Abstract
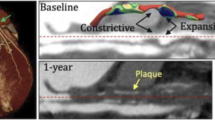
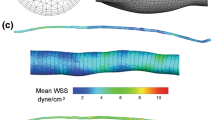
Coronary artery bypass graft surgery is a common intervention for coronary artery disease; however, it suffers from graft failure, and the underlying mechanisms are not fully understood. To better understand the relation between graft hemodynamics and surgical outcomes, we performed computational fluid dynamics simulations with deformable vessel walls in 10 study participants (24 bypass grafts) based on CT and 4D flow MRI one month after surgery to quantify lumen diameter, wall shear stress (WSS), and related hemodynamic measures. A second CT acquisition was performed one year after surgery to quantify lumen remodeling. Compared to venous grafts, left internal mammary artery grafts experienced lower abnormal WSS (< 1 Pa) area one month after surgery (13.8 vs. 70.1%, p = 0.001) and less inward lumen remodeling one year after surgery (− 2.4% vs. − 16.1%, p = 0.027). Abnormal WSS area one month post surgery correlated with percent change in graft lumen diameter one year post surgery (p = 0.030). This study shows for the first time prospectively a correlation between abnormal WSS area one month post surgery and graft lumen remodeling 1 year post surgery, suggesting that shear-related mechanisms may play a role in post-operative graft remodeling and might help explain differences in failure rates between arterial and venous grafts.






Similar content being viewed by others
Abbreviations
- CABG:
-
Coronary artery bypass graft
- CFD:
-
Computational fluid dynamics
- CT:
-
Computed tomography
- LIMA:
-
Left internal mammary artery
- MRI:
-
Magnetic resonance imaging
- RA:
-
Radial artery
- SVG:
-
Saphenous vein graft
- WSS:
-
Wall shear stress
References
Antiga, L., M. Piccinelli, L. Botti, B. Ene-Iordache, A. Remuzzi, and D. A. Steinman. An image-based modeling framework for patient-specific computational hemodynamics. Med. Biol. Eng. Comput. 46:1097, 2008.
Davies, P. F. Hemodynamic shear stress and the endothelium in cardiovascular pathophysiology. Nat. Clin. Pract. Cardiovasc. Med. 6:16–26, 2009.
de Graaf, F. R., J. E. van Velzen, A. J. Witkowska, J. D. Schuijf, N. van der Bijl, L. J. Kroft, A. de Roos, J. H. C. Reiber, J. J. Bax, G. J. de Grooth, J. W. Jukema, and E. E. van der Wall. Diagnostic performance of 320-slice multidetector computed tomography coronary angiography in patients after coronary artery bypass grafting. Eur. Radiol. 21:2285–2296, 2011.
Eslami, P., J. Tran, Z. Jin, J. Karady, R. Sotoodeh, M. T. Lu, U. Hoffmann, and A. Marsden. Effect of wall elasticity on hemodynamics and wall shear stress in patient-specific simulations in the coronary arteries. J. Biomech. Eng. 2019. https://doi.org/10.1115/1.4043722.
Figard, S. Introduction to Biostatistics with JMP. SAS Institute, 2019, 288 pp.at <https://books.google.com/books/about/Introduction_to_Biostatistics_with_JMP.html?id=0ZRMygEACAAJ>
Figueroa, C. A., I. E. Vignon-Clementel, K. E. Jansen, T. J. R. Hughes, and C. A. Taylor. A coupled momentum method for modeling blood flow in three-dimensional deformable arteries. Comput. Methods Appl. Mech. Eng. 195:5685–5706, 2006.
Gallo, D., G. De Santis, F. Negri, D. Tresoldi, R. Ponzini, D. Massai, M. A. Deriu, P. Segers, B. Verhegghe, G. Rizzo, and U. Morbiducci. On the use of in vivo measured flow rates as boundary conditions for image-based hemodynamic models of the human aorta: implications for indicators of abnormal flow. Ann. Biomed. Eng. 40:729–741, 2012.
Gaudino, M., A. Di Franco, D. L. Bhatt, J. H. Alexander, A. Abbate, L. Azzalini, S. Sandner, G. Sharma, S. V. Rao, F. Crea, S. E. Fremes, and S. Bangalore. The association between coronary graft patency and clinical status in patients with coronary artery disease. Eur. Heart J. 42:1433–1441, 2021.
