Abstract
This article explores solidarity as an ethical concept underpinning rules in the global health context. First, it considers the theoretical conceptualisation of the value and some specific duties it supports (ie: its expression in the broadest sense and its derivative action-guiding duties). Second, it considers the manifestation of solidarity in two international regulatory instruments. It concludes that, although solidarity is represented in these instruments, it is often incidental. This fact, their emphasis on other values and their internal weaknesses diminishes the action-guiding impact of the solidarity rules. The global health and human subject research scene needs a completely new instrument specifically directed at means by which solidarity can be achieved, and a reformed infrastructure dedicated to realising that value.
Similar content being viewed by others
Introduction
Scientific research and biotechnologicalFootnote 1 advances are expanding the breadth and scope of human activity. Nowhere is their impact more apparent than in the realm of human health, where they have contributed not only to new treatments, but also to new (and expanding) pressures/demands on healthcare systemsFootnote 2 ([77], at 329). The interaction between science/biotechnology and healthcare led Director-General of UNESCO, Federico Mayor, to suggest that efforts are needed to ensure that advances are solidly grounded on the essential values of mankind [72]. For purposes of this paper, “values” might be defined as deeply held ideas, or beliefs and moral concepts which contribute to personal and social identity. Of values, it has been stated that they:
… are often hidden. … [T]his may be because some values are so deeply held that they appear to require no articulation, the presumption is that they are commonly shared and acknowledged. Society … often lacks formal frameworks for discussing values. Political and regulatory frameworks have actively discouraged discussion of values, partly because they do not have the mechanisms by which to deal with them. Values and intrinsic ethical objections are often seen as ‘irrational’ and therefore discounted. … [17]
I have suggested elsewhere that legal regulation of biotechnological advances are appropriately evaluated with reference to the touchstone values of human dignity, sanctity of life, autonomy, justice, and, crucially, solidarity, which values should colour the nature, content and interpretation of regulation directed at healthcare generally and genetic research and treatment specifically. While much has been written about some of these values, this is less true of solidarity.
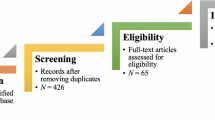
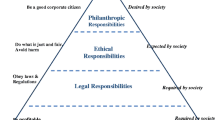
As such, this paper examines solidarity, not as an overarching moral or political theory, but as a moral/ethical value which ought to influence solutions to social/legal problems and which is supportive of derivative legal rules which can be used to evaluate legal and quasi-legal instruments; a means by which we can expand the basket of tools we use when approaching governance activities.Footnote 3 Part I briefly explores solidarity as a fundamental value, grounding its content/definition in claimed social beliefs and healthcare trends. Part II articulates some practical and concrete duties the value supports, using healthcare and, in particular, international human subject research (“HSR”) as the context. Part III assesses two international instruments—the Helsinki Declaration: Ethical Principles for Medial Research involving Human Subjects (2000) (“Helsinki Declaration”) and the CIOMS International Ethical Guidelines for Biomedical Research Involving Human Subjects (2002) (“CIOMS Guidelines”)—to identify whether and how the value finds expression in the international human research and healthcare context.
By examining the transition from theoretical value (Part I) and evaluative rules (Part II) to international directives (Part III), this paper offers some insights as to whether solidarity finds a policy voice commensurate with its theoretical ideal. In the absence of an adequate voice, it suggests a way forward for the better realisation of this important value.
Theoretical Solidarity: The Substance of (International) Solidarity in Social/Legal Regulation
As indicated above, this Part offers a definition of solidarity as a fundamental value and the context within which it should be applied, drawing on longstanding conceptions of moral human interaction and certain trends in the modern healthcare context.
Defining the value
At the outset, one must concede that the idea of solidarity has many roots, conceptions and potential manifestations. For example, it has long been a touchstone in religious norms of human interaction (which are often the first/formative norms that humans learn and the most important moral rules to which humans adhere). Religious traditions have expressed it as:
-
brotherhood, community, unity and interconnectedness,Footnote 4
-
mutual respect/love and reciprocity,Footnote 5 and
-
generous, loving and just action toward others.Footnote 6
In political discourse, solidarity is often viewed as a matter of individuals performing reciprocal duties and respecting reciprocal rights. This conception recognizes that individuals are grounded in communities and publics founded on shared identity (a sense of belonging, responsibility and moral commitment) and shared utility (a feeling of mutual dependence and shared self-interest in pursuit of opportunities and joint goals). The manifestation of political solidarity culminated in the Polish Solidarity Movement of the 1980s, which advocated democracy and social justice.
Despite its general familiarity to many people, therefore, its multidimensional history and varied use will make any attempt to arrive at a workable definition somewhat controversial. Rather than settle on a concise definition for the value, it may be more useful to articulate it as a series of interrelated and mutually enhancing propositions which draw on some of the existing expressions. I suggest that solidarity is captured by the following:
-
Proposition 1: Solidarity recognizes that individuals are naturally and irrevocably embedded in social contexts; they are in a state of interrelationship or interconnectedness with individuals, groups and society.Footnote 7 It therefore emphasises community.
-
Proposition 2: Solidarity is grounded in compassion, fraternity and a genuine interest in the well-being of others, the ultimate goal being to construct, through personal and collective actions, both a “just” and a “decent” or “fair” society. It therefore emphasises equality and the active promotion of welfare.
-
Proposition 3: Solidarity demands common action to uphold the complex of social relationships and values that is needed to realise useful standards of decency and justice. It therefore emphasises the role of duties flowing from and toward individuals and communities, and may require collective interests to take priority over the interest of individuals or sub-collectives.
Having settled on these propositions, one must delineate the “social context” within which to apply them.Footnote 8
Defining the context
Modern social contexts are more diverse, overlapping and conflicting than ever before (ie: family, neighbourhood, trade organisation, class, nation, continent, religion, gender) ([55, 56], at 336; [3], at 378; [53], at 207). One might argue that adoption of a broad social context risks ignoring cultural, linguistic, national and racial differences, resulting in connections/identities that are too loose/weak to found compelling duties. However, given existing economic demographics and converging legal practices, I believe that the only social context that will vindicate the value and redress the social inequalities that currently exemplify human existence is the global one.
The current global setting is characterised by widening economic disparities,Footnote 9 rapid population growth,Footnote 10 the emergence and spread of infectious diseases,Footnote 11 escalating environmental degradation (due to the expansion of human population and human activities),Footnote 12 and ubiquitous armed conflicts (with resultant social dislocation),Footnote 13 none of the consequences of which are limited to the groupings identified above. With respect to health, this is resulting in a human tragedy and an ever-growing disparity between the “haves” and the “have-nots.”Footnote 14 For example:
-
though basic health(care) is viewed as a fundamental human right,Footnote 15 the 90/10 disequilibrium on global medical expenditure continues, and thereby ensures that enjoyment of health is very much differentiated between regions;Footnote 16 [44, 86, 101]
-
the public-to-private and developing-to-developed country migration of healthcare workers persists, and thereby negatively impacts on equitable healthcare delivery [90];
-
a model of development and international aid that is shaped by donor-agendas and characterised by poor coordination, weak management and inappropriate means of measuring benefits persists, and thereby fails to redress the healthcare deficit; [82] and
-
private entities often fail to act in conformity with appropriate healthcare development practices, erecting high drug prices,Footnote 17 conducting under-scrutinised multi-jurisdictional trials which involve procurement of genetic samples, and plundering underdeveloped countries for biological sources, and thereby instrumentalises large groups of people ([1, 7, 28, 29, 79, 89, 92]; GRAIN).
Additionally, and ironically, this global health setting is exhibiting a marked and sharpening emphasis on the self, and not only by westerners familiar with rights-based language and ready to claim rights to health,Footnote 18 to reproduction, and to information, and to, conversely, informational and physical privacyFootnote 19 (as well as rights of/to privacy,Footnote 20 equality,Footnote 21 expression,Footnote 22 mobility,Footnote 23 freedom from arbitrary state interferenceFootnote 24). This trend has lead to an emphasis on the vindication of autonomy-based individual rights in ethical and legal analyses (e.g: as evidenced by the avalanche of writing on consent in medical treatment),Footnote 25 and a growing discomfort with the recognition, imposition and enforcement of duties (e.g: as demonstrated by our treatment of the environment,Footnote 26 and of fellow human beings in impoverished regions of the worldFootnote 27). In short, we (particularly in the west) are trading social context for individual freedom such that we are empowered and enabled, but isolated and disconnected; a trajectory that leads to an over-emphasis on consumption and inwardness with a corresponding alienation of the “other” [16, 76]. Such an emphasis makes it unlikely for the “haves” to seriously and effectively work toward the validation, empowerment and enhancement of the “have nots,” especially those who may live (and die) thousands of miles away.
