Abstract
Levosimendan, a calcium sensitizer and potassium channel-opener, is widely appreciated by many specialist heart failure practitioners for its effects on systemic and pulmonary hemodynamics and for the relief of symptoms of acute heart failure. The drug’s impact on mortality in large randomized controlled trials has been inconsistent or inconclusive but, in contrast to conventional inotropes, there have been no indications of worsened survival and some signals of improved heart failure-related quality of life. For this reason, levosimendan has been proposed as a safer inodilator option than traditional agents in settings, such as advanced heart failure. Positive effects of levosimendan on renal function have also been described. At the HEART FAILURE 2018 congress of the Heart Failure Association of the European Society of Cardiology, safe and effective use levosimendan in acute and advanced heart failure was examined in a series of expert tutorials. The proceedings of those tutorials are summarized in this review, with special reference to advanced heart failure and heart failure with concomitant renal dysfunction. Meta-analysis of clinical trials data is supportive of a renal-protective effect of levosimendan, while physiological observations suggest that this effect is exerted at least in part via organ-specific effects that may include selective vasodilation of glomerular afferent arterioles and increased renal blood flow, with no compromise of renal oxygenation. These lines of evidence require further investigation and their clinical significance needs to be evaluated in specifically designed prospective trials.
Similar content being viewed by others
Introduction
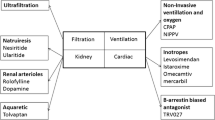
The pharmacological effects of levosimendan, an inodilator indicated for the treatment of decompensated heart failure, are exerted via three pathways (Fig. 1) [1]: (1) increased sensitivity of troponin C to calcium in myocardial cells, thereby inducing a cAMP-independent inotropic effect; (2) opening of adenosine triphosphate-sensitive potassium channels (KATP channels) in the smooth muscle cells of the vasculature, so inducing vasodilation; and (3) activation of KATP channels in cardiac mitochondria, hence protecting cells against ischemia/reperfusion injury [1]. As it is a calcium sensitizer not a calcium mobilizer [2, 3], levosimendan does not increase myocardial oxygen consumption [4, 5], and prevents myocardial apoptosis and remodeling [6, 7].
mechanisms of action of levosimendan (data from Papp et al. [1])
In its clinical development program, levosimendan showed beneficial effects on hemodynamic parameters, symptoms, and neurohormones, with a characteristic prolonged pharmacokinetics [8], and an overall positive effect on mortality [9]. Although some pivotal clinical trials failed to show superiority against comparators in terms of survival [10, 11], other regulatory trials [12, 13] as well as the results of the large ALARM-HF registry [14] showed a favorable impact of levosimendan on clinical outcomes, versus either placebo or other inotropes such as dobutamine.
In addition, various lines of clinical investigation have produced indications of a net beneficial impact of levosimendan on renal dysfunction [10, 15,16,17,18,19,20].
At the 2018 congress of the Heart Failure Association of the European Society of Cardiology (HEART FAILURE 2018, Vienna, Austria, May 27–28), a series of tutorials by experts from nine European countries (Austria, Belgium, Denmark, Finland, Germany, Greece, Hungary, Italy, and Sweden) was delivered examining how to use levosimendan safely and effectively in acute heart failure (AHF) and advanced heart failure (AdHF), including an appraisal of its impact in concomitant renal dysfunction. This review summarizes some of those expert perspectives on the optimized use of levosimendan in these settings.
Levosimendan in the Clinical Literature
Levosimendan’s current indication for the short-term treatment of acutely decompensated severe chronic heart failure in situations where conventional therapy is not sufficient and where inotropic support is appropriate rests on experience in clinical trials from which a series of salient features was identified.
-
1.
Improved systemic and pulmonary hemodynamics [12, 21, 22] with no significant increase in myocardial oxygen consumption [23, 24]
- 2.
-
3.
A theoretically beneficial effect on neurohormone profile [10, 11]
-
4.
Prolonged duration of effect due to the formation of an active metabolite designated OR-1896 [25, 26]
-
5.
Unlike dobutamine, effective also in patients treated with beta-blockers [12, 27]
The safety profile of levosimendan that emerged from these studies was largely reassuring [10, 12, 22], with no impairment of diastolic function [28, 29] or development of tolerance [26]. Common adverse events associated with levosimendan use are hypotension, headache, atrial fibrillation, hypokalemia, and tachycardia [1].
