Abstract
During a pandemic outbreak, it is important for health officials to know the proportions of deaths among infected individuals and to understand how these proportions change overtime, to accurately predict the impact of the pandemic and to implement effectively new intervention policies and health protocols and to adjust them accordingly. However, most studies where efforts have been made to estimate accurately the case fatality rates did not address the issue of measuring the dynamics of the pandemic deadliness during its course. Daily data on COVID-19 cases and deaths were collected from selected MENA countries. In this paper, two new measures of the pandemic fatality are developed based on the estimated time it takes hospitalized infected patients to eventually die from the disease. The first measure assigns COVID-19 deaths to its most significant lagged number of cases based on a fixed-effects panel data model. The second fatality measure relates pandemic deaths and cases based on their respective change points. The results find notable variations of the pandemic lethality between the Middle East countries, likely due to the difference in the quality of health care. Although crude case-fatality rate does not identify the pandemic lethality variations during the ongoing of the disease, this paper develops two novel measures for COVID-19 case fatality which can identify the dynamics and the variations of the pandemic deadliness.
Similar content being viewed by others
Introduction
It is worth noticing that some countries in the Middle East region were among the first outside China to be hit by the coronavirus pandemic, as indicated by World Health Organization official statistics (WHO, 2020). For instances, Iran had its first infection cases in February 2020, and as of February 2022, the Iranian government had reported nearly 135,500 COVID-19 related deaths, although it is suggested that the true number may be even higher. In Turkey, as of February 2022, statistics show more than 13 million people have been infected and nearly 93,000 are dead due to the pandemic. Other countries of the region were perhaps spared from the worst of the pandemic in the first few months, but their numbers of cases and deaths rose sharply after summer 2020. In almost 2 years into the pandemic the infection and death counts are still staggering as reported in Table 1.
Scholars who investigated the coronavirus outbreak situation in the Middle East region include Mohammad-Ebrahimi et al. (2021) who studied the epidemiologic characteristics of COVID-19 cases in north-eastern Iran through mapping the spatiotemporal trend of the disease. Also, Mohammadi et al. (2021) measured potential spatial access to COVID-19 vaccination centers in a large Iranian city.
Reports and published statistics showed that COVID-19 cases and deaths were still increasing until the summer of 2021 and only recently with more people being vaccinated those official statistics show a notable decrease in the number of deaths and in the number of people being hospitalized to the coronavirus pandemic. In addition, the statistics presented in Table 1 point to a high variation of pandemic fatality among MENA countries. But perhaps what is most important to notice is that some countries with high infection rates like Bahrain, Israel, Kuwait, and the United Arab Emirates (Khedhiri, 2021a) have the smallest death rates which imply that the coronavirus was less lethal in these countries. On the opposite side, statistics suggest that countries like Iran and Tunisia (Khedhiri, 2021b) with relatively smaller infection rates have higher death rates. This simple remark points to an important question about the accuracy of the traditional crude case-fatality rate in describing the pandemic lethality and its dynamics.
To develop more informative pandemic case-fatality measures, this study looks at similar trends between infection and death counts and introduces dynamic measures of COVID-19 case-fatality. These measures yield a comprehensive description of potential changes in the lethality of the pandemic during its course. The methods are illustrated with an empirical investigation of COVID-19 cases and deaths in the Middle East and North Africa countries in the following sections.
Methods and materials
CFR literature review
Crude CFR is defined as a percentage or a ratio to measure the number of confirmed deaths among the number of confirmed diagnosed cases of a particular disease at a given time. As argued by Shabir (2020), crude CFR heavily relies on confirmed cases and deaths and thus may not accurately reflect the total picture within the population due to unreported cases and subsequent deaths. In addition, this measure can vary considerably for the same disease across different cities and countries since much of this can depend on the population’s characteristics – such as average age, as well as access to robust and free healthcare systems, levels of previous immunity (vaccinations), and treatment strategies. One notable limitation of crude CFR as described by Shabir (2020) comes from the fact that it is unlikely that all cases or deaths due to a widespread disease will be detected or correctly designated. Delays in recordings of deaths and cases can also skew CFR. Another issue with the standard crude CFR may be explained by the factor of underestimation and the duration of time from symptom tod death (Shim, 2021). Fan et al. (2021) attempted to identify the dynamics of COVID-19 case-fatality rate by comparing this measure between two waves. This paper contributes to the literature by providing a more general method to identify possible changes of case-fatality variations and changes during the pandemic.
