Abstract
Background
Hyperuricemia would be a risk factor for the development/progression of CKD. However, several studies showed U-shape association between serum uric acid level and renal impairment, suggesting that hypouricemia was rather associated with renal dysfunction. Perhaps, there is the optimal target level of serum UA for renal function.
Methods
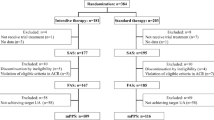
The Target-UA study is a multicenter randomized controlled trial. Eligible CKD patients (eGFR ≥ 30, < 60 mL/min/1.73 m2 and urine protein < 0.5 g/gCr or urine albumin to creatinine ratio (ACR) < 300 mg/gCr) with serum UA ≥ 8.0 mg/dL (≥ 7.0 mg/dl: under the treatment) will be enrolled and be randomly assigned to the intensive therapy group (target serum UA level ≥ 4.0 mg/dL, < 5.0 mg/dL) or the standard therapy group (serum UA level ≥ 6.0 mg/dL, < 7.0 mg/dL). Topiroxostat, a new xanthine oxidase inhibitor, will be administered to treat hyperuricemia. The primary endpoint is a change in logarithmic value of urine ACR between baseline and week 52 of treatment. The secondary endpoints include changes in serum UA, eGFR, urine protein, lipid profile, and onset of composite cardiovascular events, renal events, gouty arthritis, and attack of urolithiasis. The number of subjects has been set to be 185 in each group for a total of 370.
Discussion
This is the first study, to the best of our knowledge, to determine the optimal target level of serum UA for renal protection and is expected to lead to progress in CKD treatment.
Trial registration
(UMIN000026741 and jRCTs051180146).


Similar content being viewed by others
Personal data protection and confidentiality
Personal information and data will be converted to an anonymous, unique identification code unrelated to any personal information. The data center and person(s) in charge of statistical analysis will handle patient data using the identification code numbers.
References
Importance of CKD. In: Japanese Society of Nephrology edit. Clinical Practice Guidebook for Diagnosis and Treatment of Chronic Kidney Disease. Tokyo: TOKYO IGAKUSHA; 2012. pp. 5–7.
Lysaght MJ. Maintenance dialysis population dynamics: current trends and long-term implications. J Am Soc Nephrol. 2002;13 Suppl 1:S37–40.
Iseki K, Ikemiya Y, Iseki C. Proteinuria and the risk of developing end-stage renal disease. Kidney Int. 2003;63:1468–1474.
Zhang Z, Shahinfar S, Keane WF. Importance of baseline distribution of proteinuria in renal outcomes trials: lessons from the reduction of endpoints in NIDDM with the angiotensin II antagonist losartan (RENAAL) study. J Am Soc Nephrol. 2005;16:1775–1780.
Peterson JC, Adler S, Burkart JM. Blood pressure control, proteinuria, and the progression of renal disease. The modification of diet in renal disease study. Ann Intern Med. 1995;123:754–762.
Lea J, Greene T, Hebert L. The relationship between magnitude of proteinuria reduction and risk of end-stage renal disease: results of the African American study of kidney disease and hypertension. Arch Intern Med. 2005;165:947–953.
Halbesma N, Kuiken DS, Brantsma AH. Macroalbuminuria is a better risk marker than low estimated GFR to identify individuals at risk for accelerated GFR loss in population screening. J Am Soc Nephrol. 2006;17:2582–2590.
Gerstein HC, Mann JF, Yi Q. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001; 286:421–426.
Wachtell K, Ibsen H, Olsen MH. Albuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: the LIFE study. Ann Intern Med. 2003;139:901–906.
Arnlöv J, Evans JC, Meigs JB. Low-grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: the Framingham Heart Study. Circulation. 2005;112:969–975.
Ibsen H, Olsen MH, Wachtell K. Reduction in albuminuria translates to reduction in cardiovascular events in hypertensive patients: losartan intervention for endpoint reduction in hypertension study. Hypertension. 2005;45:198–202.
Yu MA, Sánchez-Lozada LG, Johnson RJ. Oxidative stress with an activation of the renin-angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. J Hypertens. 2010;28:1234–1242.
Tsuda H, Kawada N, Kaimori JY Febuxostat suppressed renal ischemia-reperfusion injury via reduced oxidative stress. Biochem Biophys Res Commun. 2012;427:266–272.
Nakagawa T, Mazzali M, Kang DH. Hyperuricemia causes glomerular hypertrophy in the rat. Am J Nephrol. 2003;23:2–7.