The immorality of the existing global milieu (whether assessed from a utilitarian, human rights or other perspective), seems self evident. Patients, wherever located, are becoming more aware of the expanding scope of healthcare capabilities, and have a legitimate interest in access to reasonable healthcare so they can maintain reasonably active and fulfilling lives. However, despite the incontrovertible truth that pursuit of human goals is heavily contingent on the health of people, communities and the environment (i.e: nothing can be achieved without some reasonable level of health and fitness), they are unable to do so. There are no conditions under which we as moral agents can legitimately accept an expanding and fatal healthcare deficit for the global majority and a widely counter-productive emphasis on the importance of the individual as a self-motivated consumer of health and other resources extracted from around the world and with consequences for all parts of the world. Their continued existence suggests both that:
-
1.
our dominant ethical approaches to (health) problem-solving have obvious blind spots; and
-
2.
health solidarity, as an ethical value, must become a more integral aspect of these approaches, driving them toward responses that adopt a broad, community perspective and have a global reach.Footnote 28
A global reach is all the more important given the rise of predictive medicine (involving genetic research and clinical genetics), which is driven by private global operators, thereby suggesting a need for regulatory responses which are similarly global.
Summary/conclusion
Solidarity, with its emphasis on the social context within which we live and our shared duties toward one another, encourages us to become “global citizens”; to be cognizant of and contribute to the global community to which we all belong and upon which we all rely. As defined above, solidarity is a moral vehicle for injecting legitimate concepts and considerations of community and interconnectedness into ethical and legal analyses. If the potential benefits of solidarity are to be realised (eg: redressing some of the shortcomings of the existing healthcare deficit), solidarity must be ranked equally with other popularly claimed and largely complimentary moral values such as sanctity of life and human dignity.
Practical Solidarity: The Translation of (International) Solidarity Into Rules for Human Subject Research
If the solidarity value is to be realised, one must look beyond defining it and the social context to which it applies, and explore the types of actions which promote and flow from its realisation:
What counts primarily is not an awareness of social association, but the actual practice of keeping associations intact and reforming associations in such a way that social ties may be upheld in a redefined way. This perspective [is] on action instead of merely values … . What counts is … the maintenance of a certain quality of social relationships [95].
In short, one must articulate the quality of membership in society that is demanded by solidarity (regardless of the particular ethical theory to which one subscribes). As such, this Part offers some specific duties derived from the solidarity value which are applicable to the international healthcare and HSR context. In many ways, this is an imaginative exercise, the purpose being to determine the action that solidarity reasonably imposes (or could or should impose) on us as members of the global community toward others within that community. The duties articulated below are aimed at the realisation of a “decent” global society in which everyone’s health is supported such that they can effectively participate in life. They address obligations to contribute to the common effort to protect life and equity in society, and they are not exhaustive. More could be added if one were to incorporate all health determinants (i.e: education, nutrition, water, sanitation, communication infrastructure), but they are beyond the scope of the analysis, which now narrows to the promotion of global health through the advancement of biotechnology through HSR.
Duty to research
Propositions 1 and 2 above clearly suggest a duty to pursue scientific-medical knowledge for the “betterment of humanity” (ie: research directed toward preventing serious harm or providing significant benefits to humankind).Footnote 29 Given existing social and research structures, this duty settles on individual researchers, private entities and states.
With respect to public bodies, the realisation of this duty necessitates the strategic use of public research funds and the clear expression of research priorities to and from funding bodies. For example, public funds could be used for “frontier research” (i.e: early stage or basic research which is amenable to multiple applications and could lead to unforeseen breakthroughs), and “gap research” (ie: projects which attempt to address diseases/conditions which are not as commercially lucrative and are therefore less likely to be tackled by private entities).
With respect to academic bodies and private entities, it suggests a similar responsibility to prepare morally defensible expressions of biotechnological/medical research priorities. Where notions of solidarity are steering health research, one would expect the research to be directed at conditions/diseases that are both widespread and, additionally, more narrowly experienced (and therefore not necessarily profitable to cure). Indeed, this would seem imperative given current concerns that market priorities are driving research and resulting in the value of research being measured by commercialisable results [88].
Duty to capacity-build
Given the stark and inequitable realities of the health deficit, and its dire consequences on individuals and populations, and given the wide disparities between the developed and the developing world with respect to the existence and application of ethical laws, regulations and guidelines and the existence of quality ethical review, a “duty to capacity-build” is of vital importance [69]. Such a duty is supported by Proposition 3 above, which, in practice, requires more enabled states and research bodies to enter into collaborations with less enabled states/bodies. Such activities would enhance the capability of “have nots” to identify local health priorities, to ethically review research proposals, to create opportunities for domestic researchers, and to avoid unfair research practices.Footnote 30 Importantly, capacity building must not only form an ongoing part of (ethical) multi-jurisdictional research, it must precede research:
Parties affected by proposed health research projects need to become increasingly involved in designing and carrying out the research. … There is … broader recognition of the need and value of consulting local communities and involving potential participants in research early on in the process of designing research protocols [62].
Pre-commencement collaboration and capacity-building is particularly important where host countries have set national health priorities, are endeavouring to ensure that research responds to societal needs, and are trying to weigh the benefits/risks to both participants and communities.
Duty to share
The solidarity value, by virtue of each of the above Propositions, supports a duty to disseminate and share biomedical knowledge and advances [85]. This is vital if exploitation is to be curtailed and the existing health deficit rectified. This duty imposes a responsibility on individual researchers, private entities and states to erect mechanisms for knowledge- and benefit-sharing (which includes making medical products available according to principles of fairness and decencyFootnote 31). Only by doing so can individuals enjoy their right to share in or enjoy the outcomes of scientific advancement, a universal right already enunciated in existing international human rights instruments,Footnote 32 and by the HUGO Statement on Benefit Sharing [57], which recommends that profit-making companies dedicate a percentage of their profits to healthcare infrastructure and/or humanitarian efforts. On a practical level, in the HSR context, one might expect governing/guiding instruments to directly and concisely address matters of (1) the standard of care of treatment to individual research subjects, (2) benefits for host populations, and (3) ongoing treatment for research subjects.
Duty to account
The solidarity value’s emphasis on community and the construction of a just and fair society implicates a duty to account. That is the duty—of individual researchers, private entities and states—to report fully, honestly and regularly, on the performance of those tasks they have been given, to their stakeholders and the wider public so that their conformity to stakeholder/public interests and concerns can be monitored/measured ([65], at 515Footnote 33). Because failures also contribute to scientific knowledge and from failures one can find avenues to success, this includes reporting adverse results of ethical research, although it may not necessitate reporting adverse results from exploratory pilot studies aimed at generating hypotheses rather than proving them [54]. On a practical level, it requires legal instruments to clearly delineate and apportion oversight responsibilities and disclosure/dissemination responsibilities as between researchers and sponsors (whether private or public) so that accountability can be realised (and may demand the erection of variable standards and modes of disclosure/dissemination so as to ensure effective accountability in jurisdictions with low-capacity or inexpert institutions).
Duty to participate
It has been suggested that:
… the fundamental reason why contemporary medical ethics has so little to say about public health is that its focus on individual autonomy suggests that all compulsion for the sake of health is wrong. … Thinking at the level of populations or groups requires a vetting of current ethical and legal principles and the development of a concept of the public good or of “common” goods [61].
An over-emphasis on autonomy-based individual rights causes problems for effective healthcare research, not only domestically, but internationally [36]. For example, strict compliance with western articulations of individual rights in countries where such rights are not similarly valued or defined could lead to misunderstandings and the abandonment of research that could benefit the host country. Similarly, strict compliance with such rights could impose onerous and expensive administrative requirements that cannot be met by researchers or participants in countries with diminished/developing capacity for research, and thereby hinder research.
