Abstract
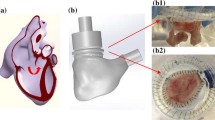
The scarcity of data available on the best approach for pulmonary fetal valve replacement or implantation necessitate an investigation on whether practices using adult transcatheter valves could be translated to fetal applications. The objective of this study is to evaluate the hemodynamic characteristics and the turbulent properties of a fetal sized trileaflet transcatheter pulmonary valve in comparison with an adult balloon-expandable valve in order to assess the possibility of designing valves for fetal applications using dynamic similarity. A 6 mm fetal trileaflet valve and a 26 mm SAPIEN 3 valve were assessed in a pulse duplicator. Particle image velocimetry was performed. Pressure gradient (ΔP), effective orifice area (EOA), regurgitant fractions (RF), pinwheeling indices (PI) and turbulent stresses were evaluated. ΔP was 8.56 ± 0.139 and 7.76 ± 0.083 mmHg with fetal valve and SAPIEN respectively (p < 0.0001); EOA was 0.10 ± 0.0007 and 2.1 ± 0.025 cm2 with fetal valve and SAPIEN respectively (p < 0.0001); RF with the fetal valve was 2.35 ± 1.99% and with SAPIEN 10.92 ± 0.11% (p < 0.0001); PI with fetal valve was 0.404 ± 0.01 and with SAPIEN 0.37 ± 0.07; The flow regime with the fetal valve was turbulent and Reynolds numbers reached about 7000 while those with the SAPIEN reached about 20,000 at peak velocity. Turbulent stresses were significantly higher with fetal valve compared with SAPIEN. Instantaneous viscous shear stresses with fetal valve were 5.8 times higher than those obtained with SAPIEN and Reynolds shear stresses were 2.5 times higher during peak systole. The fetal valve implantation leads to a turbulent flow (specific to this particular type and design of valve) regime unlike what is expected of a small valve with different flow properties compared to adult valves.










Similar content being viewed by others
References
Abdel-Wahab, M., F.-J. Neumann, J. Mehilli, C. Frerker, D. Richardt, M. Landt, J. Jose, R. Toelg, K.-H. Kuck, and S. Massberg. 1-year outcomes after transcatheter aortic valve replacement with balloon-expandable versus self-expandable valves: results from the CHOICE randomized clinical trial. J. Am. Coll. Cardiol. 66:791–800, 2015.
Alexander, R. M., and A. Jayes. A dynamic similarity hypothesis for the gaits of quadrupedal mammals. J. Zool. 201:135–152, 1983.
Angelini, A., M. Fedrigo, C. Frescura, and G. Thiene. Fetal anatomy: the pulmonary valve in fetal pulmonary valve disease. In: Fetal and Hybrid Procedures in Congenital Heart Diseases, edited by G. Butera, J. Cheatham, C. A. Pedra, D. Schranz, and G. Tulzer. New York: Springer, 2016, pp. 61–67.
Antiga, L., and D. A. Steinman. Rethinking turbulence in blood. Biorheology 46:77–81, 2009.
Cartier, M., and P. Doubilet. Fetal aortic and pulmonary artery diameters: sonographic measurements in growth-retarded fetuses. Am. J. Roentgenol. 151:991–993, 1988.
Dasi, L. P., H. A. Simon, P. Sucosky, and A. P. Yoganathan. Fluid mechanics of artificial heart valves. Clin. Exp. Pharmacol. Physiol. 36:225–237, 2009.
De Smedt, M. C., G. H. Visser, and E. J. Meijboom. Fetal cardiac output estimated by Doppler echocardiography during mid-and late gestation. Am. J. Cardiol. 60:338–342, 1987.
Freud, L. R., D. B. McElhinney, A. C. Marshall, G. R. Marx, K. G. Friedman, P. J. del Nido, S. M. Emani, T. Lafranchi, V. Silva, and L. E. Wilkins-Haug. Fetal aortic valvuloplasty for evolving hypoplastic left heart syndrome: postnatal outcomes of the first 100 patients. Circulation 130:638–645, 2014.
Ge, L., L. P. Dasi, F. Sotiropoulos, and A. P. Yoganathan. Characterization of hemodynamic forces induced by mechanical heart valves: Reynolds vs. viscous stresses. Ann. Biomed. Eng. 36:276–297, 2008.
Giersiepen, M., L. Wurzinger, R. Opitz, and H. Reul. Estimation of shear stress-related blood damage in heart valve prostheses—in vitro comparison of 25 aortic valves. Int. J. Artif. Organs. 13:300–306, 1990.
Graupner, O., C. Enzensberger, and R. Axt-Fliedner. New aspects in the diagnosis and therapy of fetal hypoplastic left heart syndrome. Geburtshilfe Frauenheilkd 79:863–872, 2019.