It is important to measure accurately the case fatality rate of COVID-19 because efficient intervention policies such as testing, self-isolation, lockdown and health protocols depend on it. Often, estimates of case-fatality and infection-fatality rates (IFR) are biased (Li et al., 2020; Basu, 2020) since the exact level of transmission may be underestimated either because many infected individuals do not show symptoms or because testing may not be available to everyone who needs it. Also, there are issues with finding credible statistical estimation of CFR which is the proportion of deaths among identified confirmed cases. This can only be obtained after all cases have been resolved. Thus, when the pandemic is still spreading, the crude CFR estimate does not inform about the dynamics and the variations of the deadliness of the disease and the efficiency of health protocols. Several studies showed that researchers and epidemiologists have attempted to find better estimates of case-fatality rates. For instance, in a recent study Yalaman et al. (2021) used regression analysis to estimate CFR based on testing policy variables, healthcare system capabilities and country characteristics, and Park et al. (2021) analyzed the associations between case-fatality ratio and factors related to the quality of care in hospitals in Korea. Also, Kim et al. (2020) estimated case fatality rate of the coronavirus for several countries and asked for caution when it comes to the interpretation of these estimates, and Abdollahi et al. (2020) referred to daily incidence of COVID-19 cases and deaths in Canada and the US to adjust for potential biases in estimating crude CFR. In Table 2, estimated crude CFR of COVID-19 for the MENA countries are reported.
To present a full assessment of the dynamics of pandemic lethality, we need clinical data on patients and information and admission and release dates and dated hospitalization and deaths for the symptomatic patients who were admitted in the hospital. This information is either hard to obtain or is not reliable especially for countries where the public health system is still developing. Thus, one objective of this paper is to correctly assign COVID-19 deaths when they are detected without the use of patients’ personal health records. This study suggests computing multiple case-fatality rates which depend on similar infection and death trends of the pandemic. Two methods are developed in this paper by answering the following question: At some point in time during the pandemic when where the identified dead individuals from COVID-19 most likely infected.
In the first method, death counts are estimated as a function of current and lagged numbers of cases with a panel data model. In the second method, a change point analysis is performed to find the death and infection counts that are most likely related to each other and thus they can infer about the dynamics of the lethality of the pandemic in each country.
Data sources
Data are collected on the cumulative number of infections and deaths related to the pandemic in the MENA countries. These data are publicly available online (https://www.statista.com/statistics/1104709/coronavirus-deaths-worldwide-per-million-inhabitants/) and they cover the period from March 24, 2020 to April 21, 2021. It should be noticed that we looked at different online resources where the data are available to compare the reported numbers and to minimize the issue of data reliability. Thus, data from Jordan and Yemen could not be included in this study since some of their published cumulative counts of death and infection show decreasing numbers.
In addition, based on a broader definition of MENA region (Middle East and North Africa) we also included Turkey in the study. Therefore, the list of countries included in this paper are Algeria, Bahrain, Egypt, Iran, Iraq, Israel, Kuwait, Lebanon, Libya, Morocco, Palestine, Qatar, Saudi Arabia, Syria, Tunisia, Turkey, and United Arab Emirates. A total of 394 daily observations for each of the 18 countries were used in the statistical analysis.
Suggested new measures of case fatality rates
In the first measure, a model is estimated for deaths explained by lagged cases in a panel-data fixed effect model as follows:
where i = 1…18 and t = 1…394, \(\mu_{i,0}\) is a fixed effect and \(\varepsilon_{i,t}\) is the error term. The optimal value of l is equal to 7, based on AIC and coefficient significance. This value is specific to the data collected. The idea is that the number of lags in the most significant lagged cases will determine, approximately, the average time length (measured by the number of days) it takes the virus to cause death.
Model Eq. (1) was run with alternative lag lengths, using R software. Following AIC information criterion, the number of lags equals to 7 is chosen in the fixed effects panel data model. The dependent variable is defined as the number of deaths and the independent variable is the lagged number of cases with lag l equals to 7 days. The estimated coefficient is 0.00565 and shows statistically significance at the 5% level with a t-statistic equals to 3.547. This statistical finding indicates that the more likely approximation of the time it takes the coronavirus to kill infected individuals in the Middle East region is equal to seven days, on average.
Therefore, it is suggested to form a series of CFR for each country i at each time t, based on the following measure:
where \(deaths_{it} = \frac{1}{3}\sum\nolimits_{j = t - 1}^{t + 1} {deaths_{i.j} }\), and \(cases_{i,t - 7} = \frac{1}{3}\sum\nolimits_{{j = \left( {t - 7} \right) - 1}}^{{\left( {t - 7} \right) + 1}} {cases_{i,j} }\), for each country i.