The results of small exploratory clinical trials of levosimendan in AdHF have been summarized by Nieminen et al. [30] and were generally affirmative but inevitably of limited statistical resilience. Two larger studies were subsequently performed and reported: the LEVOREP [31], and LION-HEART [32] clinical trials. As appraised by Pölzl et al. in a consensus opinion paper [33], those studies supported the view that repetitive i.v. use of levosimendan in AdHF patients delivered overall benefit in terms of improved hemodynamics, symptom relief, re-hospitalization rates, biomarkers, and survival but at least one additional suitably-powered clinical trial in AdHF is desirable to set these conclusions on a firm basis of evidence.
Meta-analyses of levosimendan data in various settings, including AHF and AdHF, indicated a trend towards a survival benefit that reached statistical significance in some investigations [34,35,36] though not all [37, 38]. These discrepancies may have reflected the various selection criteria applied and the precise natures of the study populations. The larger pooled analyses were less likely to identify a robust survival gain and the authors of many of these investigations signaled the need for more extensive prospectively derived data. Of note, however, none of these meta-analyses produced any indication that the use of levosimendan is associated with an increase of mortality, whereas a worsening impact on survival has been reported for other inotropes or inodilators [39, 40].
Levosimendan: From Guidelines to Clinical Practice
The 2016 ESC guidelines on acute and chronic heart failure assign the same level of evidence and class of recommendation to all inotropes (Class IIb/Evidence level C) but distinguish levosimendan due to its particular mode of action and recommend its use in cases where there is concomitant use of beta-blockers [41]. It is not clear how widely that advice is implemented in real-life clinical practice.
The latest (2018) position statement of the Heart Failure Association of the European Society of Cardiology on Advanced Heart Failure (HFA-ESC) on AdHF [42] comments that “Although patients with chronic heart failure have improved outcomes with implementation of evidence-based therapies, ultimately, they still progress to an advanced stage of the disease.” The authors advise that patients with severe symptoms and reduced exercise capacity, or who endure frequent and repeated hospitalizations, are often refractory to (or cannot tolerate maximal doses of) established therapies and therefore need something in addition to standard-of-care medication.
Considered from this perspective levosimendan has attractive features relevant to AdHF and is distinctly different from dobutamine and milrinone. Notably, two meta-analyses associate repeated use of levosimendan in advanced heart failure with improved survival [35] and reduced re-hospitalization [43] (Fig. 2). Given that patients with AdHF may comprise up to 10% of the overall heart failure population [44,45,46], these benefits may be accessible to substantial numbers of patients. The long duration of action of levosimendan, due to its OR-1896 metabolite [1, 25, 26], is also relevant in this context. The position statement of the HFA-ESC [43] further notes that “…intermittent use of inodilators for long-term symptomatic improvement or palliation has gained popularity, especially use of levosimendan, since the hemodynamic effect may last for >7 days after a 12–24h infusion.” This may be considered as a fair summary of practice in this area.
Guidance and expert consensus [30, 47] advise that levosimendan should ordinarily be administered without a loading bolus (to minimize risk of hypotension). The continuous 24-h infusion of levosimendan should be administered at a rate of 0.05–0.1 μg/kg/min. (Some clinicians start levosimendan infusion at a higher rate, 0.2 μg/kg/min for the first 60 min in order to reach the desired therapeutic effect more rapidly, and then reduce the dose to 0.1 μg/kg/min.) It should be recalled that levosimendan has profound vasodilatory effects; accordingly, it should be administered with caution in patients with low blood pressure. Hypovolemia should be avoided before and during levosimendan treatment (give fluid as needed; reduce intravenous diuretics when necessary) and measures taken to avoid hypokalemia (serum/plasma potassium levels should be kept ≥ 4.0 mmol/l during levosimendan infusion).
Heart Failure and Renal Function: a Role for Levosimendan?
Renal dysfunction is frequently associated with heart failure and is implicated in worse prognosis [48], and further detriment of QoL [49]. Five types of cardiorenal syndrome (CRS) with distinct pathophysiologies and clinical presentations have been described [50].
In patients with heart failure, CRS tends to be encountered as either Type 1 CRS (worsening of renal function during treatment for cardiac decompensation) or Type 2 CRS (reduced glomerular filtration rate [GFR] [< 60 mL/min/1.73 m2]): both carry a worse prognosis than heart failure without attendant renal dysfunction. Multiple mechanisms contribute to kidney damage in these forms of CRS, including hypoperfusion, renal venous congestion, interstitial fibrosis, tubular damage, and nephron loss are linked to neurohormonal activation.