Gijsen, F., Y. Katagiri, P. Barlis, C. Bourantas, C. Collet, U. Coskun, J. Daemen, J. Dijkstra, E. Edelman, P. Evans, K. van der Heiden, R. Hose, B.-K. Koo, R. Krams, A. Marsden, F. Migliavacca, Y. Onuma, A. Ooi, E. Poon, H. Samady, P. Stone, K. Takahashi, D. Tang, V. Thondapu, E. Tenekecioglu, L. Timmins, R. Torii, J. Wentzel, and P. Serruys. Expert recommendations on the assessment of wall shear stress in human coronary arteries: existing methodologies, technical considerations, and clinical applications. Eur. Heart J. 40:3421–3433, 2019.
Gimbrone, M. A., and G. García-Cardeña. Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ. Res. 118:620–636, 2016.
Goldman, S., K. Zadina, T. Moritz, T. Ovitt, G. Sethi, J. G. Copeland, L. Thottapurathu, B. Krasnicka, N. Ellis, R. J. Anderson, and W. Henderson. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: Results from a Department of Veterans Affairs Cooperative Study. J. Am. Coll. Cardiol. 44:2149–2156, 2004.
Heiberg, E., C. Green, J. Toger, A. M. Andersson, M. Carlsson, and H. Arheden. FourFlow-open source code software for quantification and visualization of time-resolved three-directional phase contrast magnetic resonance velocity mapping. J. Cardiovasc. Magn. Reson. 14:W14, 2012.
Heiberg, E., J. Sjögren, M. Ugander, M. Carlsson, H. Engblom, and H. Arheden. Design and validation of segment-freely available software for cardiovascular image analysis. BMC Med. Imaging. 10:1, 2010.
Hwang, H. Y., B.-K. Koo, S. Y. Yeom, T. K. Kim, and K.-B. Kim. Endothelial shear stress of the saphenous vein composite graft based on the internal thoracic artery. Ann. Thorac. Surg. 105:564–571, 2018.
Jiménez-Juan, L., E. T. Nguyen, B. J. Wintersperger, H. Moshonov, A. M. Crean, D. P. Deva, N. S. Paul, and F. S. Torres. Failed heart rate control with oral metoprolol prior to coronary CT angiography: effect of additional intravenous metoprolol on heart rate, image quality and radiation dose. Int. J. Cardiovasc. Imaging. 29:199–206, 2013.
Khan, M. O., J. S. Tran, H. Zhu, J. Boyd, R. R. S. Packard, R. P. Karlsberg, A. M. Kahn, and A. L. Marsden. Low wall shear stress is associated with saphenous vein graft stenosis in patients with coronary artery bypass grafting. J. Cardiovasc. Trans. Res. 2020. https://doi.org/10.1007/s12265-020-09982-7.
Kim, H. J., I. E. Vignon-Clementel, J. S. Coogan, C. A. Figueroa, K. E. Jansen, and C. A. Taylor. Patient-specific modeling of blood flow and pressure in human coronary arteries. Ann. Biomed. Eng. 38:3195–3209, 2010.
Lopes, R. D., R. H. Mehta, G. E. Hafley, J. B. Williams, M. J. Mack, E. D. Peterson, K. B. Allen, R. A. Harrington, C. M. Gibson, R. M. Califf, N. T. Kouchoukos, T. B. Ferguson, J. H. Alexander, Project of Ex Vivo Vein Graft Engineering via Transfection IV (PREVENT IV) Investigators. Relationship between vein graft failure and subsequent clinical outcomes after coronary artery bypass surgery. Circulation. 125:749–756, 2012.
Markl, M., G. J. Wagner, and A. J. Barker. Re: Blood flow analysis of the aortic arch using computational fluid dynamics. Eur. J. Cardiothorac. Surg. 49:1586–1587, 2016.