The solidarity propositions reasonably impose a duty on individuals to contribute to the search for knowledge that will be used for the good of themselves and others (eg: to participate in HSR). This duty has been defended as follows:
[T]here is clearly sometimes an obligation to make sacrifices for the community, or [for] an entitlement of the community to go so far as to deny autonomy and even violate bodily integrity in the public interest … . [W]e accept substantial degrees of compulsion or coercion in the interest of those coerced and in the public interest. Numerous examples can be given: limiting access to dangerous or addictive drugs or substances; … vaccination as a requirement … ; screening or diagnostic tests for pregnant mothers or for newborns; genetic profiling for those suspected of crimes; quarantine for some serious communicable diseases ; … ; detention under mental health acts … . All of these [and others of a non-health nature, including jury duty, taxation, voting] involve some denial of autonomy [and] some imposition of public standards … [52]
In short, so long as our own health is not unreasonably threatened and safeguards are in place to ensure respect of certain of our rights (eg: provision of information, anonymity of data, etc.), there is a strong argument for individuals having a moral obligation to take part in research where that research will further knowledge and help people in need, presently and in the future, locally and around the world [23, 66]. Parenthetically, it is important to note here that the solidarity value does not abhor individual rights or enlightened self-interest. Rather, it recognises that individual freedom is contingent upon cooperative action toward others so they too can enjoy freedom; acts of solidarity are a means by which we empower others to pursue and by which others empower us to pursue our interests (the emphasis being on common interests which further the common good) and by which we realise our rights.
The most obvious consequence of this moral imperative to take part in research is that participation might be compelled without informed consent.Footnote 34 The subject’s human rights are not so much trumped by society’s interests as balanced against comparable rights of other people within the shared social context:
[T]he contrast is not between vulnerable individuals … and an abstract entity such as ‘society’ … but rather between two different groups of vulnerable individuals. The rights and interests of research subjects are surely not served by privileging them at the expense of the rights and interests of those who will benefit from research. Both these groups are potentially vulnerable, neither is obviously prima facie more vulnerable or deserving of special protection [52].
In articulating and promoting this duty, instruments would have to enumerate the purposes for which and the circumstances under which people (individuals and communities) are appropriately compelled to participate in research. Given the existing rights-based paradigm, the prominence of individual rights in international and domestic instruments, and the indisputable good that stems from healthy levels of individual freedom, these circumstances would, presumably, be circumscribed. But their recognition and delineation are important if solidarity is to be realised in a practical sense.
Summary/conclusion
If solidarity is to be transformed from a purely rhetorical device into a practical device, it must be translated into social and political actions capable of recognition and enforcement in legal instruments.Footnote 35 The duties discussed above, though perhaps controversial, emerge from the solidarity propositions offered in Part I, and are all clearly capable of legislative enactment, or inclusion in international legal and policy instruments. Further, and importantly, being characterised as duties rather than rights, they are readily assignable and amenable to measurement (for compliance).
Existing Solidarity: The Articulation of (International) Solidarity in Human Subject Research
One must acknowledge that the autonomy value (and the individualist perspective) is dominant in both the Helsinki DeclarationFootnote 36 and the CIOMS Guidelines,Footnote 37 their core objective being to protect research subjects from the dangers of participating in research [5]. This is understandable given their genesis out of wartime medical research atrocities, and their evolution during a time when there was a perceived need to bolster the position of the individual. Given their tenor, one might question the choice of examining them for evidence of solidarity. However, I defend the choice on the following grounds:
-
Although not legally binding (and with no enforcement mechanisms or sanctions for non-compliance), they are widely relied on in the biomedical research field around the world, often cited as the cornerstones of HSR [12].Footnote 38 The Helsinki Declaration in particular has been described as the most influential international instrument on ethical oversight of HSR, portions of it having been incorporated into international guidelines, domestic regulations and human rights related instruments, and informing the research protocols of various private entities [20, 25, 30, 34, 58].
-
They are directed at the health deficit in that their emphasis is multinational research and, in the case of the CIOMS Guidelines, protection of research subjects/communities/ populations from the developing world.
-
They were authored by broadly representative non-governmental organizations and were both recently revised.Footnote 39
Ultimately, in the absence of any similarly respected international instruments founded on solidarity, the value must (currently) be sussed out of and vindicated through instruments like these. As such, this Part explores whether and to what extent these instruments recognise/promote solidarity in the HSR context. It does this by examining the position of the above solidarity related duties within them (i.e: their presence, their clarity, and the extent to which they conform to the “ideals” suggested above).
Duty to research
The “duty to research” is addressed obliquely in Article 6 of the Helsinki Declaration, which states that proven prophylactic, diagnostic and therapeutic methods must be challenged and improved through research. A number of other provisions address not so much the “duty to research,” but the need for sound scientific methods: Article 2 makes it a duty of all physicians to promote and safeguard “the health of the people”; Article 12 recommends caution with respect to research which might affect the environment or the welfare of animals. CIOMS Guideline 1 states that research must have “the prospect of discovering new ways of benefiting people’s health.” One might argue that this restricts opportunities for frontier science, but it is not difficult to find some health-benefiting hook to most well-planned research, and, given that the subject matter is HSR and experimentation, certain welfare-related limitations are reasonable. One can see that the “duty to research” finds only limited overt recognition in these instruments, the duty presumably being assumed. With respect to its more specific articulation, neither instrument goes so far as to emphasise or differentiate the specific duties of the specific actors as outlined above.
Duty to capacity build
The “duty to capacity build” is not specifically addressed in the Helsinki Declaration, but CIOMS Guideline 20 enumerates several measures directed at enhancing ethical review and administrative expertise in developing world locales, including:
-
strengthening review capacity by establishing competent independent review bodies;
-
strengthening research capacity by training research and healthcare staff;
-
developing technologies appropriate to healthcare and biomedical research; and
-
educating the community from which subjects are drawn.
However, the CIOMS Guidelines do not specifically outline the ethical procedural characteristics of developed-developing world partnerships (e.g: timing of capacity building activities, allocation of research roles, infrastructure investments, authorship credits, measures of capacity building among local researchers, health services and communities), which would seem essential if emerging jurisdictions are to enjoy some consistency of experience on which they can build their own expertise [96].
Duty to share
Standard of care
Article 29 of the Helsinki Declaration states that the benefits, risks, burdens and effectiveness of new methods should be tested against those of the best available method, and that placebos should only be used where no proven method exists. CIOMS Guideline 11 states that control groups should receive established and effective interventions and should only receive placebos where no effective intervention exists. The solidarity enhancing quality of these provisions is obvious—their intention being to get some reasonable level of treatment to participants.
However, difficult issues remain unresolved, such as the meaning of “standard of care” in the HSR context. Does it refer to what would constitute a best or ideal practice given the state of international medical knowledge? Or does it refer to the existing standard practice in response to that condition in the sponsoring country (often western), or the host country (which may have no standard because no treatment exists there), or is it some international standard (which might involve local/host experts determining the best maintainable diagnostic and therapeutic practices to be met given their circumstances)? This uncertainty diminishes the proscriptive value of these instruments. Indeed, an absence of precision has triggered controversy, with commentators (1) pointing to various (beneficial) projects which would not have proceeded had these provisions been interpreted so as to force provision of expensive western care in developing communities with little infrastructure to support or maintain it, and (2) lamenting the possible stymieing effect on research if it is so interpreted in future [12, 14, 49, 69, 87]. A solution which serves to reify the solidarity value probably lies in the “international standard” approach, which is more contextual in that it:
… rejects the “bad, if not perfidious” local de facto standard while still permitting research to go forward that may not meet the stringent requirements of the global de jure standard. [It] would not permit researchers knowingly to deny subjects care that has proven effective for their illness in their population, and thus ensures that subjects … are not exploited. At the same time, [it] requires attention to substantive differences. In social, cultural and economic contexts and their impact on the permissibility of international research ([69], at 30).
In any event, it is clear that the provisions have the solidarity-promoting intention of ensuring some positive benefit to participants, but has no way of promoting much less ensuring any sort of consistent standard.