The use of inodilators or inotropes may be particularly beneficial in cases of acute CRS in patients with low blood pressure or hypoperfusion in the setting of borderline blood pressure values, and the mechanisms of action of levosimendan identify it as a plausible option in this setting.
Evidence for a renal-protective action of levosimendan has been reported from preclinical experiments [51,52,53,54,55]. Improved renal function becomes evident before any increase in cardiac index or left ventricular performance may be detected, suggesting that any renal-protective effect of levosimendan is exerted at least in part via organ-specific effects, including pre-glomerular vasodilation and increased renal artery diameter and renal blood flow, without compromise of renal oxygenation [56, 57]. An interesting hypothesis has been developed to explain those findings: it may be that levosimendan exerts a selective vasodilation on the afferent arterioles of the renal glomeruli thus improving renal filtration both directly and indirectly [51] (Fig. 3).
Scheme of the putative selective effect of levosimendan on afferent glomerular arterioles. Levosimendan exerts predominantly a vasodilation of the afferent arterioles [net effect RBF↑, GFR↑], while dopamine and dobutamine vasodilate both afferent and efferent arterioles [net effect RBF↑↑, GFR↔] (from Yilmaz et al. [51])
This finding is consistent with the observation in the Levosimendan Infusion versus Dobutamine (LIDO) trial [12], in which levosimendan treatment was associated with an increase in GFR, whereas treatment with the active comparator, dobutamine, was not even though it increased cardiac index and urine output. The explanation of that disparity offered by the LIDO authors is that the capacity of levosimendan to promote arterial and venous vasodilation through activation of KATP channels reduces central venous pressure and thus may be beneficial on GFR in some patients.
Further insights into this matter have been provided in recently-reported investigations by Lannemyr, Ricksten, and colleagues in 32 adult patients with chronic heart failure (mean baseline LVEF ~27%) and impaired renal function (mean GFR rate < 80 mL/min per 1.73 m2) [58]. As part of an elective cardiac work-up participants were randomly assigned to short-term (75 min) treatments with either levosimendan (loading dose of 12 mcg/kg over 10 min, then infusion at 0.1 μg/kg/min for 65 mins; n = 16) or dobutamine (continuous infusion started at 5.0 μg/kg/min for 10 mins then 7.5 μg/kg/min for 65 mins; n = 16).
Both treatments were associated with quantitatively and qualitatively very similar alterations in systemic hemodynamic indices, including augmentation of cardiac output and cardiac index, and reductions in systemic vascular resistance index, central venous pressure, and pulmonary capillary wedge pressure. Both treatments also significantly enhanced renal blood flow (levosimendan P < 0.05 vs. baseline; dobutamine P < 0.001 vs. baseline) but only levosimendan therapy was associated with a significant increase in GFR (P < 0.05 vs. baseline: in fact, no alteration in GFR was seen in response to dobutamine, leading to a significant intergroup difference at the end of the treatment phase (P = 0.012; Fig. 4). Filtration fraction was stable during levosimendan treatment but fell in response to dobutamine (P = 0.045 between groups). The authors of this research conjectured that their data are compatible with the hypothesis that levosimendan acts as a vasodilator on afferent renal arterioles, whereas dobutamine dilates both afferent and efferent vessels. They noted also that as both drugs reduced central venous pressure to a similar extent, this affect could not be adduced as the cause of the different treatments’ impact on GFR. Of note, the > 20% increase in GFR observed in patients treated with levosimendan was not accompanied by renal oxygenation as renal oxygen delivery increased in proportion to the increase in GFR. Lannemyr et al. concede that theirs is a study of short-term drug exposure in a small patient cohort: they suggest, nevertheless, that their data question the assumption that all inotropes that have favorable effects on central and peripheral hemodynamics can be assumed also to exert correspondingly favorable effects on renal perfusion and function, and conjecture that levosimendan "could be the preferred inotropic agent for treatment of the cardiorenal syndrome.”
Percentage changes in cardiac index (CI), renal blood flow (RBF), and glomerular filtration rate (GFR) after 75 mins administration of levosimendan or dobutamine. Derived from Lannemyr et al. [58]. (See text for further discussion of dosage and results)
Data on the effects of levosimendan on renal function in various clinical situations including cardiac surgery [34, 37, 59] and critical illness [60] have been collated in and the results suggest a renal-protective effect (Fig. 5). Both in these situations, however, and in heart failure, any such effect requires confirmation in specifically designed prospective trials of adequate statistical power.
