Abstract
Background
Racial and socio-economic status (SES) disparities exist in prostate cancer (PrCA) incidence and mortality. Less is known regarding how geographical factors, including neighborhood social vulnerability and distance traveled to receive care, affect PrCA risk. The purpose of this research was to use the Veterans Administration Medical System, which provides a unique means for studying PrCA epidemiology among diverse individuals with ostensibly equal access to healthcare, to determine whether area-level characteristics influence PrCA incidence while accounting for individual-level risk factors.
Methods
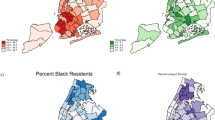
From the US Veteran’s Health Administration (VHA) electronic medical records (EMR) database from January 1999 to December 2015, we identified 3,736 PrCA patients and 104,017 cancer-free controls from South Carolina (SC). The VHA EMRs were linked to the US census which provided area-level factors. US census data were used to construct the Social Vulnerability Index which is a continuous composite measure of area-level vulnerability and was divided into tertiles for modeling purposes. Data were analyzed using a Bayesian multivariate conditional autoregressive model (CAR) which accounted for individual-level factors, area-level factors, spatial random effects, and autocorrelation, which were used to identify areas of higher- or lower-than-expected PrCA incidence after controlling for risk factors.
Results
As expected, after accounting for age (sixfold and 13-fold increases in men 40–50 years and > 50 years, respectively), race was an important risk factor, with threefold higher odds among Blacks in the fully adjusted model [ORadj 2.98 (2.77, 3.20)]. After accounting for all other factors, residing in a ZIP code tabulated areas (ZCTA) with the greatest level social vulnerability versus the lowest, least vulnerable ZCTA’s, increased PrCA risk by 39% [ORadj 1.39 (1.11, 1.75)].
Conclusions
While accounting for known risk factors for PrCA, including age, race, and marital status, we found geographic areas in SC characterized by higher than average social vulnerability with higher rates of incident PrCA among veterans. Outreach for screening, education, and care coordination may be needed for veterans in these areas.

Similar content being viewed by others
References
Siegel RL, Miller KD (2018) Jemal A (2018) Cancer statistics. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Adami H-O, Hunter DJ, Trichopoulos D (2008) Textbook of cancer epidemiology. Monographs in epidemiology and biostatistics, 2nd ed. vol 36. Oxford University Press, Oxford, New York
Clegg LX, Reichman ME, Miller BA, Hankey BF, Singh GK, Lin YD, Goodman MT, Lynch CF, Schwartz SM, Chen VW, Bernstein L, Gomez SL, Graff JJ, Lin CC, Johnson NJ, Edwards BK (2009) Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control 20(4):417–435. https://doi.org/10.1007/s10552-008-9256-0
Hebert JR, Hurley TG, Olendzki BC, Teas J, Ma Y, Hampl JS (1998) Nutritional and socioeconomic factors in relation to prostate cancer mortality: a cross-national study. J Natl Cancer Inst 90(21):1637–1647. https://doi.org/10.1093/jnci/90.21.1637
McMahon DM, Burch JB, Hebert JR, Hardin JW, Zhang J, Wirth MD, Youngstedt SD, Shivappa N, Jacobsen SJ, Caan B, Van Den Eeden SK (2019) Diet-related inflammation and risk of prostate cancer in the California Men's Health Study. Ann Epidemiol 29:30–38. https://doi.org/10.1016/j.annepidem.2018.10.008
