Abstract
Background
A better understanding underlying radiation (RT) response after breast-conserving surgery (BCS) is needed to mitigate over-treatment of DCIS. The hazard ratio (HR) measures the effect of RT but assumes the effect is constant over time. We examined the hazard function adjusted for adherence to surveillance mammography to examine variations in LR risk and the effect of RT over time.
Methods
Crude hazard estimates for the development of LR in a population cohort of DCIS treated by BCS ± RT were computed. Multivariable extended Cox models and hazard plots were used to examine the association between receipt of RT and risk of each outcome adjusted for baseline covariates and adherence to mammography.
Results
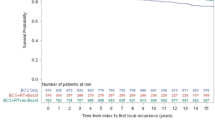
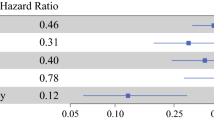
Population cohort includes 3262 women treated by BCS; 1635 received RT. Median follow-up was 13 years. LR developed in 364 women treated by BCS alone and 274 treated with RT. LR risk peaked at 2 years, declined until year 7, and then remained steady. The peak hazard of LR was associated with adverse features of DCIS. Early LR risk was attenuated in patients treated with RT but late annual risks of LR and invasive LR were similar among the two treatment groups. On multivariate analysis, RT was associated with a reduction in early LR risk (HR = 0.52, 95% CI 0.43–0.63, p < 0.0001) but did not reduce the risk of late LR (HR = 0.89, 95% CI: 0.67, 1.19, p = 0.44) (interaction, p = 0.002).
Conclusions
The effect of RT is not uniform over time and greatest in the first 7 years after BCS for DCIS, which can guide future research to understand mechanisms underlying RT response and optimize future management of DCIS.




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), Correa C, McGale P, Taylor C, Wang Y, Clarke M, Davies C, Peto R, Bijker N, Solin L et al (2010) Overview of the randomized trials of radiotherapy in ductal carcinoma in situ of the breast. J Natl Cancer Inst Monogr 10(41):162–177
Sagara Y, Freedman RA, Vaz-Luis I, Mallory MA, Wong SM, Aydogan F, DeSantis S, Barry WT, Golshan M (2016) Patient prognostic score and associations with survival improvement offered by radiotherapy after breast-conserving surgery for ductal carcinoma in situ: a population-based longitudinal cohort study. J Clin Oncol 34(11):1190–1196
Rakovitch E, Nofech-Mozes S, Hanna W, Sutradhar R, Baehner FL, Miller DP, Fong C, Gu S, Tuck A, Sengupta S et al (2017) Multigene expression assay and benefit of radiotherapy after breast conservation in ductal carcinoma in situ. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djw256
Bremer T, Whitworth P, Patel R, Savala J, Barry T, Lyle S, Leesman G, Linke SP, Jirstrom K, Zhou W et al (2018) A biologic signature for breast ductal carcinoma in situ to predict radiation therapy (RT) benefit and assess recurrence risk. Clin Cancer Res 24(23):5895–5901
Sedgwick P, Joekes K (2015) Interpreting hazard ratios. BMJ 351:h4631
Cheng L, Swartz MD, Zhao H, Kapadia AS, Lai D, Rowan PJ, Buchholz TA, Giordano SH (2012) Hazard of recurrence among women after primary breast cancer treatment—a 10-year follow-up using data from SEER-Medicare. Cancer Epidemiol Biomarkers Prev 21(5):800–809
Dignam JJ, Dukic V, Anderson SJ, Mamounas EP, Wickerham DL, Wolmark N (2009) Hazard of recurrence and adjuvant treatment effects over time in lymph node-negative breast cancer. Breast Cancer Res Treat 116(3):595–602
Warnberg F, Garmo H, Emdin S, Hedberg V, Adwall L, Sandelin K, Ringberg A, Karlsson P, Arnesson LG, Anderson H et al (2014) Effect of radiotherapy after breast-conserving surgery for ductal carcinoma in situ: 20 years follow-up in the randomized SweDCIS Trial. J Clin Oncol 32(32):3613–3618
Donker M, Litiere S, Werutsky G, Julien JP, Fentiman IS, Agresti R, Rouanet P, de Lara CT, Bartelink H, Duez N et al (2013) Breast-conserving treatment with or without radiotherapy in ductal carcinoma in situ: 15-year recurrence rates and outcome after a recurrence, from the EORTC 10853 randomized phase III trial. J Clin Oncol 31(32):4054–4059
Wapnir IL, Dignam JJ, Fisher B, Mamounas EP, Anderson SJ, Julian TB, Land SR, Margolese RG, Swain SM, Costantino JP et al (2011) Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst 103(6):478–488
Rakovitch E, Nofech-Mozes S, Narod S, Hanna W, Thiruchelvam D, Saskin R, Taylor C, Tuck A, Sengupta S, Elavathil L et al (2013) Can we select individuals with low risk ductal carcinoma in situ (DCIS)? A population-based outcomes analysis. Breast Cancer Res Treat 138(2):581–590
Allison PD (2010) Survival analysis using SAS: a practical guide. SAS Press, Cary
Therneau TM, Grambsch PM (2000) Modeling survival data: extending the cox model. Springer, New York
Ratanawichitrasin A, Rybicki LA, Steiger E, Grundfest-Broniatowski S, Hermann RE, Crowe JP (1999) Predicting the likelihood of residual disease in women treated for ductal carcinoma in situ. J Am Coll Surg 188(1):17–21
Sprague BL, Vacek PM, Herschorn SD, James TA, Geller BM, Trentham-Dietz A, Stein JL, Weaver DL (2018) Time-varying risks of second events following a DCIS diagnosis in the population-based Vermont DCIS cohort. Breast Cancer Res Treat 174(1):227–235
Enderling H, Anderson AR, Chaplain MA, Munro AJ, Vaidya JS (2006) Mathematical modelling of radiotherapy strategies for early breast cancer. J Theor Biol 241(1):158–171
Acknowledgements
The authors would like to acknowledge the assistance of C. Fong and S. Trebinjac in the preparation and submission of this manuscript. This study was supported by the ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. These datasets were linked using unique encoded identifiers and analyzed at the ICES. Parts of this material are based on data and/or information compiled and provided by CIHI. However, the analyses, conclusions, opinions, and statements expressed in the material are those of the author(s), and not necessarily those of CIHI. Parts of this material are based on data and information provided by Cancer Care Ontario (CCO). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of CCO. No endorsement by CCO is intended or should be inferred.
Funding
This work was supported in part by a grant from the Canadian Cancer Society Research Institute (Grant Number 18491). Dr. Rakovitch holds the LC Campbell Breast Cancer Research Chair.
Author information
Authors and Affiliations
Contributions
All authors contributed to the interpretation of the analysis and manuscript preparation.
Corresponding author
Ethics declarations
Conflicts of interest
ERakovitch has received research grant funding from Genomic Health Inc. A Thompson has received lecture honoraria from Pfizer outside of this work. T Whelan has received other research grant funding from Genomic Health Inc. All other authors declare no conflict of interest.
Ethical approval
Ethical approval was obtained from Sunnybrook Health Sciences Centre.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rakovitch, E., Sutradhar, R., Hallett, M. et al. The time-varying effect of radiotherapy after breast-conserving surgery for DCIS. Breast Cancer Res Treat 178, 221–230 (2019). https://doi.org/10.1007/s10549-019-05377-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05377-8