It can be noticed that death and case counts are computed from averaging present, one lead, and one lag counts. This idea of allowing one point of margin is to avoid single zero counts and to have smoother approximations.
In the next step, a series of case-fatality rates are obtained for each country as shown in Table 2.
The estimated CFR1values are based on the statistical modeling and the significant result for the relationship between infection and death. This measure estimates the average time it takes infected patients in the Middle East to die and therefore is identifies accurately infected individuals who are likely to eventually die from the disease. It is shown from Table 2 that the traditional crude case-fatality rates underestimate the proportion of dead patients who are COVID-19 infected.
Next, an econometric model is developed to study the relationship between case-fatality measures and country-specific explanatory variables. Data on per-capita GDP and population size of each MENA country are collected and GLM statistical method (generalized linear model) is executed to estimate model Eq. (3):
where \(CFR_{1,i}\) is the GLM estimate of the average case-fatality rates which were reported for each country in Table 2, growth is the per-capita GDP, and pop refers to the population size in millions. The t-statistics of the model parameters are given in parentheses and the p-values are 0.001, 0.051, and 0.096 for the constant, the growth coefficient, and the population coefficient, respectively. In addition, for the statistical results of model (3) we can also report that AIC is equal to 69.779, and that the null and the residual deviances are 61.239 and 32.612, respectively. These findings show unequivocal statistical evidence that COVID-19 is less lethal in more prosperous countries in the Middle East, but perhaps there is less evidence that the pandemic is more fatal in more populated countries. It can be noted that the findings of this paper are different from those reported by Cao et al. (2020) in which it was found that the association between population size and COVID-19 CFR implies the healthcare strain and lower treatment efficiency in countries with large populations.
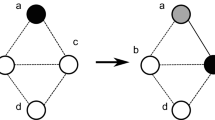
An alternative method to obtain a dynamic measure of case fatality for the COVID-19 pandemic is presented next and it assumes that it is more likely to observe a high number of deaths from an associated high number of cases than from an associated low number of case, and vice-versa. To compute this measure, the first step is to estimate the change points for death and infection counts to find a possible connection based on common trends between the two counts during similar cycles, whether growth or decline.
The statistical estimation of mean change points in the time series counts of both deaths and cases for each country are performed with the cumulative sum method in R software. This method was studied and illustrated in climatological and epidemiological applications. For instance, Kass-Hout et al. (2012) applied change point analysis to study emergency department visits of patients with influence-like symptoms and You et al. (2021) conducted a study to detect vaccine safety signals.
Results and discussion
In this study we used the R package strucchange to compute the optimal number of breakpoints. The results are displayed in Tables 3 and 4 for deaths and cases, respectively.
The paper aimed to develop two novel measures of case-fatality which depict the dynamics of the pandemic deadliness and to apply these measures to study COVID-19 infections and deaths in the Middle East and to investigate the difference in the quality of health care related to the differences and the variations of the pandemic lethality between these countries.
The first measure is obtained from estimated case-fatality rates which are based on the statistical modeling of the relationship between infection and death. This measure estimates the average time it takes infected patients to die from the disease.
The second measure of case-fatality rate is based on a change point analysis. The new rates are computed as follows:
where for each country i,\(deaths_{it} = \frac{1}{5}\sum\nolimits_{j = t - 2}^{t + 2} {death\;count_{i,j} }\), \(cases_{i\tau } = \frac{1}{5}\sum\nolimits_{j = \tau - 2}^{\tau + 2} {case\;count_{i,j} }\), and the change pointe date \(\tau\) of cases lags the change point date \(t\) of deaths by 1 to 21 days. The counts are from similar cycles either growing or declining numbers. Also, infection and death counts cannot be more than 21 days apart in a cycle. The change point for the number of cases must precede immediately the change point for the number of deaths. In addition, in the computations of this case-fatality measure two points of margin in the counts are allowed, that is 2 leads and 2 lags. The change point dates for each Middle East country and the second new measures of pandemic case-fatality, denoted by CFR2, are displayed in Table 5. It is shown that there are notable variations of the pandemic lethality between the Middle East countries. This may be explained by the difference in the quality of health care for symptomatic patients.