Mohseni R, Abbasi S, Mohseni F, Rahimi F, Alizadeh S (2019) Association between dietary inflammatory index and the risk of prostate cancer: a meta-analysis. Nutr Cancer 71(3):359–366. https://doi.org/10.1080/01635581.2018.1516787
Prostate Cancer in the United States in (2015) by State. Interactive Cancer Atlas, CDC
Klassen AC, Curriero FC, Hong JH, Williams C, Kulldorff M, Meissner HI, Alberg A, Ensminger M (2004) The role of area-level influences on prostate cancer grade and stage at diagnosis. Prev Med 39(3):441–448. https://doi.org/10.1016/j.ypmed.2004.04.031
Oliver MN, Smith E, Siadaty M, Hauck FR, Pickle LW (2006) Spatial analysis of prostate cancer incidence and race in Virginia, 1990–1999. Am J Prev Med 30(2 Suppl):S67–S76. https://doi.org/10.1016/j.amepre.2005.09.008
Xiao H, Gwede CK, Kiros G, Milla K (2007) Analysis of prostate cancer incidence using geographic information system and multilevel modeling. J Natl Med Assoc 99(3):218–225
National Center for Health Statistics (U.S.) (2012) Healthy people 2010: final review. DHHS publication, vol no (PHS) 2012–1038. U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, Hyattsville
DeChello LM, Gregorio DI, Samociuk H (2006) Race-specific geography of prostate cancer incidence. Int J Health Geogr 5:59. https://doi.org/10.1186/1476-072X-5-59
Hebert JR, Daguise VG, Hurley DM, Wilkerson RC, Mosley CM, Adams SA, Puett R, Burch JB, Steck SE, Bolick-Aldrich SW (2009) Mapping cancer mortality-to-incidence ratios to illustrate racial and sex disparities in a high-risk population. Cancer 115(11):2539–2552. https://doi.org/10.1002/cncr.24270
Hsu CE, Mas FS, Miller JA, Nkhoma ET (2007) A spatial-temporal approach to surveillance of prostate cancer disparities in population subgroups. J Natl Med Assoc 99(1):72–80
Wagner SE, Bauer SE, Bayakly AR, Vena JE (2013) Prostate cancer incidence and tumor severity in Georgia: descriptive epidemiology, racial disparity, and geographic trends. Cancer Causes Control 24(1):153–166. https://doi.org/10.1007/s10552-012-0101-0
Wagner SE, Hurley DM, Hebert JR, McNamara C, Bayakly AR, Vena JE (2012) Cancer mortality-to-incidence ratios in Georgia: describing racial cancer disparities and potential geographic determinants. Cancer 118(16):4032–4045. https://doi.org/10.1002/cncr.26728
Goovaerts P, Xiao H (2011) Geographical, temporal and racial disparities in late-stage prostate cancer incidence across Florida: a multiscale joinpoint regression analysis. Int J Health Geogr 10:63. https://doi.org/10.1186/1476-072X-10-63
Goovaerts P, Xiao H (2012) The impact of place and time on the proportion of late-stage diagnosis: the case of prostate cancer in Florida, 1981–2007. Spat Spatio-temporal Epidemiol 3(3):243–253. https://doi.org/10.1016/j.sste.2012.03.001
Zhou H, Lawson AB, Hebert JR, Slate EH, Hill EG (2008) A Bayesian hierarchical modeling approach for studying the factors affecting the stage at diagnosis of prostate cancer. Stat Med 27(9):1468–1489. https://doi.org/10.1002/sim.3024
Zhou H, Lawson AB, Hebert JR, Slate EH, Hill EG (2008) Joint spatial survival modeling for the age at diagnosis and the vital outcome of prostate cancer. Stat Med 27(18):3612–3628. https://doi.org/10.1002/sim.3232
Waller LA, Gotway CA (2004) Applied spatial statistics for public health data. Wiley series in probability and statistics, Wiley, Hoboken
Prostate Cancer in the United States in 2011–2015 by State. Interactive Cancer Atlas. CDC
ZIP Code™ Tabulation Areas (ZCTAs™). US Department of Commerce. https://www.census.gov/geo/reference/zctas.html
Department of Veterans Affairs. VA Medical SAS® Files (121VA10P2). VA Corporate Data Center Operations, Austin Information Technology Center, Austin
