a significant form of preventative medicine, rather than a technology that raises serious concerns about radical life extension, boredom, or the creation of a new caste system between the “longevity-haves” and “have-nots”.
While the egalitarian analysis I deploy to champion the case that there is a pressing moral imperative to retard aging coheres with the same substantive conclusion Davis arrives at—namely, that an aging intervention should be researched aggressively—I believe the more effective strategy to deploy to convince sceptics of that conclusion is one that emphasizes the magnitude of the (global) health challenges (i.e., the prevalence of chronic disease, frailty and disability) facing the world’s aging populations if we do not alter the inborn aging process.
The Ambiguity of “Life Extension”
When advocating for greater public support and increased research funding, scientists in different areas of scientific study will often highlight the health risks that could be abated by the knowledge and potential applied technologies of their field of study. For example, cancer researchers note that nearly 10 million people die each year from cancer (Ferlay et al., 2020). Because most people personally know someone whose health has been adversely impacted by cancer, it is not difficult for most people to conceptualize the magnitude of the benefits improvements in cancer prevention and treatments could yield. Similarly, greater public awareness of the impact climate change has on increased heat waves and draughts, more intense and frequent hurricanes, changes to global sea levels, etc. has helped environmentalists lobby for greater investments in climate change research and policy initiatives concerning things like renewable energy and reducing our reliance on fossil fuels.
Tackling cancer and climate change are considered pressing global health imperatives because they are framed as interventions that can help “prevent loses” vs. merely “adding benefits”. No one who wishes to sway the general public and policy makers to tackle cancer and climate change more seriously would describe the potential benefits of doing so as “life extending” interventions, though both would extend the life of many people. There is good reason for this, given that findings in behavioural economics [“prospect theory” (Kahneman and Tversky (1979)] have revealed that preferences are in fact dependent on whether particular outcomes of a choice are regarded as ‘‘a loss’’ or ‘‘a gain’’, relative to a reference point [or ‘‘aspiration level for survival’’ (Farrelly, 2010)]. This means that the harms from cancer (e.g. cancer mortality) and other diseases of aging are typically considered as “losses” because the reference point most people internalize is a “cancer-free” existence. Thus the prevention of cancer is highly valued when construed as a cause of “premature” death.
But when the framing of the benefits of an applied gerontological intervention invokes “adding years of life” the stakes are construed as “gains” in terms of additional life years (vs. disease prevention). Prospect theory contends that the value attributed to receiving such benefits will be skewed when they are perceived as exceeding the “aspirational level for survival”. However, when an aging intervention is framed in public health terms, as a form of preventative medicine, this helps fixate the focus on the most morally salient features of such an intervention—namely, its potential to prevent or delay the onset of disease, frailty, and disability by increasing the healthspan (a side-effect of which may be an increase in the number of years lived).
Unlike cancer research and environmental science, geroscience faces a number of public relations challenges other areas of science do not face. Firstly, no one officially dies from aging, which creates a challenge when framing what the goal of an applied gerontological intervention would be. It cannot be considered a “life saving” medical intervention if there is no one who officially dies from aging. “Since 1951, the year all state and federal agencies in the United States were required to adopt a standard list of contributing and underlying causes of death, no one in the United States died from “old age” (Hayflick, 2003, p. 1). If aging is not considered a cause of death, then it is challenging to conceptualize it as a “loss”.
Secondly, the aspiration to alter human aging does not always elicit a strong, positive emotional response, at least in part because there is an ambiguity behind the general aspiration of “life extension”. For example, is the aspiration one of immortality, or at least biological immortality?Footnote 3 Or is the aspiration to simply extend the period of frailty, disease and disability at the end of life by delaying death for as long as possible? Because the aspiration of “life extension” lacks precision, talk of “life extension” typically raises a wide array of intuition-based concerns (the type Davis addresses), such as whether we would be bored living hundreds of centuries, or how this would likely impact the global population size and environment, etc., or if this would create a new caste society between those with “normal life” and those with “extended life”.
To help ensure an ethical analysis of an applied gerontological intervention is empirically and morally sound, I believe it is imperative to “frame” an aging intervention within the context of the present-day health predicaments facing the world’s aging populations, as well as the current knowledge of the biology of aging and what (at least the first generation of) an aging intervention is likely to be and do. So rather than contemplating scenarios of radical life extension (of people attaining biological immortality or living thousands or even hundreds of years), let us consider two, more plausible, future scenarios.
The two scenarios I will invoke are designed to prime contrasting moral sensibilities, and the purpose of this is to show how powerful the “framing” of the prospect of “life extension” can be in terms of either repelling us from, or winning us over to support, longevity science. The first scenario (Scenario 1) describes what many would take to be a dystopic life extension future, and the second scenario (Scenario 2) is a more utopian one.
Scenario 1: Extended Life = Extended Survival (accompanied by extended and more severe frailty, disease and disability)
Over the next half a century, population A increases its life expectancy at birth by 40 years, from age 80 to age 120. This increase in life expectancy is primarily achieved by simply forestalling death in late life. The procurement of additional decades of life in late life is achieved not by altering aging, but from advances in improving survival to the upper limits of maximal longevity. Through a combination of novel and expensive drug development, coupled with extensive public health expenditures in long-term care facilities and palliative care, patients can now survive for decades on chemotherapy and radiation, reliant upon ventilators, etc. enduring dementia and other severe diseases, frailty and disability for decades. The majority of the people surviving past age 110 have little psychological continuity to their former selves, as new diseases of the brain emerge with the extreme longevity achieved (but with minimal improvements in treating these cognitive disorders).
