Abstract
Purpose
Lower aerobic fitness increases the risk of developing hypertension. Muscle sympathetic nerve activity (MSNA) is important for the beat-by-beat regulation of blood pressure. Whether the cardiovascular consequences of lower aerobic fitness are due to augmented transduction of MSNA into vascular responses is unclear. We tested the hypothesis that aerobic fitness is inversely related to peak increases in total peripheral resistance (TPR) and mean arterial pressure (MAP) in response to spontaneous MSNA bursts in young males.
Methods
Relative peak oxygen consumption (VO2peak, indirect calorimetry) was assessed in 18 young males (23 ± 3 years; 41 ± 8 ml/kg/min). MSNA (microneurography), cardiac intervals (electrocardiogram) and arterial pressure (finger photoplethysmography) were recorded continuously during supine rest. Stroke volume and cardiac output (CO) were estimated via the ModelFlow method. TPR was calculated as MAP/CO. Changes in TPR and MAP were tracked for 12 cardiac cycles following heartbeats associated with or without spontaneous bursts of MSNA.
Results
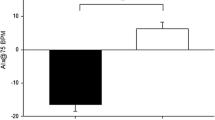
Overall, aerobic fitness was inversely correlated to the peak ΔTPR (0.8 ± 0.7 mmHg/l/min; R = − 0.61, P = 0.007) and ΔMAP (2.3 ± 0.8 mmHg; R = − 0.69, P < 0.001), but not with the peak ΔCO (0.2 ± 0.1 l/min; P = 0.50), MSNA burst frequency (14 ± 5 bursts/min; P = 0.43) or MSNA relative burst amplitude (65 ± 12%; P = 0.13). Heartbeats without an associated burst of MSNA did not increase TPR, MAP or CO.
Conclusion
Although unrelated to traditional MSNA characteristics, aerobic fitness was inversely associated with spontaneous sympathetic neurovascular transduction in young males. This may be a potential mechanism by which aerobic fitness modulates the regulation of arterial blood pressure through the sympathetic nervous system.


Similar content being viewed by others
References
McKinney J, Lithwick D, Morrison B et al (2016) The health benefits of physical activity and cardiorespiratory fitness. BCMJ 58:131–137
Clausen JSR, Marott JL, Holtermann A et al (2018) Midlife cardiorespiratory fitness and the long-term risk of mortality. J Am Coll Cardiol 72:987–995. https://doi.org/10.1016/j.jacc.2018.06.045
Laukkanen JA, Zaccardi F, Khan H et al (2016) Long-term change in cardiorespiratory fitness and all-cause mortality. Mayo Clin Proc 91:1183–1188. https://doi.org/10.1016/j.mayocp.2016.05.014
Carnethon MR, Evans NS, Church TS et al (2010) Joint associations of physical activity and aerobic fitness on the development of incident hypertension. Hypertension 56:49–55. https://doi.org/10.1161/HYPERTENSIONAHA.109.147603
Carnethon MR, Gidding S, Nehgme R et al (2003) Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA 290:3092. https://doi.org/10.1001/jama.290.23.3092
Hart EC, Charkoudian N (2011) Sympathetic neural mechanisms in human blood pressure regulation. Curr Hypertens Rep 13:237–243. https://doi.org/10.1007/s11906-011-0191-1
Notarius CF, Murai H, Morris BL, Floras JS (2012) Effect of fitness on reflex sympathetic neurovascular transduction in middle-age men. Med Sci Sport Exerc 44:232–237. https://doi.org/10.1249/MSS.0b013e31822a68a5
Fairfax ST, Holwerda SW, Credeur DP et al (2013) The role of α-adrenergic receptors in mediating beat-by-beat sympathetic vascular transduction in the forearm of resting man. J Physiol 591:3637–3649. https://doi.org/10.1113/jphysiol.2013.250894
Fairfax ST, Padilla J, Vianna LC et al (2013) Spontaneous bursts of muscle sympathetic nerve activity decrease leg vascular conductance in resting humans. Am J Physiol Heart Circ Physiol 304:H759–H766. https://doi.org/10.1152/ajpheart.00842.2012
Briant LJB, Burchell AE, Ratcliffe LEK et al (2016) Quantifying sympathetic neuro-haemodynamic transduction at rest in humans: insights into sex, ageing and blood pressure control. J Physiol 594:4753–4768. https://doi.org/10.1113/JP272167
Steinback CD, Fraser GM, Usselman CW et al (2019) Blunted sympathetic neurovascular transduction during normotensive pregnancy. J Physiol 597:3687–3696. https://doi.org/10.1113/JP277714
Robinson AT, Babcock MC, Watso JC et al (2019) Relation between resting sympathetic outflow and vasoconstrictor responses to sympathetic nerve bursts: sex differences in healthy young adults. Am J Physiol Integr Comp Physiol 316:R463–R471. https://doi.org/10.1152/ajpregu.00305.2018
Vianna LC, Hart EC, Fairfax ST et al (2012) Influence of age and sex on the pressor response following a spontaneous burst of muscle sympathetic nerve activity. Am J Physiol Circ Physiol 302:H2419–H2427. https://doi.org/10.1152/ajpheart.01105.2011
Coovadia Y, Adler TE, Steinback CD et al (2020) Sex differences in dynamic blood pressure regulation: beat-by-beat responses to muscle sympathetic nerve activity. Am J Physiol Circ Physiol 319:H531–H538. https://doi.org/10.1152/ajpheart.00245.2020
Babcock MC, Robinson AT, Migdal KU et al (2019) Reducing dietary sodium to 1000 mg per day reduces neurovascular transduction without stimulating sympathetic outflow. Hypertension 73:587–593. https://doi.org/10.1161/HYPERTENSIONAHA.118.12074