Benefits to host populations
Article 19 of the Helsinki Declaration states that research is only justified where there is a reasonable likelihood that the populations in which the research is being carried out stand to benefit from the results of the research. Similarly, CIOMS Guideline 10 stipulates that every effort must be taken to ensure that research is responsive to the health needs and priorities of the community/population of the host country and that the knowledge/intervention/product developed will be made reasonably available for the benefit of that population. Disappointingly, the instruments are not clear as to what constitutes “reasonable likelihood” of benefit, or what constitutes benefits being “reasonably available” (ie: what factors are relevant and how many are needed to tip the balance). This vagueness obviously has implications for the action-directing capabilities of these instruments.
Further vagueness-related concerns arise when looking at the instruments through the solidarity lens. For example, Article 19 of the Helsinki Declaration could be interpreted to limit participation in research to those who will benefit directly from the research (ie: to those who suffer from the condition investigated). Such an interpretation is bolstered by the overarching tone of the instrument and by Articles 5, 19, 24, 28 and 29, all of which suggest that the research must be in the direct interest of the subject him/herself.Footnote 40 Surely it is inappropriate to challenge the ethicality of research not directly beneficial to the participant(s) in experimental settings where consent has been obtained; such a challenge is offensive to solidarity in that it fails to acknowledge the duties to research and to participate. Alternatively, Article 19 could be interpreted as requiring researchers to ensure that the populations in which the research is undertaken (not necessarily limited to the participants per se) incur some identifiable benefit as a result of the research. On this point, it has been suggested that Article 19:
… supports the position that to avoid exploitation, the research question and results should have relevance to and potential benefit for the population from which participants are drawn. However, it seems overly narrow and unjustifiable to restrict the notion of benefit to populations participating in research to benefits derived from the results of the research. A broader notion of benefits to the populations would recognise that benefits from the conduct of research (such as capacity development) and not restrict them to those linked solely with results [39].
For purposes of realising solidarity, it is appropriate that subject communities/populations share in the benefits of the research. Whether that requires broad/diluted benefits such as dissemination of information/knowledge to subjects and capacity building in local communities, or narrow/direct benefits such as access to research outcomes (e.g: new treatments or products if any are developed) by participants and/or their community, is open to debate [12]. For present purposes, the key is that the “duty to share” is clearly implicated, if not clearly articulated.
Continuation of treatment
The idea that subjects (and communities) should continue to receive treatments on which they may have become dependent clearly implicates the “duty to share” by recognising that in “have not” communities, participation in trials is sometimes the only way to access new treatments (or any formal healthcare at all) [5] making the subsequent abandonment of subjects where some reasonable treatment has been developed or otherwise exists, morally questionable.
Article 30 of the Helsinki Declaration, and its Explanatory Note, stipulate that, at the conclusion of studies incorporating medical care, subjects should retain the best proven care identified by the study. Similarly, CIOMS Guideline 21, which bolsters Guideline 10, stipulates that healthcare services should be provided throughout the course of the research and, where interventions or products are developed, they should be made “reasonably available” to the community/population concerned post-study. These provisions have generated vociferous debate,Footnote 41 stakeholders arguing that the concomitant added research preparation and expense could dissuade certain research [54, 58, 69]. Similarly, it has been argued that:
This debate needs to be resolved in a manner that does not preclude further development of health systems through targeted research. It should permit pragmatic improvement rather than waiting for revolutionary changes in health systems that may never happen. The development of low cost alternative interventions is only possible through such a process [13].
Obviously, caution must be exercised in responding to complaints about added expenses because of the parochial interests which may be driving them.
For purposes of the present exercise, one can say that both instruments are supportive of the solidarity-justified duty to continue treatment at least for research subjects beyond the conclusion of the protocol where the known circumstances of the subject warrant it (although they pursue this in slightly different ways). Unfortunately, the provisions have met strong industry resistance, and the frailties of these instruments (eg: their non-enforceability) is here starkly exposed.
Duty to account
The Helsinki Declaration includes a host of “duty to account” provisions, many of them added in the most recent revision (and mostly as a means of protecting the individual). Articles 13, 14, 16 and 22 state that, where human subjects are anticipated, research protocols should:
-
be preceded by careful risk/benefit analysis (with respect to both subject and society);
-
contain information about funding/sponsors, affiliations and potential conflicts;
-
contain a statement of ethical considerations;
-
contain a statement of compliance with ethical principles;
-
be reviewed by ethical committees independent of the investigator and the sponsor;
-
be monitored on an ongoing basis and particularly in the case of an adverse event.
Article 27 also implicates accountability in its stipulation that funding sources, institutional affiliations, possible conflicts of interest, and results must be accurately reported and publicly disseminated.
Similar directions are contained in CIOMS Guideline 2, the Commentary for which specifically envisions possible reference to international review committees. Guideline 3 is directed at protecting the vulnerable by requiring ethical review in both sponsor country and host country. It tries to ensure that the most stringent and effective standards are applied, that there will be some capacity building in the host country, and that the research is responsive to the health needs of the host population [27]. Guideline 18 imposes the responsibility of establishing confidentiality safeguards and reporting the limits of same to subjects.
Clearly both instruments are mindful of the concept of stringent accountability, and to that extent promote solidarity. The Helsinki Declaration’s provisions in particular represent an improvement over previous versions; however, it fails to specifically recognize and address the ethical oversight and accountability duties of the host country [96]. The CIOMS Guidelines’ dual review procedure avoids this weakness, but fails to identify the appropriate course when opposite outcomes on ethicality are arrived at by host and sponsor country institutions. This lack of clarity has led to debates over the danger of imposing inappropriate western principles on culturally distinct communities in developing countries, on the one hand, and the immorality of conducting research in developing countries just because it is cheaper and laws are more lax, on the other handFootnote 42 [80].
Duty to participate
Given its historical backdrop, it is unsurprising that the Helsinki Declaration does not endorse the “duty to participate.” Rather, it seeks to promote participation through individual participant protections. For example, Article 5 stipulates that the well-being of the subject takes precedence over the interests of science and society, and Article 8 states that research must promote respect for all humans and protect their health and rights. Curiously, however, Article 8 characterises subjects who will not personally benefit from research as “vulnerable” and in need of “special protection,” thereby capturing those who are otherwise of sound mind and body (and suggesting that everyone is vulnerable and in need of special protection). Article 24 bars participation of incompetents except in very limited cases where the health of the population they represent (those with a similar condition?) is benefited and no competent subjects are available. Article 17 restricts research to that where the risks are assessed and managed, which could arguably bar pilot studies and phase I studies (which naturally entail unpredictable risks).
Although the “duty to participate” is equally absent from the CIOMS Guidelines, they arguably adopt a more balanced approach to participation promotion. Guideline 8 states, inter alia, that where no benefit is expected to the subject, the risk must be reasonable in comparison to the benefit to society, thus explicitly endorsing the possibility of exposing (healthy) individuals to risk for society. Guideline 12 highlights the need to choose research subjects with a view to the equitable distribution of benefits and burdens.Footnote 43 Guideline 13 and its Commentary offers more explicit action-guidance by specifying groups that are considered vulnerable and deserving of special protection, being those who are incapable of protecting their interests because they have insufficient power, intelligence, education, resources, strength or other needed attributes (ie: children, the mentally handicapped, subordinate members of a hierarchy, the poor, the aged, etc.).Footnote 44
The Helsinki Declaration’s over-expansiveness, which stems from its lack of clarity, is contrary to the solidarity value and may actually hinder research [39], because it erects hurdles to the recruitment of participants and creates an atmosphere of “selfism” not particularly conducive to research participation. The CIOMS Guidelines, though falling well short of endorsing research participation as a duty which we all have toward humankind and the society in which we live, offers better guidance which is directed at making participation safer and, by implication, more desirable.