Beneficial impact of levosimendan in critically ill patients with or at risk for acute renal failure: a meta-analysis of randomized clinical trials (data from Bove et al. [60])
Conclusions
Levosimendan’s current indication for the short-term treatment of acutely decompensated severe chronic heart failure is based on its unique pharmacological profile as a myocardial sensitizer and KATP channel activator and from experience from an extensive clinical trials program.
Renal dysfunction is very common in HF, and a further worsening of kidney function may be expected during hospitalization for AHF. The treatment of cardiorenal syndrome in decompensated HF is challenging due to variable pathophysiology and lack of specifically tailored therapeutic options. Identifying the underlying processes of kidney dysfunction is essential to successful management. Volume status should be checked whenever possible, as well as hypotension and third space fluid accumulation.
Inotropes may be appropriate for short-term management of AHF with renal dysfunction; especially, in low-output states, they may be particularly indicated to avoid renal hypoperfusion. Levosimendan, both in the acute setting and in the repetitive/intermittent context of AdHF, appears to a promising option to improve renal perfusion or to reverse or ameliorate renal dysfunction, but further controlled trials are needed to confirm the status of levosimendan for this purpose.
The posology of levosimendan in AHF and AdHF is a central consideration, especially when treating patients with associated renal dysfunction: dosing of levosimendan should commence without a bolus, to minimize the risk of hypotension. A continuous 24-h infusion of levosimendan should be administered at a rate of 0.05–0.1 μg/kg/min, while maintaining the patient in euvolemic and eukalemic state.
References
Papp Z, Edes I, Fruhwald S, De Hert SG, Salmenpera M, Leppikangas H, et al. Levosimendan: molecular mechanisms and clinical implications: consensus of experts on the mechanisms of action of levosimendan. Int J Cardiol. 2012;159:82–7.
Pollesello P, Papp Z, Papp JG. Calcium sensitizers: what have we learned over the last 25 years? Int J Cardiol. 2016;203:543–8.
Brixius K, Reicke S, Schwinger RH. Beneficial effects of the Ca(2+) sensitizer levosimendan in human myocardium. Am J Physiol Heart Circ Physiol. 2002 Jan;282(1):H131–7.
Ukkonen H, Saraste M, Akkila J, Knuuti MJ, Lehikoinen P, Någren K, et al. Myocardial efficiency during calcium sensitization with levosimendan: a noninvasive study with positron emission tomography and echocardiography in healthy volunteers. Clin Pharmacol Ther. 1997;61:596–607.
Nieminen MS, Pollesello P, Vajda G, Papp Z. Effects of levosimendan on the energy balance: preclinical and clinical evidence. J Cardiovasc Pharmacol. 2009;53(4):302–10.
Louhelainen M, Vahtola E, Kaheinen P, Leskinen H, Merasto S, Kytö V, et al. Effects of levosimendan on cardiac remodeling and cardiomyocyte apoptosis in hypertensive Dahl/Rapp rats. Br J Pharmacol. 2007;150(7):851–61.
Farmakis D, Alvarez J, Gal TB, Brito D, Fedele F, Fonseca C, et al. Levosimendan beyond inotropy and acute heart failure: evidence of pleiotropic effects on the heart and other organs: an expert panel position paper. Int J Cardiol. 2016;222:303–12.
Nieminen MS, Fruhwald S, Heunks LM, Suominen PK, Gordon AC, Kivikko M, et al. Levosimendan: current data, clinical use and future development. Heart Lung Vessels. 2013;5(4):227–45.
Pollesello P, Parissis J, Kivikko M, Harjola VP. Levosimendan meta-analyses: is there a pattern in the effect on mortality? Int J Cardiol. 2016;209:77–83.
Mebazaa A, Nieminen MS, Packer M, Cohen-Solal A, Kleber FX, Pocock SJ, et al. Levosimendan vs dobutamine for patients with acute decompensated heart failure: the SURVIVE Randomized Trial. JAMA. 2007;297(17):1883–91.
Packer M, Colucci W, Fisher L, Massie BM, Teerlink JR, Young J, et al. Effect of levosimendan on the short-term clinical course of patients with acutely decompensated heart failure. JCHF. 2013;1:103–11.