To elaborate further on the suggested idea of CFR2, suppose a cycle of increasing numbers of deaths from which the highest number is selected, call it \(deaths_{it}\). We look at the similar cycle of increasing numbers of cases that immediately precedes the death count cycle, if it does not lag by more than 21 days. From that cycle, the highest number of cases is chosen, call it \(cases_{i\tau }\). Next, these counts are updated by accounting for a margin of two days. Finally, the new measure will estimate more accurately the proportion of patients who were infected and eventually who have died during a specific cycle of the pandemic. It should be noted that these rates cannot be computed if one count is not available (NA) during the cycle or if the infection break point time does not lag the death break point time by at most 21 days during the same cycle. An example to illustrate the detailed steps for the calculation of this measure is presented in the appendix.
The variations and the dynamics of COVID-19 case-fatality for the MENA countries can be explained by the difference in the quality of health care for patients who were admitted in the hospitals. It is found that there are four clusters of countries according to their pattern of pandemic lethality which decreases over time for Algeria, Iran, Iraq, Palestine, Turkey, and the United Arab Emirates. The overall trend increases for Egypt, Oman, Saudi Arabia, Tunisia, Lebanon, and Kuwait. It goes up and then declines for Bahrain and Qatar, and it fluctuates in the opposite direction for Morocco and Israel. However, for Libya, there is only one possible estimate of case-fatality rate of the coronavirus disease and therefore there are no variations. The new measure of fatality rates may be described as shown in Fig. 1.
Conclusion
Crude case-fatality rate and other related measures suggested in the epidemiologic literature are biased and at best do not provide any information on how the deadliness of a pandemic progresses over time. This paper addresses the issue and presents alternative dynamic measures of case-fatality based on the assessment of pandemic lethality and the estimated time between infection and death. The methods identify the variations in the lethality of the virus which is likely due to the difference of the quality of health care for hospitalized symptomatic patients. An empirical investigation is carried out to study the coronavirus pandemic outbreak in the Middle East region and to assess the difference in the dynamics and the variations of its lethality between these countries due to the difference in the quality of their health care.
The findings of this paper show that traditional crude case fatality rates are overall underestimated, and they do not identify the possible variations of COVID-19 deadliness during the outbreak. The suggested new measures allow to have a comprehensive analysis of how the pandemic lethality may change and therefore can help health officials adjust their interventions and their health services accordingly. However, the results obtained in this paper depend on the reported daily counts of cases and deaths which may lack accuracy and reliability.
As noted in the World Health Organization report (WHO, 2020), one crucial feature of an infectious disease caused by a novel pathogen like the coronavirus, is its severity and the ultimate measure of which is its ability to cause death. Fatality rates can help health officials understand the severity of the disease and identify at-risk populations and evaluate the quality of healthcare to make recommendations as how to improve it. However, the resulting interventions and health policies can be more effective if these measures of case-fatality rates can also identify how the disease fatality might change during the outbreak and thus it would be crucial to evaluate accurately not only the differences in mortality between groups of people within each country and between countries (Sorci et al., 2020) but also to identify the potential variations of disease fatality. The main contribution of this paper is to develop new methods of case fatality rates that allow to know how the pandemic lethality varies during the outbreak. This can help health officials find efficient policies regarding the allocation of medical resources and better strategies to reduce the fatal impact of the pandemic.
Data availability
Data is publicly available online.
References
Abdollahi, E., Champredon, D., Langley, J., Galvani, A., & Moghada, S. E. (2020). Temporal estimates of case-fatality rate for COVID-19 outbreaks in Canada and the United States. Canadian Medical Association Journal, 192(55), E666–E670. https://doi.org/10.1503/cmaj.200711
Basu, A. (2020). Estimating the infection fatality rate among symptomatic COVID-19 cases in the United States. Health Affairs, 39(7), 1229. https://doi.org/10.1377/hlthaff.2020.00455
Cao, Y., Hiyoshi, A., & Montgomery, S. (2020). COVID-19 case-fatality rate and demographic and socioeconomic influences: Worldwide spatial regression analysis based on country-level data. British Medical Journal Open, 10(11), e043560. https://doi.org/10.1136/bmjopen-2020-043560
Fan, G., Yang, Z., Lin, Q., Zhao, S., Yang, L., & He, D. (2021). Decreased case fatality rate of COVID-19 in the second wave: A study in 53 countries or regions. Transboundary and Emerging Diseases, 86(2), 213–215. https://doi.org/10.1111/tbed.13819
Kass-Hout, T. A., Xu, Z., McMurray, P., et al. (2012). Application of change point analysis to daily influenza-like illness emergency department visits. Journal of the American Medical Informatics Association, 19(6), 1075–1081. https://doi.org/10.1136/amiajnl-2011-000793
Khedhiri, S. (2021a). Forecasting COVID-19 infections in the Arabian Gulf region. Modeling Earth Systems and Environment, 6, 1–10. https://doi.org/10.1007/s40808-021-01332-z
Khedhiri, S. (2021b). Statistical modeling of COVID-19 deaths with excess zero counts. Epidemiologic Methods, 10(s1), 20210007.
