Abstract
Background
Patients with NAFLD are considered at a high risk of cardiovascular events due to underlying metabolic risk factors. Currently, data related to the impact of NAFLD on cardiovascular risk in the general population are lacking.
Aims
The aim of this study was to investigate the role of NAFLD on risk of myocardial infarction (MI), coronary heart disease (CHD), atrial fibrillation (AF), and stroke in primary care in Germany.
Methods
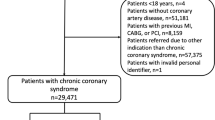
The study included patients diagnosed with NAFLD in primary care between 2010 and 2015. NAFLD cases (n = 22,048) were matched to a cohort without NAFLD (n = 22,048) based on age, sex, treating physician, type 2 diabetes, arterial hypertension, and hyperlipidemia. The primary outcome of the study was the incidence of MI, CHD, AF, and stroke.
Results
Within 10 years of the index date, 12.8% of patients with NAFLD and 10.0% of controls were diagnosed with CHD (p < 0.001). Additionally, frequency of MI was significantly higher in NAFLD (2.9% vs. 2.3%, p < 0.001). On regression analysis, HR for incidence of MI was 1.34 (p = 0.003) in all NAFLD patients and 1.35 (p = 0.013) for men. Incidence of AF was significantly higher in patients with NAFLD. On regression analysis, HR for incidence of AF was 1.15 (p = 0.005). NAFLD was not associated with a higher incidence of stroke (HR 1.09, p = 0.243).
Conclusions
NAFLD constitutes an independent risk factor for CHD, MI, and AF in primary care in Germany. Identification of patients with NAFLD in primary care will allow specifically managing and modifying underlying risk factors to improve the overall prognosis.





Similar content being viewed by others
Abbreviations
- NAFLD:
-
Nonalcoholic fatty liver disease
- NASH:
-
Nonalcoholic steatohepatitis
- CVD:
-
Cardiovascular disease
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
References
Younossi Z, Tacke F, Arrese M, et al. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology. 2019;69:2672–2682.
Schuppan D, Schattenberg JM. Non-alcoholic steatohepatitis: pathogenesis and novel therapeutic approaches. J Gastroenterol Hepatol. 2013;28:68–76.
Estes C, Anstee QM, Arias-Loste MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol. 2018;69:896–904.
Schattenberg JM, Schuppan D. Nonalcoholic steatohepatitis: the therapeutic challenge of a global epidemic. Curr Opin Lipidol. 2011;22:479–488.
Schattenberg JM, Loomba R. Refining noninvasive diagnostics in nonalcoholic fatty liver disease: closing the gap to detect advanced fibrosis. Hepatology. 2019;69:934–936.
Liebig S, Stoeckmann N, Geier A, et al. Multicenter validation study of a diagnostic algorithm to detect NASH and fibrosis in NAFLD patients with low NAFLD fibrosis score or liver stiffness. Clin Transl Gastroenterol. 2019;10:e00066.
Younossi Z, Anstee QM, Marietti M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20.
Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148:547–555.
Huber Y, Pfirrmann D, Gebhardt I, et al. Improvement of non-invasive markers of NAFLD from an individualised, web-based exercise program. Aliment Pharmacol Ther. 2019;50:930–939.
Dulai PS, Singh S, Patel J, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 2017;65:1557–1565.
Ekstedt M, Hagstrom H, Nasr P, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61:1547–1554.
Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol. 2016;65:589–600.
Golabi P, Paik J, Fukui N, Locklear CT, de Avilla L, Younossi ZM. Patients with lean nonalcoholic fatty liver disease are metabolically abnormal and have a higher risk for mortality. Clin Diabetes. 2019;37:65–72.
Labenz C, Prochaska JH, Huber Y, et al. Cardiovascular risk categories in patients with nonalcoholic fatty liver disease and the role of low-density lipoprotein cholesterol. Hepatol Commun. 2019;3:1472–1481.
Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10:330–344.
Ndumele CE, Nasir K, Conceicao RD, Carvalho JA, Blumenthal RS, Santos RD. Hepatic steatosis, obesity, and the metabolic syndrome are independently and additively associated with increased systemic inflammation. Arterioscler Thromb Vasc Biol. 2011;31:1927–1932.
Santos RD, Valenti L, Romeo S. Does nonalcoholic fatty liver disease cause cardiovascular disease? Current knowledge and gaps. Atherosclerosis. 2019;282:110–120.
Labenz C, Huber Y, Kalliga E, et al. Predictors of advanced fibrosis in non-cirrhotic non-alcoholic fatty liver disease in Germany. Aliment Pharmacol Ther. 2018;48:1109–1116.