The only real achievement for population A in this scenario, from a population health perspective, is increased survival and a prolongation of the period of disease, frailty and disability in late life. The “longevity dividend” (Olshansky et al., 2006) achieved in society A is very costly, with ever increasing healthcare expenditures being invested in preventing death in late life with little to no regard for the “quality of life” of people in late life. Family members learn to normalize the practice of spending many decades visiting family members in long-term care facilities, and those family members over age 100 typically can not live independently and many are no longer capable of actively participating in family life.
Consider now a contrasting future of life extension:
Scenario 2: Extended Life = Extended Healthspan (increasing health and decreasing frailty, disease and disability).
Over the next half a century, population B increases its life expectancy at birth by 40 years, from age 80 to age 120. This increase in life expectancy is primarily achieved by extending the human healthspan, which means a substantive delay and compression of disease, frailty and disability in late life. The procurement of additional decades of life is achieved by a relatively inexpensive drug that re-programmes the human metabolism to mimic the longevity effects of caloric restriction (without people having to endure the deprivation of actually consuming less calories than that required for a normal diet). With this public health advancement it takes the average person 120 years to biologically age what use to be achieved in 80 years. Furthermore, at the end of life there is a compression of morbidity, meaning the period of time people suffer age-related health maladies (e.g., disease, frailty and disability) is shorter than the period they experienced before the aging intervention. Thanks to this anti-aging drug, most people will be capable of working well past age 100, though many decide to spend the additional years of healthy life volunteering in their communities, helping out with childcare duties for their grand and even great grandchildren, etc.
People in this second scenario enjoy more health in late life, and thus the “longevity dividend” in population B also brings significant economic benefits. By expanding the opportunity for people remaining productive in late life, and reducing the public expenditures typically spent helping persons manage the co-morbidities of late life, population B reaps significant economic as well as health benefits.
The two contrasting scenarios of populations A and B are deliberately exaggerated in terms of stark negative and positive health and economic outcomes to reveal how such details activate different moral sensibilities in terms of our considering the desirability of “life extension”, for both individual lives and populations. Population A realizes perhaps the worst outcome most people could envision for aging populations—prolonging the suffering, disease, and frailty of diminishing health in late life at an exorbitant social cost. Such a society fanatically values “quantity” of years survived over the “quality” of the life lived, something most people would disagree with. Surviving many additional decades of life with progressive and severe infirmities and minimal psychological wellbeing is not something most people would see as a desirable outcome.
The “longevity dividend” realized in scenario A is one that prioritizes “adding years to life” instead of “adding life to years”. Scenario A is not a cost-effective, nor morally laudable, aspiration. The quality of life secured by the 40 year increase in longevity is very relevant to our assessment of the value of such an increase in the lifespan. With the details provided in Scenario A, many people might (reasonably) take the view that the society would have been better off not aspiring to increase life expectancy further than the original age of 80 years.
In scenario B the “longevity dividend” is the opposite of that in A. Population B realized the goal of “healthy aging” vs. simply delaying death. The health benefits secured in B are meaningful and substantive because people enjoy more health, and thus life extension is simply a by-product of increasing the healthspan vs. the intended goal. The preamble to the Constitution of the World Health Organization defines “health” as follows: “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (2006). The Constitution goes on to affirm that “the enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition” (World Health Organization, 2006). Adding health to late life, rather than simply “life extension”, is the goal of biogerontology. Making this point explicit permits us to more effectively address the “inequality of access” concern which is one of the foundational concerns of Davis’s analysis of the ethics of life extension.
The Vulnerability and Inequality of the “Aging Status Quo”
The global population is approaching 8 billion people. Life expectancy at birth for a baby born in the world is currently age 73 (World Health Organization, 2021a), and expected to rise to age 81 by the end of the century (United Nations, 2011, p. xviii). While there still persists substantive health inequalities between the world’s richest and poorest countries—in terms of the early and mid-life mortality risks the latter face from infectious diseases (HIV/AIDS, malaria, tuberculosis, etc.), poverty (e.g., the lack of clean drinking water, malnutrition, and basic healthcare services), conflict, etc.—most humans this century will live beyond age 70 and will die from the chronic diseases associated with late life. Cardiovascular diseases are the leading cause of death in the world, responsible for an estimated 17.9 million deaths (31% of all deaths) each year (World Health Organization, 2021b). Chronic diseases like cancer and cardiovascular disease are complex diseases, meaning they are influenced by many factors (genes, environment, lifestyle, etc.), but the most significant risk factor for chronic diseases is age. Even for an infectious disease like COVID-19, age is the most significant risk factor for death and serious illness. By the end of 2020, The World Health Organization estimated the global death toll from COVID-19 to be > 1.8 million deaths. The Centers for Disease Control and Prevention in the United States estimates that 80% of the deaths that have involved COVID-19 in the US occurred among persons age 65 and older (Centers for Disease Control and Prevention, 2020).
The aging of today’s global populations is both a incredible success story—as this indicates that significant improvements have been made with reducing the mortality risks of early life—but it also represents significant and unprecedented health and economic challenges. Shifting demographics, fuelled by populations surviving longer into late life and lower birth rates, will have a significant impact on both healthcare expenditures and the productive capacities of the workforce of the future.