Vranish JR, Holwerda SW, Young BE et al (2018) Exaggerated vasoconstriction to spontaneous bursts of muscle sympathetic nerve activity in healthy young black men. Hypertension 71:192–198. https://doi.org/10.1161/HYPERTENSIONAHA.117.10229
Young BE, Holwerda SW, Vranish JR et al (2019) Sympathetic transduction in type 2 diabetes mellitus. Hypertension 74:201–207. https://doi.org/10.1161/HYPERTENSIONAHA.119.12928
Hissen SL, Taylor CE (2020) Sex differences in vascular transduction of sympathetic nerve activity. Clin Auton Res. https://doi.org/10.1007/s10286-020-00722-0
Hart EC, Charkoudian N, Wallin BG et al (2011) Sex and ageing differences in resting arterial pressure regulation: the role of the β-adrenergic receptors. J Physiol 589:5285–5297. https://doi.org/10.1113/jphysiol.2011.212753
Christou DD, Jones PP, Jordan J et al (2005) Women have lower tonic autonomic support of arterial blood pressure and less effective baroreflex buffering than men. Circulation 111:494–498. https://doi.org/10.1161/01.CIR.0000153864.24034.A6
Thijssen DHJ, Bruno RM, van Mil ACCM et al (2019) Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J 40:2534–2547. https://doi.org/10.1093/eurheartj/ehz350
Borg G (1982) Psychophysical basis of perceived exertion. Med Sci Sport Exerc 14:377–381. https://doi.org/10.1249/00005768-198205000-00012
Hart EC, Head GA, Carter JR et al (2017) Recording sympathetic nerve activity in conscious humans and other mammals: guidelines and the road to standardization. Am J Physiol Circ Physiol 312:H1031–H1051. https://doi.org/10.1152/ajpheart.00703.2016
Kimmerly DS, O’Leary DD, Shoemaker JK (2004) Test–retest repeatability of muscle sympathetic nerve activity: influence of data analysis and head-up tilt. Auton Neurosci 114:61–71. https://doi.org/10.1016/j.autneu.2004.06.005
Hissen SL, Macefield VG, Brown R, Taylor CE (2019) Sympathetic baroreflex sensitivity is inversely related to vascular transduction in men but not women. Am J Physiol Circ Physiol 317:H1203–H1209. https://doi.org/10.1152/ajpheart.00501.2019
Esler MD, Hasking GJ, Willett IR et al (1985) Noradrenaline release and sympathetic nervous system activity. J Hypertens 3:117–129. https://doi.org/10.1097/00004872-198504000-00003
Ninomiya I, Malpas SC, Matsukawa K et al (1993) The amplitude of synchronized cardiac sympathetic nerve activity reflects the number of activated pre- and postganglionic fibers in anesthetized cats. J Auton Nerv Syst 45:139–147. https://doi.org/10.1016/0165-1838(93)90125-E
Donato AJ, Lesniewski LA, Delp MD (2007) Ageing and exercise training alter adrenergic vasomotor responses of rat skeletal muscle arterioles. J Physiol 579:115–125. https://doi.org/10.1113/jphysiol.2006.120055
Montero D (2015) The association of cardiorespiratory fitness with endothelial or smooth muscle vasodilator function. Eur J Prev Cardiol 22:1200–1211. https://doi.org/10.1177/2047487314553780
Funding
Canadian Foundation for Innovation: Leader’s Opportunity Fund (DSK), Faculty of Health Professions Research Development (DSK), and Nova Scotia Health Research Foundation (NSHRF) Development/Innovation (DSK) Grants. MWO was supported by a Heart & Stroke BrightRed Scholarship, Nova Scotia Graduate Scholarship, an NSHRF Scotia Scholars Award, and a Killam PreDoctoral Scholarship.
Author information
Authors and Affiliations
Contributions
MWO and DSK conceived and designed the study. All authors were involved with data collection. MWO created the neurovascular transduction analysis program and analyzed the data. MWO and DSK interpreted the data. MWO drafted the manuscript. All authors revised and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Ethical approval
Research ethics board approval was attained from Dalhousie University. Participants provided written, informed consent prior to study enrollment.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10286_2020_734_MOESM1_ESM.tif
Supplemental Figure 1. The relationship between peak relative activity and the peak pressor responses for total peripheral resistance (TPR; panel A), mean arterial pressure (MAP; panel B) and cardiac output (CO; C). Data were analyzed by burst pattern including singlets (circles), doublets (triangles) and triplets+ (squares. Within each burst pattern, data were ordered based on burst sequence amplitude quartiles denoted by Q1 (black), Q2 (dark grey), Q3 (light grey), and Q4 (white). Data presented as means ± standard deviations. The relationship between peak relative activity (%) and the peak pressor responses were determined via Pearson correlations for each variable (TIF 13300 kb)
Rights and permissions
About this article
Cite this article
O’Brien, M.W., Ramsay, D., Johnston, W. et al. Aerobic fitness and sympathetic responses to spontaneous muscle sympathetic nerve activity in young males. Clin Auton Res 31, 253–261 (2021). https://doi.org/10.1007/s10286-020-00734-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-020-00734-w