Hayashino Y, Okamura S, Tsujii S, Ishii H. Association of serum uric acid levels with the risk of development or progression of albuminuria among Japanese patients with type 2 diabetes: a prospective cohort study [Diabetes Distress and Care Registry at Tenri (DDCRT 10)]. Acta Diabetol. 2016;53:599–607.
Suzuki K, Konta T, Kudo K. The association between serum uric acid and renal damage in a community-based population: the Takahata study. Clin Exp Nephrol. 2013;17:541–548.
The Japanese Society of Nephrology. Evidence-based clinical practice guideline for CKD 2013. Clin Exp Nephrol. 2014;18:346–423.
Goicoechea M, Vinuesa de SG, Verdalles U. Effect of allopurinol in chronic kidney disease progression and cardiovascular risk. Clin J Am Soc Nephrol. 2010;5:1388–1393.
Iseki K, Oshiro S, Tozawa M Significance of hyperuricemia on the early detection of renal failure in a cohort of screened subjects. Hypertens Res. 2001;24:691–697.
Satirapoj B, Supasyndh O, Chaiprasert A. Relationship between serum uric acid levels with chronic kidney disease in a Southeast Asian population. Nephrology (Carlton). 2010;15:253–258.
Hande KR Noone RM Stone WJ. Severe allopurinol toxicity. Description and guidelines for prevention in patients with renal insufficiency. Am J Med. 1984;76:47–56.
GlaxoSmithLkine K.K. Zyloric® tablets package insert (18th edition). 2017. https://www.info.pmda.go.jp/go/pack/3943001F1314_W_12/.
Fuji Yakuhin Co., Ltd. Topiloric® tablets package insert (4th edition). 2016. https://www.info.pmda.go.jp/go/pack/3949004F1036_1_03/. Accessed 1 Oct 2019.
Teijin Pharma Limited. Feburic® tablets package insert, (8th edition). 2016. https://www.info.pmda.go.jp/go/pack/3949003F1023_1_09/. Accessed 1 Oct 2019.
Murase T, Nampei M, Oka M. A highly sensitive assay of human plasma xanthine oxidoreductase activity using stable isotope-labeled xanthine and LC/TQMS. J Chromatogr B Anal Technol Biomed Life Sci. 2016;1039:51–58.
Bellomo G, Venanzi S, Verdura C. Association of uric acid with change in kidney function in healthy normotensive individuals. Am J Kidney Dis. 2010;56:264–272.
Obermayr RP, Temml C, Gutjahr G. Elevated uric acid increases the risk for kidney disease. J Am Soc Nephrol. 2008;19:2407–2413.
Siu YP, Leung KT, Tong MK. Use of allopurinol in slowing the progression of renal disease through its ability to lower serum uric acid level. Am J Kidney Dis. 2006;47:51–59.
Kanbay M, Ozkara A, Selcoki Y. Effect of treatment of hyperuricemia with allopurinol on blood pressure, creatinine clearance, and proteinuria in patients with normal renal functions. Int Urol Nephrol. 2007;39:1227–1233.
Tsuruta Y, Mochizuki T, Moriyama T. Switching from allopurinol to febuxostat for the treatment of hyperuricemia and renal function in patients with chronic kidney disease. Clin Rheumatol. 2014;33:1643–1648.
Hosoya T, Ohno I, Nomura S. Effects of topiroxostat on the serum urate levels and urinary albumin excretion in hyperuricemic stage 3 chronic kidney disease patients with or without gout. Clin Exp Nephrol. 2014;18:876–884.
Kanbay M, Huddam B, Azak A. A randomized study of allopurinol on endothelial function and estimated glomular filtration rate in asymptomatic hyperuricemic subjects with normal renal function. Clin J Am Soc Nephrol. 2011;6:1887–1894.
Takae K, Nagata M, Hata J. Serum uric acid as a risk factor for chronic kidney disease in a Japanese community—the Hisayama study. Circ J. 2016;80:1857–1862.
Zhang L, Wang F, Wang X. The association between plasma uric acid and renal function decline in a Chinese population-based cohort. Nephrol Dial Transplant. 2012;27:1836–1839.
Kanda E, Muneyuki T, Kanno Y. Uric acid level has a U-shaped association with loss of kidney function in healthy people: a prospective cohort study. PLoS One. 2015;10:e0118031.