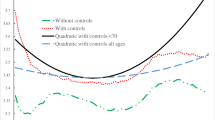
Instead of considering the speculative scenario of a far-off future with unequal access to “life extension”, as Davis does in New Methuselahs, an egalitarian analysis can also be applied to (1) the variation in health risks persons typically face over the lifespan in the “here and now” and (2) the spectrum of variations in the rate of biological aging in the “aging status quo” (that is, before the development of an aging intervention). I will deploy two such analyses, the first provides a synchronic snapshot to amplify the significance of promoting healthy aging given that older persons are most at risk for chronic disease, frailty, and disability. The second analysis I develop is a diachronic egalitarian analysis that reveals the existing health inequalities that arise from variations in the rate of biological aging. The latter will be the focus of the next section. I believe these “present-day” egalitarian analyses of the aging status quo ought to be the central focus of an ethical analysis of a potential aging intervention.
In this section, I will focus on a synchronic snapshot of health inequalities over the course of the human lifespan in developed countries like the United States. This is revealed most starkly in the mortality and morbidity risks facing the following two groups (Group A and Group B). Group A faces very low risks of mortality. The vast majority of persons in this age category are expected to still be healthy and alive over the next 5 years. This contrasts with the persons in group B, a sizeable portion of which are not expected to survive the next 5 years, and the majority of those who do survive will face high risks of disease, frailty, and disability over the next 5 years.
To make the numbers more concrete, the health inequality between groups A and B will be illustrated by the actual risks of death from two specific diseases, which are illustrative of the more general health risks the two groups face. The two diseases are cancer and COVID-19. In 2019, the cancer death rates per 100,000 people in Group A was only 9.4 vs. 1571.0 for persons in Group B (Centers for Disease Control and Prevention, 2020). That means Group B has 167 × as many cancer deaths per 100,000 people as Group A. With respect to COVID-19 risks, persons in Group B have mortality risks 370 × that of persons in Group A, and 10 × more hospitalizations (Centers for Disease Control and Prevention, 2021).
The health inequalities between these two groups are not limited to just cancer and COVID-19, but also apply to most of the prevalent diseases and disorders in the United States. What risk factor could be so significant that it leads to such health disparities in the 5 year mortality and morbidity risks between these two groups? Is it race? No. Is it gender? No. Is it socio-economic status? No. It is age. The cancer death rate cited was for persons ages 20–29 (Group A) and persons age 85 and over (Group B), and for COVID-19 the Centers for Disease Control and Prevention’s latest estimate for persons ages 18–29 (Group A) and age 85 and over (Group B).
The health inequalities between young adults and older adults does not stem, at least primarily, from socio-cultural factors. It is not simply “lack of access to healthcare”, or “institutional ageism” or the “past lifestyle choices of older persons” that explain the magnitude of the health inequalities between groups A and B (though all three are real factors that can exacerbate these health inequalities). The most significant causal factor at play is evolution by natural selection. “Natural selection has not shaped organisms for maximum health, but rather to maximise their reproductive success (or genetic fitness)” (Wells et al., 2017, p. 500).
Aging is “the progressive loss of function accompanied by decreasing fertility and increasing mortality with advancing age” (Kirkwood & Austad, 2000, p. 233). The evolutionary biologist Theodosius Dozhansky (1973) famously remarked that “nothing in biology makes sense except in the light of evolution”. Dozhansky’s insight applies to aging itself. Why do we, or sexually reproducing species more generally, age? Sexually reproducing species have an evolutionary history that prioritized reproduction over the somatic maintenance needed for indefinite survival. This means that the force of natural selection acts more weakly to reduce mortality at older ages, which means that genes that cause deleterious affects in later life are much more prevalent in the population that those genes that cause early onset maladies and reduce reproduction.
The two main theories of the evolution of aging are the mutation accumulation theory (advanced by Peter Medawar, 1952) and the antagonistic pleiotropy theory [advanced by George Williams (1975)]. The dominant version of the latter is known as the disposable soma theory (Kirkwood, 1977; Kirkwood & Holliday, 1979). This theory posits that the winning evolutionary strategy for sexually reproducing species, species that have had to find ways to survive the extrinsic risks of the hostile environments of life on this planet, is to prioritize health during the “essential lifespan”. The “essential lifespan” of a species is defined as the time required to fulfill the Darwinian purpose of life, that is, successful reproduction and continuation of generations (Rattan, 2000).
A species’ “essential lifespan” determines its biological warranty period—“biological warranty periods are an inadvertent by product of evolutionary neglect, and genetic programs for growth, development and reproduction” (Carnes et al., 2003, p. 43). Data on longevity among extant hunter-gatherers and forager-horticulturalists (Gurven and Kaplan (2007), coupled with biological evidence (Carnes et al., 2003) concerning the risks of infertility, disease, frailty, disability and death supports the conjecture that humans have a biological warranty period of approximately 70 years. Framed within insights from the evolution of aging, the declining forces of natural selection are the ultimate (or evolutionary) causation of the inequality between the intrinsic health risks facing humans during the reproductive and post-reproductive years. These health inequalities are (1) significant, they are also (2) unchosenFootnote 4 and, in a scenario where a safe and effective aging intervention exists, these inequalities are (3) ameliorable.
The critic might raise what I believe is a reasonable objection to my highlighting the intrinsic health inequalities between young and older adults. Namely, that the young eventually get older and thus there is no troubling health “inequality” when we take a diachronic (vs. synchronic) perspective of the complete lifespan. “As a group the young eventually get older, and thus, because aging is universal, it does not threaten equality of opportunity for health” our critic might contend. There is some sage insight in this critic’s response, but I think this objection has only partial (but not full) success in undermining the concerns raised above in the synchronic snapshot of health inequalities between young and older adults. The central premise behind the moral duty to retard human aging is simple and persuasive—as the World Health Organization’s Constitution maintains, the right to health is a human right. This right applies to persons at all stages of the human lifespan, including older persons. If an aging intervention which increased the human healthspan could be developed, access to such an intervention should be considered as an “essential” medical necessity, in accordance with the right to human health.