Gunning, P. S., N. Saikrishnan, L. M. McNamara, and A. P. Yoganathan. An in vitro evaluation of the impact of eccentric deployment on transcatheter aortic valve hemodynamics. Ann. Biomed. Eng. 42:1195–1206, 2014.
Gunning, P. S., N. Saikrishnan, A. P. Yoganathan, and L. M. McNamara. Total ellipse of the heart valve: the impact of eccentric stent distortion on the regional dynamic deformation of pericardial tissue leaflets of a transcatheter aortic valve replacement. J. R. Soc. Interface 12:20150737, 2015.
Gurvitch, R., S. Toggweiler, A. B. Willson, N. Wijesinghe, A. Cheung, D. A. Wood, J. Ye, and J. G. Webb. Outcomes and complications of transcatheter aortic valve replacement using a balloon expandable valve according to the Valve Academic Research Consortium (VARC) guidelines. EuroIntervention 7:41–48, 2011.
Hamill, N., L. Yeo, R. Romero, S. S. Hassan, S. A. Myers, P. Mittal, J. P. Kusanovic, M. Balasubramaniam, T. Chaiworapongsa, and E. Vaisbuch. Fetal cardiac ventricular volume, cardiac output, and ejection fraction determined with 4-dimensional ultrasound using spatiotemporal image correlation and virtual organ computer-aided analysis. Am. J. Obstet. Gynecol. 205:76, 2011.
Hansson, N. C., E. L. Grove, H. R. Andersen, J. Leipsic, O. N. Mathiassen, J. M. Jensen, K. T. Jensen, P. Blanke, T. Leetmaa, and M. Tang. Transcatheter aortic valve thrombosis: incidence, predisposing factors, and clinical implications. J. Am. Coll. Cardiol. 68:2059–2069, 2016.
Hatoum, H., and L. P. Dasi. Reduction of pressure gradient and turbulence using vortex generators in prosthetic heart valves. Ann. Biomed. Eng. 47:85–96, 2019.
Hatoum, H., J. Dollery, S. M. Lilly, J. Crestanello, and L. P. Dasi. Impact of patient-specific morphologies on sinus flow stasis in transcatheter aortic valve replacement: an in vitro study. J. Thorac. Cardiovasc. Surg. 157:540–549, 2019.
Hatoum, H., J. Dollery, S. M. Lilly, J. A. Crestanello, and L. P. Dasi. Sinus hemodynamics variation with tilted transcatheter aortic valve deployments. Ann. Biomed. Eng. 47:75–84, 2019.
Hatoum, H., E. Girault, F. Heim, L. P. Dasi, and JTJot and surgery c. In-vitro characterization of self-expandable textile transcatheter aortic valves. J. Mech. Behav. Biomed. Mater. 103:103559, 2020.
Hatoum, H., F. Heim, and L. P. Dasi. Stented valve dynamic behavior induced by polyester fiber leaflet material in transcatheter aortic valve devices. J. Mech. Behav. Biomed. Mater. 86:232–239, 2018.
Hatoum, H., S. Lilly, P. Maureira, J. Crestanello, L. P. Dasi, and JTJot and surgery c. The hemodynamics of transcatheter aortic valves in transcatheter aortic valves. J. Thorac. Cardiovasc. Surg. 2019. https://doi.org/10.1016/j.jtcvs.2019.09.174.
Hatoum, H., P. Maureira, S. Lilly, and L. P. Dasi. Impact of leaflet laceration on transcatheter aortic valve-in-valve washout: BASILICA to solve neosinus and sinus stasis. JACC 12:1229–1237, 2019.
Hatoum, H., B. L. Moore, and L. P. Dasi. On the significance of systolic flow waveform on aortic valve energy loss. Ann. Biomed. Eng. 46:2102–2111, 2018.
Hatoum, H., A. Yousefi, S. Lilly, P. Maureira, J. Crestanello, and L. P. Dasi. An in vitro evaluation of turbulence after transcatheter aortic valve implantation. J. Thorac. Cardiovasc. Surg. 156:1837–1848, 2018.
Heitkemper, M., H. Hatoum, and L. P. Dasi. In vitro hemodynamic assessment of a novel polymeric transcatheter aortic valve. J. Mech. Behav. Biomed. Mater. 98:163–171, 2019.
Jones, S. A. A relationship between Reynolds stresses and viscous dissipation: implications to red cell damage. Ann. Biomed. Eng. 23:21–28, 1995.
Kameneva, M, G. Burgreen, K. Kono, J. Antaki, B. Repko, and M. Umezu. On the mechanical blood trauma: Effect of turbulence. Proceedings of the First Joint BMES/EMBS Conference 1999 IEEE Engineering in Medicine and Biology 21st Annual Conference and the 1999 Annual Fall Meeting of the Biomedical Engineering Society (Cat N. 1999);2:772 vol. 2, 1999.