Summary/conclusion
Although they are obviously founded on other values, particularly autonomy, both the Helsinki Declaration and the CIOMS Guidelines contain solidarity notions (i.e: highlight the need for reciprocity, equity and accountability), which, if pursued systematically within the arena addressed, might enhance global health and healthcare equity, the ultimate goal being the realisation of a more just, fair and decent global society. However, the strongest measures for situating the person within the social context are absent. Given our consistent and continued failure to protect and equitably utilize resources from the global commons, from plants to people, the absence of more instructive and complimentary expressions (i.e: the same duties in the same language) of the duties is disappointing. Indeed, their separate revisions, which occurred very close to one another, represent a real collaborative opportunity lost. A more cooperative approach to reforming the global HSR arena might have entailed the following:
-
revocation of the “complex and often conflicting” [81] matrix of declaratory instruments in the HSR field, and collaboration between the WHO, UNESCO, WMA, CIOMS, and ICH, in drafting a single, overtly prescriptive, ethical instrument for use by all stakeholders which (1) contained concise rules and complete supportive commentaries, (2) emphasised the duties outlined above and articulated how they could be achieved by the various stakeholders, (3) offered factors for measuring compliance and success, and (4) suggested consequences for non-compliance;
-
establishment of a single international auditor of all developing country HSR conducted by external sponsors so that systematic monitoring of research expenditure could be undertaken on an ongoing basis (which would allow for long term tracking and broad performance/outcome evaluations); and
-
formation, education and funding of accountable and independent ethics committees in every developing country through a single program sponsored by the international community, including the WHO, UNDP, SIDCER, and the World Bank, which committees would be specifically capable of addressing the special issues which arise in developed-developing country research partnerships (ie: relevance to host healthcare priorities, scientific validity, international ethical acceptability, etc.).
Such an approach to the process of governance (as compared to the substance of the guidance) promotes solidarity in a number of respects. It models international cooperation and democracy, it capacity-builds in those who participate, and it brings an important field more in line with justice by rationalising and streamlining what is currently complex and disjointed. In addition to supporting solidarity, such an endeavour would offer policy-makers the opportunity to more explicitly include solidarity duties in the substantive provisions of the new instrument.
Conclusion
Over time, the conceptual framework structuring the delivery of personal healthcare has evolved from one characterised by paternalism to one of partnership (between physician and patient). A similar evolution has not been experienced in public healthcare, and certainly not at the global level; great swathes of people are treated paternalistically and disadvantageously with respect to access to knowledge, resources, and services. The causes of this uneven evolution are numerous and include the structure of the global market and its transfer of healthcare influence to profit-driven entities with self-serving agendas and paternalistic attitudes toward development, and the emphasis on the individual patient (and what s/he can secure for self) in “have” regions around the global. The result is that real advances for patients are unevenly enjoyed around the globe. It is past time to shift from this paradigm (which is not working) to one of global citizenship.
This paper explored a conceptual/ethical vehicle for pursuing that shift—the solidarity value. Greater attention to it and some of its derivative duties (eg: to research, to capacity-build, to share, to account, and to participate) in legal instruments and ethical assessments of domestic and international healthcare activities could lead to the adoption of conduct that could realise the benefits promised by the value, namely a fairer, just and descent society where people are not “left behind” on the basis of geography; a society that acknowledges and embraces its obvious and intimate global linkages. This paper also assessed two international instruments, using the solidarity duties as the evaluative criteria. Although some notions of solidarity are clearly present, they fall short of the ideal and have no chance of realising the paradigm shift called for here and elsewhere.Footnote 45 Indeed, that stakeholders cannot even agree on whether these instruments are “prescriptive” (stating ideals that ought to be met so as to ensure the highest standards), or “descriptive” (merely reflective of existing best practices to which most researchers adhere), makes the chances of them being used in any uniform way remote; they will continue to be used as researchers see fit.
Many of the characteristics of our converging global community reflect the truth of the sentiment contained in Donne’s [35] famous words:
No man is an island, entire of itself; Every man is a piece of the continent, a part of the main. If a clod be washed away by the sea, Europe be the less
…
Any man’s death diminishes me because I am involved in mankind. And therefore, never send to know for whom the bell tolls; It tolls for thee.
In short, humans, collectively considered a class deserving of special respect and generally sharing a desire to be healthy, are irrevocably intertwined. We are comparably susceptible to disease, which creates needs in sufferers, families, carers and the community that are common around the world (i.e: resources, basic treatment, emotional support, etc.).Footnote 46 We all experience and perpetuate the global health deficit in some way, and events in faraway regions can impact directly on our health, well-being and general conduct.Footnote 47 We all benefit to wildly varying degrees from living in a society which pursues research; the very knowledge that research is being undertaken on conditions that we have or may eventually suffer from is a thread that ties all people together [52]. In short, we are not islands onto ourselves, but pieces of the whole, and we must strive to better act as though others’ deaths diminish us as a collective. Unfortunately, there is a disconnect between the ideals expressed in our most aspirational (and recent) declarations on human and social rights (and in poetic sentiments like Donne’s) and the instruments which more directly govern our actions (like the Helsinki Declaration and the CIOMS Guidelines). To shift the paradigm, we must redress this disconnect, and establish institutions with the ability to enforce conduct which is globally utilitarian and therefore better capable of actively enhancing the health and human dignity of everyone. In the HSR context, we might start by drawing more heavily on the solidarity value.
Notes
Biotechnology is here used to denote the application of new and emerging technologies to the study of living organisms or that uses living organisms or derivatives thereof to produce or modify (health) products and services. See the definition in the Convention on Biological Diversity (1992), signed by 168 states, as well as those at www.mayominnesotapartnership.org/glossary.htm and www.uni-hohenheim.de/biotech/eng/def_biotech.htm.
Attempts to define these and other values and to measure the propriety of tomorrow’s biotechnologies have been undertaken within the rubric of various moral approaches, including principlism, virtuism, feminism, etc. For the purposes of this paper, no particular “approach” or overarching “theory” of rights or morality is espoused.
In African traditionalism, note the maxim simunye (we are one; unity strength). In Buddhism, Hinduism and Christianity, note concepts of brotherhood and interconnectedness. In Judaism, note clal yisrael (unity despite differences) and brit (the covenant which binds Jews to one another and to God, and the fostering of reut or “neighbourliness”). In Islam, note tawhid (unity and oneness of humanity).
In African traditionalism, note the widely held maxim, umuntu ngumuntu ngabantu (to be human is to affirm one’s humanity by recognizing the humanity of others). In Buddhism, note the admonition against excess. In Confucianism, note the emphasis on love of life and mutual respect. In Hinduism and Christianity, note concepts of reciprocity. In Judaism, note arevut (mutual obligation). In Islam, note hubb (love), rahma (mercy/compassion).
In some African traditions, note shosholoza (working as a team; group spirit in adversity) and the shared responsibility of dialogue and cooperative action. In some Asia traditions, note kalayanamitra (friends helping friends). In Buddhism, note concepts of enduring sacrifice in others’ interests. In Confucianism, note concepts of duties and action toward others. In Hinduism, note da da da (give and be merciful) and concepts of obligation to others. In Judaism, note kiruv (reaching out, partnering with humanity) and tzedaka (duties to help the poor). In Christianity, note John 15:13 (self-sacrifice) and Mark 10:21, Luke 6:20 and John 3:17 (mutual assistance, often in relation to the poor). In Islam, note zakat (obligation to give to the poor), sadaqah (charity/altruism), and concepts of ‘adl (justice) and wast (equilibrium) which underpin principles condemning exploitation and the isolation of oneself from the rest of humanity.
J. Habermas [47] Zur Bestimmung der Moral (Frankfurt: Suhrkamp, 1986), uses the term “intersubjectivity.”
Only by situating the individual within society can we determine whether we have obligations toward one another as citizens of a community [60].
The income of the richest 20% of humanity is 80x that of the poorest 20%, and more than 2 billion people live on less than US$2 per day ([9], at 112). See also UNDP, Human Development Report 1999 (Geneva: [101], at http://hdr.undp.org/reports/global/1999/en/, and R. Falk, Predatory Globalization: A Critique (Cambridge: Polity Press, 1999).
Global population has risen from 4,452,645,562 (1980), to 5,282,765,827 (1990), to 6,081,527,896 (2000), to 6,460,560,374 (2005): see www.census.gov/ipc/www/worldpop.html (Aug. 16/05). It is expected to rise to 9.1 billion by 2050: see www.overpopulation.org/faq.html (Aug. 16/05).