How global access to an applied gerontological intervention could be feasibly realized of course presents significant logistical challenges. Much depends on the specifics of the type of intervention it is (e.g., a drug that modulates the rate of biological aging vs. genome surgery). Currently, the focus of geroscience is on targeting the aging process via generic drugs that are off-patent (e.g., metformin) and thus significantly cheaper. Much like the COVID-19 vaccines during the recent pandemic, there would need to be global collaboration to ensure that poorer regions of the world can gain access to an applied gerontological intervention. There is not adequate space here to consider the specifics of how that could best be achieved, but I acknowledge the challenges will be significant and largely dependent on the type of intervention in question.
The critic’s objection also mistakenly equates equality with respect to chronological aging (which is universal and constant for all) with biological aging. While everyone does biologically age, there is a vast health inequality between those who biologically age at an accelerated rate (e.g., such as children with progeria and, to a lesser extent, adults with diabetes and/or obesity), normal aging, and decelerated aging (e.g., centenarians and supercentenarians, as well as eunuchsFootnote 5). I will now develop a diachronic egalitarian analysis of the “aging status quo”, one which emphasizes the health disparities that already exist with respect to the rate at which people biologically age.
The synchronic egalitarian analysis explored in this section certainly does yield some radical, counterintuitive conclusions, conclusions I would actually resist endorsing. My exploration of the synchronic egalitarian analysis is not meant to be an endorsement of it, but rather to show that it can help reveal the health vulnerabilities of aging (something an ethical analysis of longevity science ought to acknowledge). One problem with a strictly synchronic egalitarian stance, applied to the health risks over the lifespan, is that it would not be able to distinguish between the moral urgency to aid in those cases when much more significant health benefits could be realized. For example, mitigating the health vulnerabilities of a child vs. a person in later life should be considered a more pressing duty when the former could confer significantly more years of healthy life vs. the later.
Elsewhere (Farrelly, 2016), I defended a duty to mitigate the health vulnerabilities of aging by invoking a duty to aid that takes seriously a number of operational-level concerns, such as the probability of success, the cost of intervening, and also the magnitude of the benefits likely to be realized. The age of those aided can be morally relevant to the latter consideration. But from this broadly utilitarian perspective the sheer number of persons living into late life generates a pressing moral duty to mitigate the harms of senescence. I think this is a much more effective way of framing the duty to tackle aging vs. invoking an appeal to a synchronic egalitarian lens.
The Genetic Lottery and Aging
The motivation behind Davis’s addressing the ethical implications of life extension are two-fold. Firstly, he is concerned about the potential injustices unequal access to such technologies would exacerbate. Secondly, he is concerned with the potential adverse effects even a modest retardation of the rate of aging might have on the world’s population size (what he calls the “Malthusian crisis”). For the purposes of this essay my attention is directed solely to the first issue, which I will call the inequality concern. Davis remarks that “the literature on life extension ethics is laced with comments about unequal access to life extension, dividing society into castes of mortals and near-immortals, making inequality worse, allowing dictators to live forever, and similar concerns.” (2018, p. 3). In my opinion, the fixation the literature has had on futuristic predictions about increasing health disparities is disconnected from an empirically-informed ethical analysis which takes seriously both the existing health inequalities of the “aging status quo” as well as where the science of aging actually is today and the type of technology it will most likely yield (at least in the foreseeable future). Attending to these empirical realities, vs. more speculative futuristic scenarios, can yield, I will now argue, more sage moral judgements and assessments about the likely impact of an applied gerontological intervention.
Rather than fixating an ethical analysis on “life extension”, the focus should be on the realization of health itself. The Constitution of the World Health Organization defines “health” as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (World Health Organization, 2006). The goal of an applied gerontological intervention is thus “healthy aging” vs. “life extension”, though a consequence of enjoying more health in advanced life would be more life. The United Nations has designated 2021–2030 the “Decade of Healthy Ageing”. Insights from biogerontology must thus be an integral part of the effort to increase health in late life if the aspiration of “health aging” is to be a feasible reality for the world’s aging populations.
Aging is the major risk factor for the most prevalent chronic diseases and disability in late life, and thus it should now be a major focus and target of biomedical research. Rather than developing (as Davis does) an ethical analysis of an aging intervention focused primarily on the potential concerns of future access to radical life extension, I will instead develop a diachronic egalitarian analysis that reveals the prevalent health inequalities that already exist between persons who biologically age at different rates.
While everyone chronologically ages at the same rate (i.e., 1 year every 365 days), we do not biologically age at the same rate. For example, children born with the rare and early onset fatal disease of progeria (Hutchinson–Gilford syndrome) have accelerated biological aging. About 1 in 4 million children are born with this rare condition, that is caused by a genetic mutation in the LMNA gene. These children suffer extreme premature aging and have an average life expectancy of around 13–14 years. This means that the rate of biological aging that results from this “genetic lottery” can reduce life expectancy by approximately 7 decades compared to people with “normal aging”.