Department of Veterans Affairs. VA Vital Status File (121VA10P2). VA Corporate Data Center Operations, Austin Information Technology Center, Austin
United States Census Bureau. 2010 Census.U.S. Census Bureau. 2010. https://www2.census.gov/census_2010/. Accessed Aug 2014
United States Census Bureau. 2011 Five Year American Community Survey.U.S. Census Bureau. 2011. https://www2.census.gov/acs2011_5yr/. Accessed Aug 2014
United States Census Bureau. TIGER/Line® Shapefiles. https://www.census.gov/cgi-bin/geo/shapefiles/index.php. Accessed Aug 2014
Cutter SL, Boruff BJ, Shirley WL (2003) Social vulnerability to environmental hazards. Soc Sci Q. https://doi.org/10.1111/1540-6237.8402002
Schmidtlein MC, Deutsch RC, Piegorsch WW, Cutter SL (2008) A sensitivity analysis of the social vulnerability index. Risk Anal 28(4):1099–1114. https://doi.org/10.1111/j.1539-6924.2008.01072.x
SAS 9.4. SAS Institute Inc., Cary
Kleinbaum DG, Kupper LL, Nizam A, Rosenberg ES (2013) Applied regression analysis and other multivariable methods, 5th edn. Cengage Learning, Boston
Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, Rastam L, Larsen K (2006) A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health 60(4):290–297. https://doi.org/10.1136/jech.2004.029454
Geweke J (1992) Evaluating the accuracy of sampling‐based approaches to the calculation of posterior moments. In Paper presented at the Bayesian Statistics, vol 4
Lunn D (2013) The BUGS book: a practical introduction to Bayesian analysis. texts in statistical science. CRC Press/Taylor & Francis Group, Boca Raton
Development Core Team R (2010) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Penchansky R, Thomas JW (1981) The concept of access: definition and relationship to consumer satisfaction. Med Care 19(2):127–140
Delamater PL, Messina JP, Shortridge AM, Grady SC (2012) Measuring geographic access to health care: raster and network-based methods. Int J Health Geogr 11(1):15. https://doi.org/10.1186/1476-072X-11-15
Obertova Z, Brown C, Holmes M, Lawrenson R (2012) Prostate cancer incidence and mortality in rural men—a systematic review of the literature. Rural Remote Health 12(2):2039
WWAMI Rural Health Research Center. https://depts.washington.edu/uwruca/
Cheng I, Witte JS, McClure LA, Shema SJ, Cockburn MG, John EM, Clarke CA (2009) Socioeconomic status and prostate cancer incidence and mortality rates among the diverse population of California. Cancer Causes Control 20(8):1431–1440. https://doi.org/10.1007/s10552-009-9369-0
Gilligan T (2005) Social disparities and prostate cancer: mapping the gaps in our knowledge. Cancer Causes Control 16(1):45–53. https://doi.org/10.1007/s10552-004-1291-x
Coker AL, Sanderson M, Ellison GL, Fadden MK (2006) Stress, coping, social support, and prostate cancer risk among older African American and Caucasian men. Ethn Dis 16(4):978–987
Newell GR, Pollack ES, Spitz MR, Sider JG, Fueger JJ (1987) Incidence of prostate cancer and marital status. J Natl Cancer Inst 79(2):259–262
Tyson MD, Andrews PE, Etzioni DA, Ferrigni RG, Humphreys MR, Swanson SK, Castle EK (2013) Marital status and prostate cancer outcomes. Can J Urol 20(2):6702–6706
Hersh WR, Weiner MG, Embi PJ, Logan JR, Payne PR, Bernstam EV, Lehmann HP, Hripcsak G, Hartzog TH, Cimino JJ, Saltz JH (2013) Caveats for the use of operational electronic health record data in comparative effectiveness research. Med Care 51(8 Suppl 3):S30–S37. https://doi.org/10.1097/MLR.0b013e31829b1dbd