Kim, D. F., Choe, Y. J., & Jeong, J. Y. (2020). Understanding and interpretation of case fatality rate of coronavirus disease 2019. Journal of Korean Medical Science, 35(12), e137. https://doi.org/10.3346/jkms.2020.35.e137
Li, R., & Pei, S. (2020). Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science, 368(6490), 489–493. https://doi.org/10.1126/science.abb3221
Mohammadi, A., Mollalo, A., Betgquist, R., & Kiani, B. (2021). Measuring COVID-19 vaccination coverage: An enhanced age-adjusted two-step floating catchment area model. Infectious Diseases of Poverty, 10(118), 1–13. https://doi.org/10.1186/s40249-021-00904-6
Mohammad-Ebrahimi, S., Mohammadi, A., Bergquist, R., et al. (2021). Epidemiological characteristics and initial spatiotemporal visualisation of COVID-19 in a major city in the Middle East. BMC Public Health, 21(1373), 1–18. https://doi.org/10.1186/s12889-021-11326-2
Park, E. H., Gil, Y. J., Kim, C., Kim, B. J., & Hwang, S. (2021). Presence of thrombectomy-capable stroke centers within hospital service area explain regional variations in the case fatality rate of acute ischemic stroke in Korea. Journal of Preventive Medicine and Public Health, 54(6), 385–394. https://doi.org/10.3961/jpmph.21.329
Shabir, O., (2020). What is case-fatality rate (CFR)? News medical life sciences. https://www.news-medical.net/health/What-is-Case-Fatality-Rate-(CFR).aspx
Shim, E. (2021). Regional variability in COVID-19 case fatality rate in Canada, february–december 2020. International Journal of Environmental Research and Public Health, 18(4), 1839. https://doi.org/10.3390/ijerph18041839
Sorci, G., Faivre, B., & Morand, S. (2020). Explaining among-country variations in COVID-19 case fatality rate. Scientific Reports, 10(18909), 1–11. https://doi.org/10.1038/s41598-020-75848-2
World Health Organization (2020) Estimating mortality from COVID-19. WHO Scientific Brief. https://www.who.int/news-room/commentaries/detail/estimating-mortality-from-covid-19
Yalaman, A., Basbug, G., Elgin, C., & Galvani, A. (2021). Cross-country evidence on the association between contact tracing and COVID-19 case fatality rates. Scientific Reports, 11(2145), 1–6. https://doi.org/10.1038/s41598-020-78760-x
You, S. H., Jang, E. J., Kim, M. S., et al. (2021). Analysis for detecting vaccine safety signals. Vaccines, 9(3), 206. https://doi.org/10.3390/vaccines9030206
Funding
No funding information to report for this article.
Author information
Authors and Affiliations
Contributions
I am the sole author of this paper and thus I am the only contributor of its content.
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interests for this article.
Ethics approval
This article uses publicly available data and therefore ethics approval is not required.
Human or animal rights
This research does not involve human or animal participation. The data used in this research is publicly available online and therefore ethical approval is not needed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
In Fig.
2, we show an example on how to compute the case fatality rates based on change points of COVID-19 cases and deaths. Suppose the number of cases (in hundreds) is displayed by the blue curve and the number of deaths (in tens) is given by the red curve. The change point corresponds to an abrupt change or a significant shift of the trend of the variable. For instance, in Fig. 2 let us denote by \(d_{t}\) the change point in the number of deaths which matches 30 units (or 300) new coronavirus related deaths. It occurs at time t. Also let \(c_{\tau }\) denote the change point in new cases which corresponds to 80 units (or 8000) new infections, and it occurs at time \(\tau\). In our analysis the time lag between the death and the infection change-points, which is given by t − τ, should be between 1 and 21 days in each cycle. Now we apply Eq. (4) to form a series of case-fatality rates that can describe the variations and the dynamics of the pandemic deadliness.
Rights and permissions
About this article
Cite this article
Khedhiri, S. COVID-19 case-fatality variations with application to the Middle East countries. GeoJournal 88, 1127–1137 (2023). https://doi.org/10.1007/s10708-022-10635-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10708-022-10635-2