Communicable diseases, which do not respect borders, continue to be the leading loss of human life: L. Garrett, The Coming Plague: Newly Emerging Diseases in a World Out of Balance (NY: Farrar, Strauss & Giroux, 1994). Contemporary examples of the mobility of infectious diseases are the SARS outbreak of 2003 and the more recent Avian Influenza pandemic; in a short time, it spread through multiple countries, resulting in tens of thousands of bird deaths and 63 human deaths: www.who.int/csr/disease/ avianinfluenze/country/case_table_2005_11_07/index.html (Nov. 8/05). For more on this, see www.fao.org/ ag/againfo/subjects/en/health/diseases-cards/special_avian.html, and http://europa/eu/int/comm/food/animal/ diseases/controlmeasures/avian/index_en.htm.
Whereas the global population increases by approximately 3,000 every 20 min (+/−), one or more species of animal or plant life becomes extinct (some 27,000 species per year): www.overpopulation.org/faq.html (Aug. 16/05). Freshwater consumption has increased 6× in the last 100 years; 5 million people die annually from diarrhoea due to polluted water; 20% of the world’s freshwater fish have disappeared or are endangered; some 63% of all species have been lost in the last 100 years and extinctions are occurring at increased rates; some 80% of forests have been cut worldwide and 40% of the remainder are threatened [84]. Extinction rates are estimated at between 1,000 and 10,000 times greater than they would be naturally [93]. Some 40% of the world’s forests are threatened by mining, and 25% of the world’s mammals and 11% of the world’s birds are at risk of extinction due to population growth and loss of habitat: Population Connection, at www.populationconnection.org/factoids/ (Aug. 16/05).
Health and security are linked [102]. Increasingly vicious, ethnic-based wars in poor nations cause massive human suffering, social disruption, population displacement and loss of natural resources [26]. Some 90% of modern war victims are civilians, mostly women and children: Population Connection, at www.populationconnection.org/factoids/ (Aug. 16/05).
Life expectancy by region has been reported as follows: Africa—46 (M), 48 (F); Americas—71 (M), 77 (F); South-East Asia—61 (M), 64 (F); Europe—68 (M), 77 (F); Eastern Mediterranean—61 (M), 64 (F); Western Pacific—70 (M), 74 (F). The countries with the lowest life expectancy rates and healthy life expectancy rates are African. Compared to life expectancy in the UK of 76 (M) and 81 (F), life expectancy rates in Lesotho are 35 (M) and 40 (F), Swaziland are 33 (M) and 36 (F), and Zimbabwe are 37 (M) and 36 (F). ([103], at 13).
See Article 12 of the International Covenant on Economic, Social and Cultural Rights (1966). Also see the Jakarta Declaration on Health Promotion into the 21 Century (1997), the People’s Health Charter (2000), and J. Mann et al. (eds.), Health and Human Rights (NY: Routledge, 1999).
Of 1,223 new drugs developed between 1975 and 1997, only 11 were for the treatment of tropical diseases, which are some of the largest killers [94]. In 1993, cancer research spending in the UK alone was US$200 million, whereas malaria research spending was US$84 million worldwide ([80], at 23). Over 40 million people, mostly in resource-poor developing countries, have HIV/AIDS, and even those few that benefit from drug trials receive very little follow up treatment post-trial [6, 59).
The commodification of the intellectual property regime has permitted the pharmaceutical industry pursue artificial improvements (rather than truly new products) while keeping prices elevated. [24].
See Preamble, WHO Constitution (1948). Every country in the world is a party to at least one treaty addressing health-related rights, including the right to health: see www.who.int/hhr/en/ (Aug. 26/05).
For an example such claims in a legal instrument, see the Convention on Biomedicine (1997).
Internationally, see Article 12 (privacy, family, home, correspondence) of the Universal Declaration of Human Rights (1948), and Article 17 (privacy, family, home, correspondence) of the International Covenant on Civil and Political Rights (1966). Regionally, see Article 8 (privacy, family, home, correspondence) of the European Convention for the Protection of Human Rights and Fundamental Freedoms (1950). In the UK, see Article 8 (privacy, family, home, correspondence), Part I of Schedule 1 of the Human Rights Act 1998 (UK) 1998, c. 42.
See Articles 2 (entitlement to rights without distinction) and 7 (no discrimination) of the UDHR (1948), Articles 2 (no distinctions on named grounds), 3 (equality of men and women), 26 (no discrimination) and 27 (minority rights) of the ICCPR (1966), Article 14 (no discrimination) of the ECHR (1950), and Article 14 (no discrimination), Part I of Schedule 1 of the HRA 1998.
See Articles 18 (thought, conscience, religion) and 19 (opinion, expression) of the UDHR (1948), Articles 18 (thought, conscience, religion) and 19 (opinion) of ICCPR (1966), Articles 9 (thought, conscience, religion) and 10 (expression) of the ECHR (1950), and Articles 9 (thought, conscience, religion) and 10 (expression), Part I of Schedule 1 of the HRA 1998.
See Articles 13 (movement) and 14 (asylum) of the UDHR (1948), Article 12 (movement) of the ICCPR (1966), Articles 2 (movement) and 3 (no expulsion) of Protocol 4 (1963) of the ECHR (1950).
See Articles 3 (life, liberty, security of the person), 8 (arrest, detention, exile), 10 (fair public hearing) of the UDHR (1948), Articles 6 (right to life) and 9 (liberty, security, fair trial) of the ICCPR (1966), Articles 5 (liberty, security) and 6 (fair trial) of the ECHR (1950), and Articles 5 (liberty, security) and 6 (fair trial), Part I of Schedule 1 of the HRA 1998.
See Chadwick and Berg [23], Callahan [18], Benatar [10], and others, who suggest that non-autonomy interests, when considered at all, are used to lead straight back to autonomy and individualism. Indeed, it has been claimed that autonomy is the primary if not the only interest worthy of protection [43].
In 1998, the USA, with approximately 4% of the world’s population, generated some 22% of the world’s green-house-effect causing CO2 emissions: Your Planet Earth (2000), at www.yourplanetearth.org (Aug. 17/05).
From 1982–1990, southern countries received US$927 million in aid, grants, trade credits, direct private investment and loans, but paid out US$1.3 trillion in interest and principal. From 1991–1998, grants to developing countries went down from US$35 billion to US$23 billion [9].
UNESCO [97], at 10, has suggested that solidarity is an ethical imperative of growing importance given ideals of collective social protection and fair opportunity and the existence of serious inequalities in access to healthcare worldwide. Benatar et al. [9], claim that solidarity is the most important global health ethic and must be applied on a global basis. See also Mayor [71].
Indeed, the UN General Assembly has called for states to take measures to ensure that the results of scientific/technological advances are used for, and only for, the benefit of humankind: General Assembly Resolution 48/140, UN GAOR, 48th Sess., Supp. No. 49, UN Doc. A/48/49 (vol. 1) (1994).
The necessity for such collaborations is identified in the Bangkok Declaration (2000). See also Tollman [96], and Benatar and Singer [8]. The idea of capacity building in less enabled states is being pursued within Europe through the EU Framework Programs and the work of the EST, which encourages joint projects, multi-state funding and international peer review: Conference, “Towards a European Research Area” (Oct. 19–21, 2005).
For more on the inequity of the current distribution of medical resources, see www.pharmaportal.com, www.globalforumhealth.org.
See Article 27 of the UDHR (1948), Article 15 of the ICESCR (1966), and Articles 1, 2 and 7 of the Convention on Biological Diversity (1992), which espouse sharing technology so as to exploit and preserve biological/genetic resources, and Articles 12, 15, 16, 17 and 18 of the same Convention, which envision sharing knowledge, research and biotechnology with developing states.
Social and ethical accounting, auditing and reporting provides a practical mechanism for companies to integrate new patterns of civil accountability and governance with a business success model focused on deepening stakeholder relationships around both financial and non-financial interests, and that effective methods for doing so are evolving ([Zadek, 105], at 1428).
Cassel and Young [21], argue that over-reliance on autonomy-based consent in NHS research hinders the public good. Both Boter et al. [15], and Dawson [32], also describe research projects where obtaining prior informed consent was not appropriate. Bhagwanjee et al. [11], offer four conditions for foregoing consent.