Follath F, Cleland JG, Just H, Papp JG, Scholz H, Peuhkurinen K, et al. Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low-output heart failure (the LIDO study): a randomised double-blind trial. Lancet. 2002;360:196–202.
Moiseyev VS, Põder P, Andrejevs N, Ruda MY, Golikov AP, Lazebnik LB, et al. Safety and efficacy of a novel calcium sensitizer, levosimendan, in patients with left ventricular failure due to an acute myocardial infarction. A randomized, placebo-controlled, double-blind study (RUSSLAN). Eur Heart J. 2002;23(18):1422–32.
Mebazaa A, Parissis J, Porcher R, Gayat E, Nikolaou M, Boas FV, et al. Short-term survival by treatment among patients hospitalized with acute heart failure: the global ALARM-HF registry using propensity scoring methods. Intensive Care Med. 2011;37(2):290–301.
Bonjos MJ, Terrovitis JV, Drakos SG, Katsaros F, Pantsios C, Nanas SN, et al. Comparison of three different regimens of intermittent inotrope infusions for end stage heart failure. Int J Cardiol. 2012;159(3):225–9.
Flevari P, Parissis JT, Leftheriotis D, Panou F, Kourea K, Kremastinos DT. Effect of levosimendan on ventricular arrhythmias and prognostic autonomic indexes in patients with decompensated advanced heart failure secondary to ischemic or dilated cardiomyopathy. Am J Cardiol. 2006;98(12):1641–5.
Fuhrmann JT, Schmeisser A, Schulze MR, Wunderlich C, Schoen SP, Rauwolf T, et al. Levosimendan is superior to enoximone in refractory cardiogenic shock complicating acute myocardial infarction. Crit Care Med. 2008;36(8):2257–66.
Hou ZQ, Sun ZX, Su CY, Tan H, Zhong X, Hu B, et al. Effect of levosimendan on estimated glomerular filtration rate in hospitalized patients with decompensated heart failure and renal dysfunction. Cardiovasc Ther. 2013;31(2):108–14.
Malfatto G, Della Rosa F, Villani A, Rella V, Branzi G, Facchini M, et al. Intermittent levosimendan infusions in advanced heart failure: favourable effects on left ventricular function, neurohormonal balance, and one-year survival. J Cardiovasc Pharmacol. 2012;60(5):450–5.
Moertl D, Berger R, Huelsmann M, Bojic A, Pacher R. Short-term effects of levosimendan and prostaglandin E1 on hemodynamic parameters and B-type natriuretic peptide levels in patients with decompensated chronic heart failure. Eur J Heart Fail. 2005;7(7):1156–63.
Slawsky MT, Colucci WS, Gottlieb SS, Greenberg BH, Haeusslein E, Hare J, et al. Acute hemodynamic and clinical effects of levosimendan in patients with severe heart failure. Study Investigators. Circulation. 2000;102:2222–7.
Nieminen MS, Akkila J, Hasenfuss G, Kleber FX, Lehtonen LA, Mitrovic V, et al. Hemodynamic and neurohumoral effects of continuous infusion of levosimendan in patients with congestive heart failure. J Am Coll Cardiol. 2000;36:1903–12.
Lilleberg J, Nieminen MS, Akkila J, Heikkila L, Kuitunen A, Lehtonen L, et al. Effects of a new calcium sensitizer, levosimendan, on haemodynamics, coronary blood flow and myocardial substrate utilization early after coronary artery bypass grafting. Eur Heart J. 1998;19:660–8.
Ukkonen H, Saraste M, Akkila J, Knuuti J, Karanko M, Iida H, et al. Myocardial efficiency during levosimendan infusion in congestive heart failure. Clin Pharmacol Ther. 2000;68:522–31.
Lilleberg J, Laine M, Palkama T, Kivikko M, Pohjanjousi P, Kupari M. Duration of the haemodynamic action of a 24-h infusion of levosimendan in patients with congestive heart failure. Eur J Heart Fail. 2007;9:75–82.
Kivikko M, Lehtonen L, Colucci WS. Sustained hemodynamic effects of intravenous levosimendan. Circulation. 2003;107:81–6.
Mebazaa A, Nieminen MS, Filippatos GS, Cleland JG, Salon JE, Thakkar R, et al. Levosimendan vs. dobutamine: outcomes for acute heart failure patients on beta-blockers in SURVIVE. Eur J Heart Fail. 2009;11:304–11.