Petrie, M. C., P. S. Jhund, L. She, C. Adlbrecht, T. Doenst, J. A. Panza, J. A. Hill, K. L. Lee, J. L. Rouleau, D. L. Prior, I. S. Ali, J. Maddury, K. S. Golba, H. D. White, P. Carson, L. Chrzanowski, A. Romanov, A. B. Miller, and E. J. Velazquez. Ten year outcomes after coronary artery bypass grafting according to age in patients with heart failure and left ventricular systolic dysfunction: an analysis of the extended follow up of the STICH trial. Circulation. 134:1314–1324, 2016.
Pinho-Gomes, A.-C., L. Azevedo, C. Antoniades, and D. P. Taggart. Comparison of graft patency following coronary artery bypass grafting in the left versus the right coronary artery systems: a systematic review and meta-analysis. Eur. J. Cardiothorac. Surg. 54:221–228, 2018.
Pirola, S., Z. Cheng, O. A. Jarral, D. P. O’Regan, J. R. Pepper, T. Athanasiou, and X. Y. Xu. On the choice of outlet boundary conditions for patient-specific analysis of aortic flow using computational fluid dynamics. J. Biomech. 60:15–21, 2017.
Ramachandra, A. B., A. M. Kahn, and A. L. Marsden. Patient-specific simulations reveal significant differences in mechanical stimuli in venous and arterial coronary grafts. J. Cardiovasc. Transl. Res. 9:279–290, 2016.
Sankaran, S., M. Esmaily Moghadam, A. M. Kahn, E. E. Tseng, J. M. Guccione, and A. L. Marsden. Patient-specific multiscale modeling of blood flow for coronary artery bypass graft surgery. Ann. Biomed. Eng. 40:2228–2242, 2012.
Seo, J., A. B. Ramachandra, J. Boyd, A. L. Marsden, and A. M. Kahn. Computational evaluation of venous graft geometries in coronary artery bypass surgery. Semin. Thorac. Cardiovasc. Surg. 2021. https://doi.org/10.1053/j.semtcvs.2021.03.007.
Stone, P. H., S. Saito, S. Takahashi, Y. Makita, S. Nakamura, T. Kawasaki, A. Takahashi, T. Katsuki, S. Nakamura, A. Namiki, and A. Hirohata. Prediction of progression of coronary artery disease and clinical outcomes using vascular profiling of endothelial shear stress and arterial plaque characteristics. Circulation. 126:172–181, 2012.
Taylor, A. J., et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. J. Cardiovasc. Comput. Tomogr. 4:407.e1-407.e33, 2010.
Taylor, C. A., T. A. Fonte, and J. K. Min. Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: scientific basis. J. Am. Coll. Cardiol. 61:2233–2241, 2013.
Tran-Nguyen, N., F. Condemi, A. Yan, S. Fremes, P. Triverio, and L. Jimenez-Juan. Wall shear stress differences between arterial and venous coronary artery bypass grafts one month after surgery. Ann. Biomed. Eng. 2022. https://doi.org/10.1007/s10439-022-03007-x.
Updegrove, A., N. M. Wilson, J. Merkow, H. Lan, A. L. Marsden, and S. C. Shadden. SimVascular: an open source pipeline for cardiovascular simulation. Ann. Biomed. Eng. 45:525–541, 2017.
Zhou, Y., G. S. Kassab, and S. Molloi. On the design of the coronary arterial tree: a generalization of Murray’s law. Phys. Med. Biol. 44:2929–2945, 1999.
Zientara, A., L. Rings, H. Bruijnen, O. Dzemali, D. Odavic, A. Häussler, M. Gruszczynski, and M. Genoni. Early silent graft failure in off-pump coronary artery bypass grafting: a computed tomography analysis†. Eur. J. Cardiothorac. Surg. 56:919–925, 2019.
Acknowledgments
This work was supported by the RSNA Scholar Grant #RSCH1716, by the Department of Medical Imaging of the University of Toronto, by the Jean & Lauri Hiivala Research Fund for Heart Health, by the Institute of Biomedical Engineering of the University of Toronto, by the Canada Research Chairs program, and by Compute Canada.
Conflict of interest
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Arash Kheradvar oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tran-Nguyen, N., Yan, A.T., Fremes, S. et al. Abnormal Wall Shear Stress Area is Correlated to Coronary Artery Bypass Graft Remodeling 1 Year After Surgery. Ann Biomed Eng 51, 1588–1601 (2023). https://doi.org/10.1007/s10439-023-03167-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-023-03167-4