It is at this stage that the differences between solidarity and altruism become apparent. Legislators are reluctant to legally impose altruism, rightfully likening that concept to a personal sense of unselfish concern for others which cannot be compelled. Its very definition implies the observance of conduct that is not demanded. I would suggest that solidarity is more active and, with its derivative duties, more appropriately compellable.
The Helsinki Declaration, adopted in 1964 and most recently revised in 2000 (with two subsequent “Clarifications”), was a response to the abuses perpetrated in Nazi Germany against involuntary human research subjects in the name of biomedical science. These abuses prompted the Nuremberg Trials and the subsequent Nuremberg Code, drafted by the US judges who tried the cases.
The CIOMS Guidelines, adopted in 1982 and most recently revised in 2002, is primarily concerned with the application of the Helsinki Declaration principles in the context of multinational research implicating developing countries. It was largely a response to the special concerns arising from the HIV/AIDS pandemic and research activities related thereto: see www.cioms.ch/guidelines_nov_2002_blurb.htm (Sep. 8/05).
Although it has been accused of representing the “doers” of research and not the “researched,” and of adopting an under-inclusive revision procedure [5]. The WMA [104] is comprised of representatives from approximately 80 national medical associations from all continents: see www.wma.net/e/about/index.htm (Sep. 2/05). CIOMS, founded under the auspices of the WHO and UNESCO in 1949, is comprised of 18 international organizations, 17 national representatives, and 25 associate members: see www.cioms.ch/frame_current_membership.htm (Sep. 7/05).
This interpretation is arrived at and lamented by Harris [52], and by Forster et al. [39], who also cite the removal of the distinction between therapeutic and non-therapeutic research in the new version as a weakness. However, Weijer and Anderson [100], state that the previous distinction between therapeutic and non-therapeutic research was a major flaw.
Indeed, there were almost immediate calls to revise Article 30, but the pressure to do so has thus far been resisted [40].
Christie [25], argues that something is either moral or not and the same ethical rules should apply wherever research is conducted.
Bastian [5], considers this a “limited approach” to the concept of access to research, which is absent in the Helsinki Declaration.
Although basic needs are common, disease burdens are not equally shared and capacities are not evenly enjoyed, so specific needs may be heterogeneous. As such, different communities will have different levels and particulars of needs (and responsibilities). This does not negate the validity of the statement that our needs draw us together, particularly now that global mobility is facilitating disease mobility.
One need only look at the impact of the SARS outbreak in China, which spread across the ocean to Canada. For more on that outbreak, see www.who.int/topics/sars/en/, and D. Macer (ed.) [67], at 24.
References
Angell M (2000) The pharmaceutical industry—To whom is it accountable. NEJM 352: 1902–1904
Arts W, Verburg R (2002) Modernisation, solidarity and care in Europe: The sociologist’s tale. In: ter Meulen R et al. (eds) Solidarity in health and social care in Europe. Springer, UK, pp 15–40
Ashcroft R et al (2000) Solidarity, society and the welfare state in the United Kingdom. Health Care Anal 8: 377–394
Azariah J (2003) Asian Bioethics in global society. In: Sang-yong S, Young-Mo K, Macer D (eds) Asian bioethics in the 21st century. Eubios, NZ, pp 219–223
Bastian H (2001) What are the effects of the fifth revision of the declaration of Helsinki? Gains and losses for rights of consumers and research participants. BMJ 323: 1417–1423
Benatar S (1998) Global disparities in health and human rights. AJPH 88: 395–400
Benatar S (2001) Distributive justice and clinical trials in the Third World. Theo Med 22: 169–176
Benatar S, Singer P (2001) Beyond Helsinki: A vision for global ethics. BMJ 322: 747–748
Benatar S, Daar A, Singer P (2003) Global health ethics: The rationale for mutual caring. Int Aff 79: 107–138
Benatar S (2004) Blinkered bioethics. JME 30: 291–292
Bhagwanjee S et al (1997) Why we did not seek informed consent before testing patients for HIV. BMJ 314: 1082
Bhutta Z (2002) Ethics in international health research: A perspective from the developing world. WHO Bull 80: 114–120
Bhutta Z (2004) Standards of care in research. BMJ 329: 1114–1115
Bond P (1999) Globalization, pharmaceutical pricing and South African health policy. IJHS 29(4): 765–792
Boter H et al (2004) Patients’ evaluation of informed consent to postponed information: Cohort study. BMJ 329: 86
Brownsword R (2005) Biotechnology and rights: Where are we coming from and where are we going?. In: Klang M, Murray A (eds) Human rights in the digital age. Glasshouse, London, pp 219–234
Bruce A, Tait J (2003) Interests, values and biotechnological risk. INNOGEN Working Paper 7, at www.innogen.ac.uk/publications/
Callahan D (2003) Principlism and communitarianism. JME 29: 287–291
Caplan A et al. (1999) The human genome project: What is immoral about eugenics? BMJ 319: 1284
Carpenter W et al (2003) The declaration of Helsinki and clinical trials: A focus on placebo-controlled trials in Schizophrenia. AJ Psychiatry 160: 356–362
Cassel J, Young A (2002) Why we should not seek individual informed consent for participation in heath service research. BMJ 328: 313–317
Chadwick R (1999) The Iceland database: Do modern times need modern sagas? BMJ 319: 441–444
Chadwick R, Berg K (2001) Solidarity and equality: New ethical frameworks for genetic databases. Nat Rev Genet 2: 318–321
Chee Khoon C (2003) Commodification and market-driven biomedical research. At www.biopolitics-berlin2003.org
Christie B (2000) Doctors revise declaration of Helsinki. BMJ 321: 913
Clarke M (2001) War in the new international order. Int Aff 77: 663–671
Commentary on Guideline 3, at www.cioms.ch/guidelines_nov_2002_blurb.htm
Commission on Intellectual Property Rights (2002) Integrating intellectual property rights and development policy. CIPR, London
Corrigan O (2004) Informed consent: The contradictory ethical safeguards in pharmacogenetics. In: Tutton R, Corrigan O (eds) Genetic databases: Socio-ethical issues in the collection and use of DNA. Routledge, London, pp 78–96
Crawley F, Hoet F (1999) Ethics and law: The declaration of Helsinki Under Discussion. Bull ME 150: 9–12
Davis M (1997) Constitutionalism and political culture: The debate over human rights and Asian values. Harv HRJ 10: 109–148
Dawson A (2004) Methodological reasons for not gaining prior informed consent are sometimes justified. BMJ 329: 87
de Bary W (1998) Asian values and human rights: A confucian communitarian perspective. Harvard U. Press, London
Deutsch E, Taupitz J (1999) Freedom of control and biomedical research. Bull ME 150: 22–24
Donne J, Meditation XVII (1624) Devotions upon emergent occasions. At http: //en.wikipedia.org/ wiki/john_donne
Eaton L (2005) Nuffield council calls for ethics framework for developing world research. BMJ 330: 618
Editorial (1999) The Helsinki declaration—Nothing to declare. Lancet 353: 1285
Elazar D (1999) Jewish civilization and polity in a globalized world: A new vision for organized jewry. At www.jcpa.org/dje/articles2/vision99.htm
Forster H et al (2001) The 2000 revision of the declaration of Helsinki: A step forward or more confusion? Lancet 358: 1449–1453
Frankish H (2003) WMA postpones decision to amend declaration of Helsinki. Lancet 362: 963
Fukuyama F (2002) Our posthuman future. Profile, London
Gevers J et al (2002) Popular support for health care in Europe: Review of the evidence of cross-national surveys. In: ter Meulen R, et al (eds) Solidarity in health and social care in Europe. Springer, UK, pp 41–76
Gillon R (2003) Ethics needs principles—Four can encompass the rest—and respect for autonomy should be ‘first among equals’.” JME 29: 307–312
Global Forum for Health Research (2004) 10/90 Report on health research 2003–2004. GFHR, Geneva
Goldsand G et al (2001) Bioethics for clinicians: Jewish bioethics. CMAJ 164: 219
Gwatkin D (2000) Health inequalities and the health of the poor: What do we know? What can we do? Bull WHO 78: 3–18
Habermas J (2003) The future of human nature. Polity Press, Cambridge
Halevi H The thirteen principles of Jewish medical ethics. At www.jewishpeople.net/jewmedet.htm
Halsey N et al (1999) Ethics and international research. BMJ 315: 965–966
Harmon S (2005a) The significance of UNESCO’s universal declaration on the human genome and human rights. SCRIPT-ed 2(1): 18–47, at www.law.ed.ac.uk/ahrb/script-ed/vol2-1/harmon.pdf
Harmon S (2005b) Regulation of human genomics & genetic biotechnology: Risks, values and analytical criteria. INNOGEN Working Paper 40, at www.innogen.ac.uk/publications/
Harris J (2005) Scientific research is a moral duty. JME 31: 242–248
Hayry M (2003) European values in bioethics: Why, what and how to be used? Theo Med 24: 1999–214
Hirsch L, Guess H (2001) Some clauses will hinder development of new drugs and vaccines. BMJ 323: 1417–1423
Houtepen R, ter Meulen R (2000a) New types of solidarity in the European welfare state. Health Care Anal 8: 329–340
Houtepen R, ter Meulen R (2000b) The expectation(s) of solidarity: Matters of justice, responsibility and identity in the reconstruction of the health care system. Health Care Anal 8: 355–376
HUGO Ethics Committee (2000) Statement on benefit sharing. At www.hugo-international.org/statement_on_benefit_sharing.htm
Human D, Fluss S (2001) The world medical association’s declaration of Helsinki: Historical and contemporary perspectives. At www.wma.net/e/ethicsunit/pdf/draft_historical_contemporary_perspectives.pdf
Joint UN Program on HIV/AIDS (2003) AIDS Epidemic Update 2003, Geneva, UN, available at www.unaids.org
Knoppers B (2004) Of biotechnology and man. Comm Gen 7: 176–181
Knoppers B (2005) Of genomics and public health: Building public ‘goods’?. CMAJ 173(10): 1185—1186.