Sonntag S, Sundberg S, Lehtonen LA, Kleber FX. The calcium sensitizer levosimendan improves the function of stunned myocardium after percutaneous transluminal coronary angioplasty in acute myocardial ischemia. J Am Coll Cardiol. 2004;43:2177–82.
Givertz MM, Andreou C, Conrad CH, Colucci WS. Direct myocardial effects of levosimendan in humans with left ventricular dysfunction: alteration of force-frequency and relaxation-frequency relationships. Circulation. 2007;115:1218–24.
Nieminen MS, Altenberger J, Ben-Gal T, Böhmer A, Comin-Colet J, Dickstein K, et al. Repetitive use of levosimendan for treatment of chronic advanced heart failure: clinical evidence, practical considerations, and perspectives: an expert panel consensus. Int J Cardiol. 2014;174:360–7.
Altenberger J, Parissis JT, Costard-Jaeckle A, Winter A, Ebner C, Karavidas A, et al. Efficacy and safety of the pulsed infusions of levosimendan in outpatients with advanced heart failure (LevoRep) study: a multicentre randomized trial. Eur J Heart Fail. 2014;16(8):898–906.
Comín-Colet J, Manito N, Segovia-Cubero J, Delgado J, García Pinilla JM, Almenar L, et al. Efficacy and safety of intermittent intravenous outpatient administration of levosimendan in patients with advanced heart failure: the LION-HEART multicentre randomised trial. Eur J Heart Fail. 2018;20:1128–36.
Pölzl G, Altenberger J, Baholli L, Beltrán P, Borbély A, Comin-Colet J, et al. Repetitive use of levosimendan in advanced heart failure: need for stronger evidence in a field in dire need of a useful therapy. Int J Cardiol. 2017;243:389–95.
Sanfilippo F, Knight JB, Scolletta S, Santonocito C, Pastore F, Lorini FL, et al. Levosimendan for patients with severely reduced left ventricular systolic function and/or low cardiac output syndrome undergoing cardiac surgery: a systematic review and meta-analysis. Crit Care. 2017;21(1):252.
Silvetti S, Nieminen MS. Repeated or intermittent levosimendan treatment in advanced heart failure: an updated meta-analysis. Int J Cardiol. 2016;202:138–43.
Gong B, Li Z, Yat Wong PC. Levosimendan treatment for heart failure: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2015;29(6):1415–25.
Putzu A, Clivio S, Belletti A, Cassina T. Perioperative levosimendan in cardiac surgery: a systematic review with meta-analysis and trial sequential analysis. Int J Cardiol. 2018;251:22–31.
Koster G, Wetterslev J, Gluud C, Zijlstra JG, Scheeren TW, van der Horst IC, et al. Effects of levosimendan for low cardiac output syndrome in critically ill patients: systematic review with meta-analysis and trial sequential analysis. Intensive Care Med. 2015;41(2):203–21.
Zangrillo A, Biondi-Zoccai G, Ponschab M, Greco M, Corno L, Covello RD, et al. Milrinone and mortality in adult cardiac surgery: a meta-analysis. J Cardiothorac Vasc Anesth. 2012;26(1):70–7.
Tacon CL, McCaffrey J, Delaney A. Dobutamine for patients with severe heart failure: a systematic review and meta-analysis of randomised controlled trials. Intensive Care Med. 2012;38(3):359–67.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Crespo-Leiro MG, Metra M, Lund LH, Milicic D, Costanzo MR, Filippatos G, et al. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018.
Silvetti S, Belletti A, Fontana A, Pollesello P. Rehospitalization after intermittent levosimendan treatment in advanced heart failure patients: a meta-analysis of randomized trials. ESC Heart Fail. 2017;4(4):595–604.
Xanthakis V, Enserro DM, Larson MG, Wollert KC, Januzzi JL, Levy D, et al. Prevalence, neurohormonal correlates, and prognosis of heart failure stages in the community. JACC Heart Fail. 2016;4:808–15.
Bjork JB, Alton KK, Georgiopoulou VV, Butler J, Kalogeropoulos AP. Defining advanced heart failure: a systematic review of criteria used in clinical trials. J Card Fail. 2016;22:569–77.
Fang JC, Ewald GA, Allen LA, Butler J, Westlake Canary CA, Colvin-Adams M, et al. Advanced (stage D) heart failure: a statement from the Heart Failure Society of America Guidelines Committee. J Card Fail. 2015;21:519–34.