Rao GA, Mann JR, Bottai M, Uemura H, Burch JB, Bennett CL, Haddock KS, Hebert JR (2013) Angiotensin receptor blockers and risk of prostate cancer among United States veterans. J Clin Pharmacol 53(7):773–778. https://doi.org/10.1002/jcph.98
Rao GA, Mann JR, Shoaibi A, Bennett CL, Nahhas G, Sutton SS, Jacob S, Strayer SM (2014) Azithromycin and levofloxacin use and increased risk of cardiac arrhythmia and death. Ann Fam Med 12(2):121–127. https://doi.org/10.1370/afm.1601
Rao GA, Mann JR, Shoaibi A, Pai SG, Bottai M, Sutton SS, Haddock KS, Bennett CL, Hebert JR (2013) Angiotensin receptor blockers: are they related to lung cancer? J Hypertens 31(8):1669–1675. https://doi.org/10.1097/HJH.0b013e3283621ea3
Shoaibi A, Rao GA, Cai B, Rawl J, Haddock KS, Hebert JR (2017) Prostate specific antigen-growth curve model to predict high-risk prostate cancer. Prostate 77(2):173–184. https://doi.org/10.1002/pros.23258
Grubesic TH, Matisziw TC (2006) On the use of ZIP codes and ZIP code tabulation areas (ZCTAs) for the spatial analysis of epidemiological data. Int J Health Geogr 5:58. https://doi.org/10.1186/1476-072X-5-58
United States. Congress. Senate. Committee on Labor and Human Resources. (1998) Health Insurance Portability and Accountability Act of 1996, first-year implementation concerns: hearing before the Committee on Labor and Human Resources, United States Senate, One Hundred Fifth Congress, second session … 19 March 1998. S hrg, vol 105–490. U.S. G.P.O.: For sale by the U.S. G.P.O., Supt. of Docs., Congressional Sales Office, Washington
United States. Congress (104th 2nd session: 1996) (1996) Health Insurance Portability and Accountability Act of 1996: conference report (to accompany H.R. 3103). Report/104th Congress, 2nd session, House of Representatives 104-736. U.S. G.P.O., Washington
Cutter SL, Finch C (2008) Temporal and spatial changes in social vulnerability to natural hazards. Proc Natl Acad Sci USA 105(7):2301–2306. https://doi.org/10.1073/pnas.0710375105
Fryar CD, Herrick K, Afful J, Ogden CL (2016) Cardiovascular disease risk factors among male veterans, U.S., 2009–2012. Am J Prev Med 50 (1):101–105. https://doi.org/10.1016/j.amepre.2015.06.011
Liu Y, Sayam S, Shao X, Wang K, Zheng S, Li Y, Wang L (2017) Prevalence of and trends in diabetes among veterans, United States, 2005–2014. Prev Chronic Dis 14:E135. https://doi.org/10.5888/pcd14.170230
Funding
None.
Author information
Authors and Affiliations
Contributions
PG developed the study idea under the mentorship of JME, BO, GR, CLB, and JRH. PG obtained, managed, cleaned, and analyzed the data. PG drafted the manuscript and was responsible for incorporating and resolving all manuscript edits and comments. JRH and JME guided PG through all epidemiological aspects of the study. BO guided PG through all biostatistical aspects of the study. GR guided PG in acquiring and cleaning the data. CLB guided PG through all clinical considerations of the study. CE guided PG in developing the Social Vulnerability Index for ZIP code tabulated areas. KSH guided PG through all required Department of Veteran’s Affairs requirements necessary to conduct a study using Veteran Health Administration data. JRH provided PG guidance in overseeing and managing all aspects of this study. JME, BO, GR, CLB, CE, KSH, and JRH reviewed, edited, and commented on all drafts of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Georgantopoulos, P., Eberth, J.M., Cai, B. et al. Patient- and area-level predictors of prostate cancer among South Carolina veterans: a spatial analysis. Cancer Causes Control 31, 209–220 (2020). https://doi.org/10.1007/s10552-019-01263-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-019-01263-2