Kameneva, M. V., G. W. Burgreen, K. Kono, B. Repko, J. F. Antaki, and M. Umezu. Effects of turbulent stresses on mechanical hemolysis: experimental and computational analysis. ASAIO J. 50:418, 2004.
Kverneland, L. S., P. Kramer, and S. Ovroutski. Five decades of the Fontan operation: a systematic review of international reports on outcomes after univentricular palliation. Congenit. Heart Dis. 13:181–193, 2018.
Laflamme, J., R. Puri, M. Urena, L. Laflamme, H. DeLarochellière, O. A.-J. Altisent, M. Del Trigo, F. Campelo-Parada, R. DeLarochellière, and J. M. Paradis. Incidence and risk factors of hemolysis after transcatheter aortic valve implantation with a balloon-expandable valve. Am. J. Cardiol. 115:1574–1579, 2015.
Martin, C., and W. Sun. Simulation of long-term fatigue damage in bioprosthetic heart valves: effects of leaflet and stent elastic properties. Biomech. Model. Mechanobiol. 13:759–770, 2014.
Martin, C., and W. Sun. Transcatheter valve underexpansion limits leaflet durability: implications for valve-in-valve procedures. Ann. Biomed. Eng. 45:394–404, 2017.
McElhinney, D. B., W. Tworetzky, and J. E. Lock. Current status of fetal cardiac intervention. Circulation 121:1256–1263, 2010.
Nakayama, Y., K. Yuasa, and T. Tajikawa. First time development of biovalve mitral valve: in vitro performance. Struct. Heart 3:138–138, 2019.
Nanjappa, B., H.-K. Chang, and C. A. Glomski. Trauma of the erythrocyte membrane associated with low shear stress. Biophys. J. 13:1212–1222, 1973.
Nygaard, H., M. Giersiepen, J. Hasenkam, H. Reul, P. Paulsen, P. Rovsing, and D. Westphal. Two-dimensional color-mapping of turbulent shear stress distribution downstream of two aortic bioprosthetic valves in vitro. J. Biomech. 25:437–440, 1992.
Pritchard, P. J., and J. W. Mitchell. Fox and McDonald’s Introduction to Fluid Mechanics. Binder Ready Version: Wiley, 2016.
Ramstack, J., L. Zuckerman, and L. Mockros. Shear-induced activation of platelets. J. Biomech. 12:113–125, 1979.
Sutera, S. P. Flow-induced trauma to blood cells. Circ. Res. 41:2–8, 1977.
Tulzer, G., and W. Arzt. IS-024 fetal cardiac interventions. Arch. Dis. Childhood 99:A8, 2014.
Tworetzky, W., L. Wilkins-Haug, R. W. Jennings, M. E. van der Velde, A. C. Marshall, G. R. Marx, S. D. Colan, C. B. Benson, J. E. Lock, and S. B. Perry. Balloon dilation of severe aortic stenosis in the fetus: potential for prevention of hypoplastic left heart syndrome: candidate selection, technique, and results of successful intervention. Circulation 110:2125–2131, 2004.
Willson, A. B., J. Rodès-Cabau, D. A. Wood, J. Leipsic, A. Cheung, S. Toggweiler, R. K. Binder, M. Freeman, R. DeLarochellière, and R. Moss. Transcatheter aortic valve replacement with the St. Jude Medical Portico valve: first-in-human experience. J. Am. Coll. Cardiol. 60:581–586, 2012.
Wurzinger, L., R. Opitz, M. Wolf, and H. Schmid-Schönbein. “Shear induced platelet activation”—a critical reappraisal. Biorheology 22:399–413, 1985.
Yanagisawa, R., M. Tanaka, F. Yashima, T. Arai, M. Jinzaki, H. Shimizu, K. Fukuda, Y. Watanabe, T. Naganuma, and A. Higashimori. Early and late leaflet thrombosis after transcatheter aortic valve replacement: a multicenter initiative from the OCEAN-TAVI Registry. Circulation. 12:7349, 2019.
Yoganathan, A. P., Z. He, and Jones S. Casey. Fluid mechanics of heart valves. Annu. Rev. Biomed. Eng. 6:331–362, 2004.
Funding
The research done was partly supported by National Institutes of Health (NIH) under Award Number R01HL119824 and the American Heart Association (AHA) under Award Number 19POST34380804.
Disclosures
Dr. Dasi reports having patent applications filed on vortex generators and superhydrophobic/omniphobic surfaces. Dr. Dasi report having two patents filed on novel polymeric heart valves. No other conflicts were reported.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Daniel Elson oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hatoum, H., Gooden, S., Heitkemper, M. et al. Fetal Transcatheter Trileaflet Heart Valve Hemodynamics: Implications of Scaling on Valve Mechanics and Turbulence. Ann Biomed Eng 48, 1683–1693 (2020). https://doi.org/10.1007/s10439-020-02475-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-020-02475-3