Progeria is the most extreme example of accelerated aging. Diabetes is a metabolic condition that has long been recognized as another form of “accelerated aging” (Morley, 2008). Obesity has also been described by some as a form of accelerated aging. In their review of how obesity and aging are “two sides of the same coin”, Tam et al. (2020) contend that both obesity and aging promote cellular senescence, inflammation, mitochondrial dysfunction, the aggregation of misfolded proteins, the attrition of telomeres, etc. Obesity-related diseases are estimated to increase the chances of dying and lessen life years by 0.2 to 11.7 years depending on gender, race, BMI classification, and age (Chang et al., 2013).
Furthermore, the health effects of differential rates of biological aging might actually be manifest by mid-life, and not just late life. A recent study followed a cohort of 1037 infants born in the same year to age 45 and found that people who are aging more rapidly than same-age peers in midlife may prematurely need supports to sustain independence that are usually reserved for older adults (Elliot et al., 2021).
The majority of the population has a biological warranty period of approximately 70 years, and we can describe that as “normal aging”. In developed countries, survival goes well beyond age 70, due to improvements in healthcare and medical technologies that can help older persons manage the diseases, frailty and disabilities of late life. Jeffrey Fries explains how estimates of the human lifespan are arrived at, and suggests that the average life span is approximately 85 years:
There are several methods of estimating the human life span. One may use the anthropological formulas, reconstruct an ideal survival curve from the tail of the present curve using the assumption that these individuals have been essentially free of disease, make extrapolations from the rectangularizing survival curve, or use estimates based on observed decline in organ reserve. All suggest an average life span of approximately 85 years, with a distribution which includes 99 percent of individuals between the ages of 70 and 100. (Fries, 2005, p. 808)
In addition to accelerated and normal aging, there is another category of persons that naturally have decelerated aging. These are the longest lived humans, such as centenarians (age ≥ 100) and supercentenarians (age ≥ 110). Jeanne Louise Calment, who died at age 122 in 1997, was the oldest person whose age has been verified by official documents. In the case of persons with such exceptional longevity genetics appears to play a major factor. Having a centenarian sibling increases one’s chances of survival to very old age (Perls et al., 1998, p. 1560). The offspring of long-lived parents have significantly lower prevalence of hypertension (by 23%), diabetes mellitus (by 50%), heart attacks (by 60%), and strokes (no events reported) than several age-matched control groups (Atzmon et al., 2004).
The prevalence of supercentenarians (age ≥ 110), and even centenarians (age ≥ 100), is very low. In the United States and other industrialized nations, centenarians occur at a prevalence rate of about 1 per 6000. Supercentenarians occur at a rate of about 1 per 7 million.Footnote 6 With centenarians there are three different categories of centenarians: “delayers”, “survivors” and “escapers” (Evert et al., 2007). The “delayers” are people who make it to 100 years with a delay of the onset of common age-associated illness. For “survivors”, these are people who were diagnosed with an illness prior to age 80, but survived for at least two more decades. The third category of centenarians are “escapers”, people who escaped the most lethal diseases, such as heart disease, non-skin cancer and stroke.
The longest lived persons can enjoy more than 20 years of additional healthy life compared to persons with normal aging, and almost a century of more life than the children born with the accelerated aging of progeria. The aging “status quo” is thus very unequal in terms of the health prospects people can have. Being born with progeria means accelerated aging and death before age 20. By contrast, individuals born with “longevity genes” may live over a century of disease-free life. The latter enjoy substantively more health in late life than the typical person who was not born with the genes for exceptional longevity. The longest lived persons who enjoy a century of disease-free life could be considered the “Haves”, and the other 99% + of the population the “Have-nots” when it comes to exceptional healthy aging. This inequality should be abated, if it is possible to do so. And not by simply treating the accelerated aging of progeria (though that ought to be a moral aspiration as well), but by modifying normal aging to increase the human healthspan and compress the disease, frailty and disability of late life. An applied gerontological intervention might help us realize such a state of affairs, permitting the average person to enjoy the extended healthspan that only some rare individuals naturally enjoy today.
This diachronic egalitarian analysis of the aging status quo thus reveals the troubling health inequalities that already exist vs. fixating our attention on the potential new inequalities that an aging intervention might create in the future. The latter is certainly a concern that an ethical analysis of an aging intervention should address, but it must be done in conjunction, I believe, with an egalitarian analysis of both the health vulnerabilities and health inequalities of the existing aging status quo. In the final section, I directly address the concern Davis addresses—that is, the potential an aging intervention might have to exacerbate inequality. I argue that much depends on the type of technology an applied gerontological intervention is. Based on the type of aging interventions currently being developed (i.e., drugs that target the aging process), I conclude that there is good reason for being optimistic than an applied gerontological intervention would not be a technology that is inaccessible to the poor for prolonged periods of time. But justice does require that the global poor have access to an intervention that promotes healthy aging, given that it would have such a significant public health and economic impact on the world’s aging populations.
Technological Progress and the Future
Davis’s ethical analysis of longevity science employs a three-fold methodology of examining the impact of life extension on three distinct groups: the “Haves”, the “Have-nots” and the “Will-nots”. There are a number of epistemic limitations that constrain our ability to competently theorize the future (especially the distant future) of any technology, including potential “life extending” technologies. Space travel, food and energy technology, artificial intelligence, not to mention new technological breakthroughs beyond our current imagination, all of these innovations will be evolving simultaneously over the next century, along with potential aging interventions.