Rathmann W, Bongaerts B, Carius HJ, Kruppert S, Kostev K. Basic characteristics and representativeness of the German Disease Analyzer database. Int J Clin Pharmacol Ther. 2018;56:459–466.
Zwiener I, Blettner M, Hommel G. Survival analysis: part 15 of a series on evaluation of scientific publications. Deutsches Arzteblatt International. 2011;108:163–169.
Alexander M, Loomis AK, van der Lei J, et al. Risks and clinical predictors of cirrhosis and hepatocellular carcinoma diagnoses in adults with diagnosed NAFLD: real-world study of 18 million patients in four European cohorts. BMC Med. 2019;17:95.
Schattenberg JM, Ekstedt M. Assessing the disease burden of non-alcoholic fatty liver disease in the real world—big data and big numbers. BMC Med. 2019;17:123.
Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol. 2012;10:646–650.
Sinn DH, Kang D, Chang Y, et al. Nonalcoholic Fatty liver disease and the incidence of myocardial infarction: a cohort study. J Gastroenterol Hepatol. 2019. https://doi.org/10.1111/jgh.14856
Targher G, Bertolini L, Poli F, et al. Nonalcoholic fatty liver disease and risk of future cardiovascular events among type 2 diabetic patients. Diabetes. 2005;54:3541–3546.
Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62:S47–S64.
Golabi P, Fukui N, Paik J, Sayiner M, Mishra A, Younossi ZM. Mortality risk detected by atherosclerotic cardiovascular disease score in patients with nonalcoholic fatty liver disease. Hepatol Commun. 2019;3:1050–1060.
Francque SM, van der Graaff D, Kwanten WJ. Non-alcoholic fatty liver disease and cardiovascular risk: pathophysiological mechanisms and implications. J Hepatol. 2016;65:425–443.
Pockros PJ, Fuchs M, Freilich B, et al. CONTROL: A randomized phase 2 study of obeticholic acid and atorvastatin on lipoproteins in nonalcoholic steatohepatitis patients. Liver Int. 2019. https://doi.org/10.1111/liv.14209
Petta S, Argano C, Colomba D, et al. Epicardial fat, cardiac geometry and cardiac function in patients with non-alcoholic fatty liver disease: association with the severity of liver disease. J. Hepatol. 2015;62:928–933.
Hu J, Xu Y, He Z, et al. Increased risk of cerebrovascular accident related to non-alcoholic fatty liver disease: a meta-analysis. Oncotarget. 2018;9:2752–2760.
Kim SU, Song D, Heo JH, et al. Liver fibrosis assessed with transient elastography is an independent risk factor for ischemic stroke. Atherosclerosis. 2017;260:156–162.
Wong RJ, Liu B, Bhuket T. Significant burden of nonalcoholic fatty liver disease with advanced fibrosis in the US: a cross-sectional analysis of 2011-2014 National Health and Nutrition Examination Survey. Aliment Pharmacol Ther. 2017;46:974–980.
Mensink G, Schienkiewitz A, Haftenberger M, Lampert T, Ziese T, Scheidt-Nave C. Overweight and obesity in Germany. Bundesgesundheitsbl. 2013;56:786–794.
Hebebrand J, Dabrock P, Lingenfelder M, Mand E, Rief W, Voit W. Ist Adipositas eine Krankheit? Interdisziplinäre Perspektiven. Dtsch Arztebl International. 2004;101:A-2468.
Funding
This work was in part funded by intramural finds of the University Medical Center Mainz.
Author information
Authors and Affiliations
Contributions
CL, KK, and JMS performed research; CL, YH, MM, MN, PRG, KK, and JMS designed the experiments and analyzed the data; KK provided reagents/materials/analysis tools; CL and JMS wrote the paper; and KK was involved in statistical analysis. All authors approved the final version of the manuscript and the authorship list.
Corresponding author
Ethics declarations
Conflict of interest
KK is an employee of IQVIA. JMS has acted as consultant to: Boehringer Ingelheim, Galmed, Genfit, Gilead Sciences, Intercept Pharmaceuticals, IQVIA, and has received research funding from Gilead Sciences. The other authors have nothing to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Guarantor of the article: J.M.S.
Rights and permissions
About this article
Cite this article
Labenz, C., Huber, Y., Michel, M. et al. Impact of NAFLD on the Incidence of Cardiovascular Diseases in a Primary Care Population in Germany. Dig Dis Sci 65, 2112–2119 (2020). https://doi.org/10.1007/s10620-019-05986-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05986-9