Wakasugi M, Kazama JJ, Narita I. Association between hypouricemia and reduced kidney function: a cross-sectional population-based study in Japan. Am J Nephrol. 2015;41:138–146.
Ohta T, Sakano T, Igarashi T, Itami N, Ogawa T, ARF Assocoated with Renal Hypouricemia Research Group. Exercise-induced acute renal failure associated with renal hypouricaemia: results of a questionnaire-based survey in Japan. Nephrol Dial Transplant. 2004;19:1447–1453.
Murakami T, Kawakami H, Fukuda M. Recurrence of acute renal failure and renal hypouricaemia. Pediatr Nephrol. 1993;7:772–773.
Coca SG, Singanamala S, Parikh CR. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 2012;81:442–448.
White WB, Saag KG, Becker MA. Cardiovascular safety of febuxostat or allopurinol in patients with gout. N Engl J Med. 2018;378:1200–1210.
Funding
This study is funded by Fuji Yakuhin Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MK is a consultant for Reason Why Inc. and has received honoraria from KYORIN Pharmaceutical Co.,Ltd., and has received grants from DAIICHI SANKYO COMPANY, LIMITED, Mitsubishi Tanabe Pharma Corporation, and FUJI YAKUHIN CO., LTD. SH has received honoraria from Mitsubishi Tanabe Pharma Corporation, Bayer Holding Ltd., MSD K.K., and Takeda Pharmaceutical Company Limited. YS is a consultant for Novartis Pharma K.K., ONO PHARMACEUTICAL CO., LTD., and Mitsubishi Tanabe Pharma Corporation, and has received honoraria from Otsuka Pharmaceutical Co., Ltd., Mitsubishi Tanabe Pharma Corporation, DAIICHI SANKYO COMPANY, LIMITED, Siemens Healthcare Diagnostics K.K., MSD K.K., Amgen Astellas BioPharma K.K., AstraZeneca K.K., Kowa Pharmaceutical Co., Ltd., Taisho Toyama Pharmaceutical Co., Ltd., Takeda Pharmaceutical Company Limited, TEIJIN PHARMA LIMITED, Nippon Shinyaku Co., Ltd., Novartis Pharma K.K., Bayer Holding Ltd., Medtronic, Inc., MOCHIDA PHARMACEUTICAL CO., LTD., Novo Nordisk Pharma Ltd., and has received grants from Japan Society for the Promotion of Science, The Ministry of Health, Labour and Welfare Scientific Research, Japan Agency for Medical Research and Development Astellas Pharma Inc., Otsuka Pharmaceutical Co., Ltd., Takeda Pharmaceutical Company Limited, TEIJIN PHARMA LIMITED, Bayer Holding Ltd., DAIICHI SANKYO COMPANY, LIMITED, Ltd., Mitsubishi Tanabe Pharma Corporation, Pfizer Japan Inc., Sanofi K.K., Novartis Pharma K.K., MSD K.K., CHUGAI PHARMACEUTICAL CO., LTD., Kyowa Hakko Kirin Co., Ltd., Nihon Medi-Physics Co.,Ltd., ONO PHARMACEUTICAL CO., LTD., Eli Lilly Japan K.K., FUJI YAKUHIN CO., LTD., Sumitomo Dainippon Pharma Co., Ltd. HS has received consulting fee from Pfizer Japan Inc., and has received honoraria from FUJI YAKUHIN CO., LTD. TN lectured a graduate student who was an employee in FUJI YAKUHIN CO., LTD. for 2 years at Nara medical university, and has two patents regarding to hyperuricemia, and has stock for XORT Therapeutics, and has received grant from FUJI YAKUHIN CO., LTD. Remaining authors have declared that no conflict of interest exists.
Ethical approval
The study was conducted in compliance with the Declaration of Helsinki and according to the Clinical Trials Act (Act No. 16 of April 14, 2017) in Japan. The study protocol was approved by the Nara Medical University Certified Review Board on February 22, 2019 (No. nara0008: CRB5180011). The study shall be started at each site after approval of the protocol by the Ethics Review Committee.
Informed consent
The investigators will give a sufficient explanation of the study using explanatory documents to each patient and written informed consent will be obtained from all individual participants included in the study before primary enrollment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kasahara, M., Kuwabara, Y., Moriyama, T. et al. Intensive uric acid-lowering therapy in CKD patients: the protocol for a randomized controlled trial. Clin Exp Nephrol 24, 235–241 (2020). https://doi.org/10.1007/s10157-019-01815-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-019-01815-5