Of course the human mind can, and has for at least hundreds of years, conjure both detailed utopic and dystopic futures for humanity. But what these simulations all share in common is that they tend to be mistaken, both about the way technology has evolved and how they have impacted our wellbeing. “Prospection” refers to our ability to “pre-experience” the future by simulating it in our minds (Gilbert & Wilson, 2007, p. 1352). Such simulations are susceptible to many prospection errors, such as being unrepresentative and abbreviated. Contemplating a caste society of longevity “Haves” and “Have-nots” is prone to such prospection errors. Such a future is “unrepresentative” for at least two obvious reasons. Firstly, even the “longevity Haves” can die prematurely from accidents, homicide and suicide. They would still be vulnerable to addiction and depression, and disabilities unrelated to aging. They would not autonomically fall into the description of “longevity Haves” until they have survived much longer than what is the average period of time for humans to survive. A more accurate descriptor of such persons would be they constitute a group of persons that face reduced risks of disease and death. But they would not be immortal.
Furthermore, envisioning a caste society of longevity “Haves” and “Have-nots” is abbreviated in that it focuses on a specific time in the future: the time when some people could not afford the technology in question. Suppose someone did this for the COVID-19 vaccines.Footnote 7 They described a world where only the affluent countries had access to the vaccines to protect against a novel and highly infectious virus. Such a description was accurate in the world for the early stages of the year 2021, when developed countries like the US authorized the emergency use of the Pfizer-BioNTech and Moderna COVID-19 vaccines. But within less than a year the World Health Organization had authorized the emergency use of other COVID-19 vaccines, including India’s Covaxin and China’s Sinopharm. COVAX, an initiative to ensure COVID-19 vaccines were distributed equally, also helped ensure that poorer countries received the vaccines. Over the course of the year 2021 many countries that are less affluent than the United States (e.g., Chile, Cambodia, Uruguay, and Brazil) actually exceeded US Covid-19 vaccination rates (given the higher prevalence of vaccine hesitancy in the US) (Ritchie et al., 2020). An ethical analysis of access to COVID-19 vaccines which fixated on only the first month of unequal access to the Pfizer COVID-19 vaccinations is unrepresentative and abbreviated because other vaccines were also developed and rapidly distributed to less affluent countries.
Abbreviated simulations of the future that present technological “inequality” as a persistent long-term problem typically function with inaccurate empirical assumptions about the reality of technological diffusion. Initially new technologies are expensive and only accessible to the richest. But like TVs, cell phones, and computers, most technologies become more widely dispersed over time. Any simulation of the potential longevity inequalities in a few hundred years should recognize the reality that the costs associated with such technologies would alter dramatically over that time. What is cost prohibitive for most today is unlikely to remain that way in a few years, let alone for decades or centuries.
Consider, for example, the costs of a technology like that involved with sequencing the human genome. The estimated cost for sequencing the initial “draft” of the human genome was $300 million dollars in the year 2000. The National Human Genome Research Institute estimates that by 2006 that cost had dropped to just $14 million.Footnote 8 By 2016 the cost to sequence a human gnome had fallen to below $1000. Simulations constructed in the year 2000, about the likely societal impact of sequencing the human genome in the year 2200, based on the estimate that the price would remain $300 million for two centuries, would be completely erroneous. Within less than a decade the costs had changed dramatically. Any long-term estimate of the costs of an aging intervention should also factor in such considerations. There is little empirical basis for conjecturing that some persons will live centuries longer than most others simply because the latter can not afford those technologies when the technologies first come into existence.
Rather than theorizing about a distant future of “extreme longevity-Haves” and “Have-nots”, I believe it is more helpful to theorize about the “here and now”. The first generation of aging interventions are likely to come out of drugs that already exist which have been shown to slow aging in other species (but not (at least yet) in humans), and have also had many decades of study for safety in humans in treatment for maladies other than aging. The two most likely candidates are metformin and rapamycin.
A study like the current TAME (Targeting Aging with Meformin) clinical trial is an excellent example of this. Starting in 2019, TAME is a 6 year clinical trial to test the effects of metformin on over 3000 healthy persons between the ages of 65–79. Metformin is a good candidate for the first aging intervention because of its cost and safety. The drug has been shown to slow aging in other animals, and it has been safely utilized as a pharmacological intervention to help control type 2 diabetes for decades. “Metformin exerts its therapeutic effects, through a number of mechanisms and physiological pathways that resemble those generated by caloric restriction (CR), an experimental model known to extend life span and health span in various organisms” (Novelle et al., 2016, p. 2).
Rapamycin is a drug that was developed from soil on Easter Island and is currently used as a drug to help prevent the rejection of transplanted organs for patients undergoing organ transplant. Recent experiments have found that consuming rapamycin can extend lifespan, including in mammals. In a study of mice (Harrison et al., 2009) it was found that being fed rapamycin increased the median and maximal lifespan of both male and female mice. Since this initial report in 2009, there have been fourteen additional studies showing that rapamycin increased the lifespans of male and female mice and these studies on mouse data demonstrate that this molecule is effective in preventing, even reversing, a broad rage of age-related conditions and thus warrants being described as an “anti-aging” intervention (Selvarani et al., 2020).
Rather than assuming an aging intervention will be prohibitively expensive for most of the world’s aging populations, the current state of drug development on an applied gerontological intervention suggests that an aging intervention may be developed from generic drugs that are off-patent and thus significantly cheaper. Even for patented drugs with a 20 year exclusivity time-frame, the expected costs should come down in time. Assuming an aging intervention will remain the exclusive purview of only the wealthiest people in the world for decades, let alone centuries, is not predicated on plausible or defensible assumptions of how technological advances are diffused. It is easy to envision such a distant two-caste society in our mind, but a sage ethical analysis of longevity science should focus on empirically defensible “real-world” scenarios vs. the dystopic fantasies of science fiction. I believe the latter only obstructs and distracts responsible policy making with regards to an aging intervention.