Lansang M, Crawley, F (2000) The ethics of international biomedical research. BMJ 321: 777–778
Lolas F (2000) Ethics in international health research: The role of transnational organizations. At http: //bmj.bmjjournals.com/cgi/eletters/321/7264/777
Louw D (1997) Ubuntu: An African assessment of the religious other. At www.bu.edu/wcp/Papers/ Afr/AfriLouw.htm
MacDonald C (2003) Patents and benefit-sharing as a challenge for corporate ethics. In: Knoppers B (ed) Populations and genetics: Legal and socio-ethical perspectives. Martinus Nijhoff, Boston, pp 505–523.
Macer D, Su B (2004) Privacy versus public interest in developing human genetic databases. Eubios JAIB 14: 82–85
Macer D (ed) (2004) Bioethics for informed citizens across cultures. Eubios Ethics Institute, NZ
Macer D Love and the history of Chinese bioethics. At www.phil.pku.edu.cn/post/center/love%20and %20the%20history%20of%20chinese%20bioethics.html
Macklin R (2001) After Helsinki: Unresolved issues in international research. KIEJ 11: 17–36
Macklin R (2003) Bioethics, vulnerability, and protection. Bioethics 17: 472–486
Mayor F (1990) Statement at ‘Genetics, ethics and human values: Human genome mapping, genetic screening and gene therapy,’ 24th CIOMS Conference, Japan
Mayor F (1994) Preface. In: Proceedings of the first session of the IBC. UNESCO, Paris
McFaden A (1990) A call to personhood: A christian theory of the individual in social relationships. CUP, Cambridge
McGwire M (2001) Shifting the paradigm. Int Aff 77: 1–28
McGwire M (2001) The paradigm that lost its way. Int Aff 77: 777–803
McKibben W (2003) Enough. Bloomsbury, London
Morgan D (2002) Science, medicine and ethical change. In: Bainham A, et al (eds) Body lore and laws. Hart Publishing, Oxford, pp 329–342
Morgan P, Lawton C (eds) (1996) Ethical issues in six religious traditions. EUP, Edinburgh
Nuffield Council (2001) The ethics of clinical research in developing countries. NCB, London
Nuffield Council (2002) The ethics of research related to healthcare in developing countries. NCB, London
Nuffield Council (2005) The ethics of research related to healthcare in developing countries. NCB, London
Onen C (2004) Medicine in resource-poor settings: Time for a paradigm shift? Clin Med 4: 355–360
Pettifor A (1996) Debt, the most potent form of slavery. Christian Aid Society, London
Polansky L (2000) The ramifications of population. ZPG Reporter 32: 5–13
Pullman D, Latus A (2003) Reconciling social justice and economic opportunism: Regulating the newfoundland genome. In: Knoppers B (ed) Populations and genetics: Legal and socio-ethical perspectives. Martinus Nijhoff, Boston, pp 543–564
Resnik D (2004) The distribution of biomedical research resources and international justice. DWB 4: 42–57
Richards T (2002) Developed countries should not impose ethics on other countries. BMJ 325: 796
Schrecker T (2003) Benefit-sharing in the new genomic marketplace: Expanding the ethical frame of reference. In: Knoppers B (ed) Populations and genetics: Legal and socio-ethical perspectives. Martinus Nijhoff, Boston, pp 405–421
Shapiro K, Benatar S (2005) HIV prevention research and global inequality: Steps towards improved standards of care. J Med Ethics 31: 39–37
Sitthi-amorn C et al (2002) The Asian voice in building equity in health for development—From the Asian forum for health research. Health Pol Plan 17: 213–217
Steinbock B Rethinking the right to reproduce. At www.hsph.harvard.edu/organizations/healthnet/hupapers/reproright.html
Stenton G (2004) Biopiracy within the pharmaceutical industry: A stark illustration of how abusive, manipulative and perverse the patenting process can be towards countries of the south. EIPR 26(1): 17–26
Stuart S (2000) Species: Unprecedented extinction rate, and it’s increasing. IUCN Special Feature at www.iucn.org/info_and_news/press/species2000.html
Suzuki Y (2003) Keynote address: International conference of drug regulatory authorities. At www.whqlibdoc.who.int/hq/2003/a79903_(chp3).pdf
ter Meulen R et al (2000) Final report: Solidarity and care in the European Union. At http: //europa.eu.int/ comm/research/biosociety/pdf/bmh4_ct8_3971_partb.pdf
Tollman S (2001) What are the effects of the fifth revision of the declaration of Helsinki? Fair partnerships support ethical research. BMJ 323: 1417–1423
UNESCO (2005) Explanatory memorandum on the elaboration of the preliminary draft declaration on universal norms on bioethics. UNESCO, Paris
van Veen E (2005) Comments on the draft CIOMS international guidelines for ethical review of epidemiological studies. At www.medlaw.nl/documenten/comments.pdf
Wallerstein I (1999) The end of the world as we know it: Social science for the twenty-first century. UMP, Minnesota
Weijer C, Anderson J (2001) The ethics wars: Disputes over international research. Hastings Centre Report 31, No. 3
WHO (1999) Investing in health research and development. WHO Publications, Geneva
WHO (2003) The world health report 2003. WHO Publications, Geneva
WHO (2005) World health report 2005. WHO Publications, Geneva
WMA Working group report on the revision of paragraph 30 of the declaration of Helsinki. WG/DoH/Jan2004
Zadek S (1998) Balancing performance, ethics and accountability. J Bus Eth 17: 1421–1441
Zion D et al (2000) The declaration of Helsinki, CIOMS and the ethics of research on vulnerable populations. Nat Med 6: 615–617
Acknowledgement
Special thanks to Dr. Graeme Laurie, Chair of Medical Jurisprudence, University of Edinburgh, and Co-Director of the AHRC Research Centre for Studies in Intellectual Property and Technology Law.
Author information
Authors and Affiliations
Corresponding author
Additional information
Research Fellow, INNOGEN, ESRC Centre for Social and Economic Research on Innovation in Genomics; PhD Candidate in Law, University of Edinburgh; Member of the Nova Scotia Bar.
Rights and permissions
About this article
Cite this article
Harmon, S.H.E. Solidarity: A (New) Ethic for Global Health Policy. Health Care Anal 14, 215–236 (2006). https://doi.org/10.1007/s10728-006-0030-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10728-006-0030-8