Nieminen MS, Buerke M, Cohen-Solál A, Costa S, Édes I, Erlikh A, et al. The role of levosimendan in acute heart failure complicating acute coronary syndrome: a review and expert consensus opinion. Int J Cardiol. 2016;218:150–7.
Salzman HE, Sharma K, Mather PJ, Rubin S, Adams S, Whellan DJ. Renal dysfunction in heart failure patients: what is the evidence? Heart Fail Rev. 2007;12:37–47.
Mahon NG, Blackstone EH, Francis GS, Starling RC 3rd, Young JB, Lauer MS. The prognostic value of estimated creatinine clearance alongside functional capacity in ambulatory patients with chronic congestive heart failure. J Am Coll Cardiol. 2002;40(6):1106–13.
Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52:1527–39.
Yilmaz MB, Grossini E, Silva Cardoso JC, Édes I, Fedele F, Pollesello P, et al. Renal effects of levosimendan: a consensus report. Cardiovasc Drugs Ther. 2013;27(6):581–90.
Pagel PS, Hettrick DA, Warltier DC. Influence of levosimendan, pimobendan, and milrinone on the regional distribution of cardiac output in anaesthetized dogs. Br J Pharmacol. 1996;119(3):609–15.
Zager RA, Johnson AC, Lund S, Hanson SY, Abrass CK. Levosimendan protects against experimental endotoxemic acute renal failure. Am J Physiol Renal Physiol. 2006;290(6):F1453–62.
Rehberg S, Ertmer C, Vincent JL, Spiegel HU, Köhler G, Erren M, et al. Effects of combined arginine vasopressin and levosimendan on organ function in ovine septic shock. Crit Care Med. 2010;38(10):2016–23.
Grossini E, Molinari C, Pollesello P, Bellomo G, Valente G, Mary D, et al. Levosimendan protection against kidney ischemia/reperfusion injuries in anesthetized pigs. J Pharmacol Exp Ther. 2012;342(2):376–88.
Bragadottir G, Redfors B, Ricksten SE. Effects of levosimendan on glomerular filtration rate, renal blood flow, and renal oxygenation after cardiac surgery with cardiopulmonary bypass: a randomized placebo-controlled study. Crit Care Med. 2013;41(10):2328–35.
Fedele F, Bruno N, Brasolin B, Caira C, D'Ambrosi A, Mancone M. Levosimendan improves renal function in acute decompensated heart failure: possible underlying mechanisms. Eur J Heart Fail. 2014;16(3):281–8.
Lannemyr L, Ricksten S-E, Rundqvist B, Andersson B, Bartfay S-E, Ljungman C, et al. Differential effects of levosimendan and dobutamine on glomerular filtration rate in patients with heart failure and renal impairment: a randomized double-blind controlled trial. J Am Heart Assoc. 2018;7:e008455.
Niu ZZ, Wu SM, Sun WY, Hou WM, Chi YF. Perioperative levosimendan therapy is associated with a lower incidence of acute kidney injury after cardiac surgery: a meta-analysis. J Cardiovasc Pharmacol. 2014;63(2):107–12.
Bove T, Matteazzi A, Belletti A, Paternoster G, Saleh O, Taddeo D, et al. Beneficial impact of levosimendan in critically ill patients with or at risk for acute renal failure: a meta-analysis of randomized clinical trials. Heart Lung Vessel. 2015;7(1):35–46.
Funding
This project did not receive any financial support, apart from logistic expenses related to the organization of the hands-on tutorials at the Heart Failure Association of the European Society of Cardiology annual meeting in Vienna on April May 27–28, 2018, which were covered by an unrestricted educational grant by Orion Pharma. The lecturers and the program were approved by the Heart Failure Association. Orion Pharma follows the EFPIA HCP CODE.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Medical Writing, Editorial, and Other Assistance
Editorial assistance in the preparation of this article was provided by Peter Hughes (Hughes associates, Oxford, UK).
Conflict of Interest
P. Pollesello and M. Kivikko are full-time employees of Orion Pharma. The other authors report no conflicts of interest apart for the lecture honoraria related to the aforementioned educational event.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bouchez, S., Fedele, F., Giannakoulas, G. et al. Levosimendan in Acute and Advanced Heart Failure: an Expert Perspective on Posology and Therapeutic Application. Cardiovasc Drugs Ther 32, 617–624 (2018). https://doi.org/10.1007/s10557-018-6838-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-018-6838-2