Conclusion
Like Davis, I believe “that developing life extension is, on balance, a good thing and that we should fund life extension research aggressively”. But unlike Davis, I do not believe the best way to promote societal discussion about, or the policy regulation of, an applied gerontological intervention should begin by contemplating the potential future inequalities radical life extension might potentially create. Instead, I believe an ethical analysis should begin from (1) the existing health vulnerabilities of today’s aging populations, (2) the existing inequalities of the “aging status quo”, and (3) address the most likely aging technology to be developed in the immediate future and reasonable empirical assumptions concerning its fair diffusion.
Aspiring to increase the healthspan, vs. merely delaying death, could constitute an innovative approach to human health and help us realize the noble aspiration of “adding life to years” vs. “adding years to life”. Given where the science is today, the goal of a century of disease-free life is a realistic and compelling aspiration. The priority should be on making an applied gerontological intervention a top public health priority for the world’s aging populations. If we do this, then the 2 billion persons over age 60 by the year 2050 could enjoy more health and a compression of disease, frailty, and disability.
Notes
Many prominent biogerontologists have argued for the significance of targeting the inborn aging process itself vs. focusing exclusively on treatments for specific diseases. See, for example, Comfort (1969), Neugarten and Havighurst (1977), Holliday (1999), Olshansky et al., (2006), Butler et al., (2008), Kaeberlein et al., (2015), Olshansky (2018), Barzilai et al., (2020) and Santesmasses et al., (2020).
I use these two terms interchangeably to refer to an interdisciplinary scientific field of inquiry “which strives to understand how aging enables chronic disease and seeks to develop novel multi-disease preventative and therapeutic approaches” (Kennedy et al., 2014, p. 709).
Meaning the elimination of senescence, so that people do not biologically age beyond young adulthood.
Even though lifestyle choices (e.g., smoking, physically inactive lifestyle) may help contribute to some of those risks they become more significant risks because of the vulnerabilities of the aging process. In other words, a 22 year old physically inactive smoker is not likely to suffer the health consequences of their actions when in their twenties. However, if they continue such an unhealthy lifestyle over the next four decades of aging, the risks of adverse health outcomes increases significantly.
Castrated men residing in a mental hospital lived 14 years longer than intact men in the same hospital (Hamilton & Mestler 1969) and historical Korean eunuchs had an incidence rate of centenarians at least 130 times higher than that of present-day developed countries (Kyung-Jin et al., 2012). Such findings support what the disposable theory predicts to be the case- namely, that longevity comes at a cost to reproductive fitness.
Boston University’s New England Centenarian Study at: http://www.bumc.bu.edu/centenarian/overview.
Or the birth control pill or nutraceuticals, both of which were medical innovations that became widely available to people in poorer countries in timeframes much shorter than centuries.
References
Atzmon, G., Schechter, C., Greiner, W., Davidson, D., Rennert, G., et al. (2004). Clinical phenotype of families with longevity. Journal of the American Geriatrics Society, 52(2), 274–277.
Barzilai, N., Appleby, J., Austad, S., Cuervo, A. M., Kaeberlein, M., et al. (2020). Geroscience in the age of COVID-19. Aging and Disease, 11(4), 725–729.
Butler, R. N., Miller, R., Perry, D., Carnes, B. A., Williams, T. F., et al. (2008). New model of health promotion and disease prevention for the 21st century. British Medical Journal, 337(7662), 149–150.
Carnes, B., Olshansky, J., & Grahn, D. (2003). Biological evidence for limits to the duration of life. Biogerontology, 4(1), 31–45.
Centers for Disease Control and Prevention. (2020). Update on cancer deaths. Retrieved 22 November, 2021, from https://www.cdc.gov/cancer/dcpc/research/update-on-cancer-deaths/index.htm.
Centers for Disease Control and Prevention. (2021). Risk for COVID-19 infection, hospitalization, and death by age group. Retrieved 2 December, 2021, from https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html
Chang, S. H., Pollack, L. M., & Colditz, G. A. (2013). Life years lost associated with obesity-related diseases for US non-smoking adults. PLoS ONE, 8(6), e66550. https://doi.org/10.1371/journal.pone.0066550
Comfort, A. (1969). Longer life by 1990? New Scientist, 11, 549–551.
Davis, J. K. (2018). New methuselahs: The ethics of life extension. Cambridge, MA: The MIT Press.
Dobzhansky, T. (1973). Nothing in biology makes sense except in the light of evolution. The American Biology Teacher, 35(3), 125–129.
Elliott, M. L., Caspi, A., Houts, R., et al. (2021). Disparities in the pace of biological aging among midlife adults of the same chronological age have implications for future frailty risk and policy. Nature Aging, 1, 295–308.
Evert, J., Lawler, E., Bogan, H., & Perls, T. (2007). Morbidity profiles of centenarians: Survivors, delayers, and escapers. The Journals of Gerontology: Series a, Biological Sciences and Medical Sciences, 58(3), M232–M237.
Farrelly, C. (2010). Framing the inborn aging process and longevity science. Biogerontology, 11(3), 377–385.
Farrelly, C. (2016). Biologically modified justice. Cambridge, UK: Cambridge University Press.
Ferlay, J., Ervik, M., Lam, F. et al. (2020). Global cancer observatory: Cancer today. Lyon, France: International Agency for Research on Cancer. Retrieved March, 2021, from https://gco.iarc.fr/today.
Fries, J. (2005). The compression of morbidity. The Milbank Quarterly, 83(4), 801–823.
Gilbert, D., & Williams, T. (2007). Prospection: Experiencing the future. Science, 317(5843), 1351–1354.
Gurven, M., & Kaplan, H. (2007). Longevity among hunter-gatherers: A cross-cultural examination. Population and Development Review, 33(2), 321–365.
Hamilton, J., & Mestler, G. (1969). Mortality and survival: Comparison of eunuchs with intact men and women in a mentally retarded population. Journal of Gerontology, 24(4), 395–411.
Harrison, D. E., Strong, R., Sharp, Z. D., et al. (2009). Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature, 460(7253), 392–395.
Hayflick, L. (2003). Has anyone ever died of old age? New York: International Longevity Centre.
Holliday, R. (1999). Ageing in the 21st century. The Lancet, 354, SIV4.
Kaeberlein, M., Rabinovitch, P., & Martin, G. (2015). Healthy aging: The ultimate preventative medicine. Science, 350(6265), 1191–1193.
Kaeberlein, M. (2018). How healthy is the healthspan concept? Geroscience, 40(4), 361–364. https://doi.org/10.1007/s11357-018-0036-9
Kahneman, D., & Tversky, A. (1979). Prospect theory: An analysis of decision under risk. Econometrica, 47(2), 263–292.
Kennedy, B. K., Berger, S. L., Brunet, A., et al. (2014). Geroscience: linking aging to chronic disease. Cell, 159(4), 709–713. https://doi.org/10.1016/j.cell.2014.10.039
Kirkwood, T. (1977). Evolution of aging. Nature, 270, 301–304.
Kirkwood, T., & Holliday, R. (1979). The evolution of ageing and longevity. Philosophical Transactions of the Royal Society B, 205, 531–546.
Kirkwood, T., & Austad, S. (2000). Why do we age? Nature, 408, (6809), 233–238.
Kyung-Jin, M., Cheol-Koo, L., & Han-Nam, P. (2012). The lifespan of Korean eunuchs. Current Biology, 22(18), R792–R793.
Morley, J. (2008). Diabetes and aging: Epidemiologic overview. Clinics in Geriatric Medicine, 24(3), 395–405.
Medawar, P. (1952). An unsolved problem in biology. H.K. Lewis and Company.
Neugarten, B., & Havighurst, R. (1977). Extending the human life span: Social policy and social ethics. Alexandria, VA: National Science Foundation.
Novelle, M. G., Ali, A., Diéguez, C., et al. (2016). Metformin: A hopeful promise in aging research. Cold Spring Harbor Perspectives in Medicine, 6(3), a025932.
Olshansky, J. (2018). From lifespan to healthspan. Journal of the American Medical Association, 320(13), 1323–1324.
Olshansky, S. J., Perry, D., Miller, R. A., & Butler, R. N. (2006). In pursuit of the longevity dividend. The Scientist, 20(3), 28–36.
Perls, T., Bubrick, E., Wage, C., et al. (1998). Siblings of centenarians live longer. The Lancet, 351(9115), 1560.
Rattan, S. (2000). Biogerontology: The next step. Annals of the New York Academy of Sciences, 908, 282–290.
Ritchie, H., Mathieu, E., Rodés-Guirao, L. et al. (2020). Coronavirus pandemic (COVID-19). Retrieved 28 October 2022, from https://ourworldindata.org/coronavirus
Santesmasses, D., Castro, J. P., Zenin, A. A., Shindyapina, A. V., Gerashchenko, M. V., et al. (2020). COVID-19 is an emergent disease of aging. Aging Cell, 19(10), e13230.
Selvarani, R., Mohammed, S., & Richardson, A. (2020). Effect of rapamycin on aging and age-related diseases-past and future. Geroscience, 43(3), 1135–1158. https://doi.org/10.1007/s11357-020-00274-1
Tam, B. T., Morais, J. A., & Santosa, S. (2020). Obesity and ageing: Two sides of the same coin. Obesity Review, 21(4), e12991. https://doi.org/10.1111/obr.12991
United Nations, Department of Economic and Social Affairs, Population Division. (2011). World population prospects: The 2010 revision, highlights and advance tables. Geneva, Switzerland: United Nations.
Wells, J. C. K., Nesse, R. M., Sear, R., et al. (2017). Evolutionary public health: Introducing the concept. The Lancet, 390(10093), 500–509. https://doi.org/10.1016/S0140-6736(17)30572-X
Williams, G. C. (1975). Pleiotropy, natural selection, and the evolution of senescence. Evolution, 11(4), 398–411.
World Health Organization,. 2006. Constitution Basic Documents, Forty-fifth edition, Supplement. Retrieved 28 October 2022, from https://www.who.int/governance/eb/who_constitution_en.pdf
World Health Organization. (2021a). The global health observatory. Retrieved 28 October 2022, from https://www.who.int/data/gho/data/indicators/indicator-details/GHO/life-expectancy-at-birth-(years)
World Health Organization. (2021b) Cardiovascular diseases. Retrieved 28 October 2022, from https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper was presented to the Political Studies Virtual Workshop at Queen’s University. I am grateful to the participants of that workshop for their feedback and questions, as well the helpful suggestions from reviewers for this journal. I want to express a special thanks to John Davis, who provided extensive and insightful feedback on the paper.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Farrelly, C. Aging, Equality and the Human Healthspan. HEC Forum (2022). https://doi.org/10.1007/s10730-022-09499-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s10730-022-09499-3