Abstract
Background
The aim of this study was to elucidate the diagnostic value of 18F-fluorodeoxyglucose positron emission tomography (PET)–computed tomography (CT) for lateral pelvic lymph node (LPN) metastasis in rectal cancer treated with preoperative chemoradiotherapy (CRT).
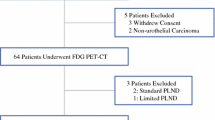
Methods
Eighteen rectal cancer patients with enlarged (≥ 8 mm) LPNs were treated with CRT followed by total mesorectal excision with LPN dissection during 2012–2015. After CRT, LPN maximum standard uptake values (SUVmax) were measured using PET/CT and long diameters of LPNs were measured using CT or magnetic resonance imaging (MRI). LPN size and SUVmax were compared with pathological status in the resected specimen. Radiologically identified nodes were matched with surgically resected nodes by separate examination of 4 lymph nodal regions: internal iliac, obturator, external iliac and common iliac lymph nodes.
Results
In total, 34 LPNs were located by CT or MRI. Metastatic LPNs were significantly larger than non-metastatic LPNs (size, mean ± standard deviation: 13.0 ± 8.3 vs. 4.9 ± 3.5 mm, p < 0.01). SUVmax was determinable for 28 of the LPNs, among which metastatic LPNs were found to have significantly higher SUVmax than non-metastatic LPNs (mean ± standard deviation: 2.2 ± 1.3 vs. 1.2 ± 0.3, p < 0.01). Receiver operating characteristic analysis suggested optimal cutoff values of size = 12 mm which had an accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of 82.1, 70.6, 100, 100, and 68.8%, respectively. An SUVmax = 1.6 had an accuracy, sensitivity, specificity, PPV, and NPV of 85.7, 76.5, 100, 100, and 73.3%, respectively. When LPNs that were ≥ 12 mm in size and/or had an SUV ≥ 1.6, the accuracy, sensitivity, specificity, PPV, and NPV were 92.9, 88.2, 100, 100, and 84.6%, respectively.
Conclusions
After CRT, PET/CT alone or in combination with CT and MRI can predict the presence of metastatic LPN with a high degree of accuracy. PET/CT may be useful in selecting patients with rectal cancer who would benefit from LPN dissection in addition to TME. These results need to be confirmed by larger studies.






Similar content being viewed by others
References
Sugihara K, Moriya Y, Akasu T, Fujita S (1996) Pelvic autonomic nerve preservation for patients with rectal carcinoma. Oncologic and functional outcome. Cancer 78(9):1871–1880
Moriya Y, Sugihara K, Akasu T, Fujita S (1997) Importance of extended lymphadenectomy with lateral node dissection for advanced lower rectal cancer. World J Surg 21(7):728–732
Mori T, Takahashi K, Yasuno M (1998) Radical resection with autonomic nerve preservation and lymph node dissection techniques in lower rectal cancer surgery and its results: the impact of lateral lymph node dissection. Langenbecks Arch Surg 383(6):409–415
Ueno H, Mochizuki H, Hashiguchi Y, Hase K (2001) Prognostic determinants of patients with lateral nodal involvement by rectal cancer. Ann Surg 234(2):190–197
Ueno M, Oya M, Azekura K, Yamaguchi T, Muto T (2005) Incidence and prognostic significance of lateral lymph node metastasis in patients with advanced low rectal cancer. Br J Surg 92(6):756–763
Bacon HE, Dirbas F, Myers TB, Ponce De Leon F (1958) Extensive lymphadenectomy and high ligation of the inferior mesenteric artery for carcinoma of the left colon and rectum. Dis Colon Rectum 1(6):457–464 (discussion 464–455)
Stearns MW Jr, Deddish MR (1959) Five-year results of abdominopelvic lymph node dissection for carcinoma of the rectum. Dis Colon Rectum 2(2):169–172
Georgiou P, Tan E, Gouvas N et al (2009) Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol 10(11):1053–1062
Folkesson J, Birgisson H, Pahlman L, Cedermark B, Glimelius B, Gunnarsson U (2005) Swedish rectal cancer trial: long lasting benefits from radiotherapy on survival and local recurrence rate. J Clin Oncol 23(24):5644–5650
Peeters KC, Marijnen CA, Nagtegaal ID et al (2007) The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg 246(5):693–701
Bosset JF, Collette L, Calais G et al (2006) Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med 355(11):1114–1123
Gerard JP, Conroy T, Bonnetain F et al (2006) Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3-4 rectal cancers: results of FFCD 9203. J Clin Oncol 24(28):4620–4625
Shihab OC, Taylor F, Bees N et al (2011) Relevance of magnetic resonance imaging-detected pelvic sidewall lymph node involvement in rectal cancer. Br J Surg 98(12):1798–1804
Kim TG, Park W, Choi DH et al (2014) Factors associated with lateral pelvic recurrence after curative resection following neoadjuvant chemoradiotherapy in rectal cancer patients. Int J Colorectal Dis 29(2):193–200
Kim TH, Jeong SY, Choi DH et al (2008) Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol 15(3):729–737
Akiyoshi T, Ueno M, Matsueda K et al (2014) Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol 21(1):189–196
Akiyoshi T, Matsueda K, Hiratsuka M et al (2015) Indications for lateral pelvic lymph node dissection based on magnetic resonance imaging before and after preoperative chemoradiotherapy in patients with advanced low-rectal cancer. Ann Surg Oncol 22(Suppl 3):S614–S620
Lu YY, Chen JH, Ding HJ, Chien CR, Lin WY, Kao CH (2012) A systematic review and meta-analysis of pretherapeutic lymph node staging of colorectal cancer by 18F-FDG PET or PET/CT. Nucl Med Commun 33(11):1127–1133
Ishihara S, Kawai K, Tanaka T et al (2017) Oncological outcomes of lateral pelvic lymph node metastasis in rectal cancer treated with preoperative chemoradiotherapy. Dis Colon Rectum 60(5):469–476
Ishihara S, Watanabe T, Fukushima Y et al (2014) Safety and factors contributing to the difficulty of laparoscopic surgery for rectal cancer treated with preoperative chemoradiotherapy. Tech Coloproctol 18(3):247–255
Nagawa H, Muto T, Sunouchi K et al (2001) Randomized, controlled trial of lateral node dissection vs. nerve-preserving resection in patients with rectal cancer after preoperative radiotherapy. Dis Colon Rectum 44(9):1274–1280
Ueno H, Mochizuki H, Hashiguchi Y et al (2007) Potential prognostic benefit of lateral pelvic node dissection for rectal cancer located below the peritoneal reflection. Ann Surg 245(1):80–87
Fujita S, Yamamoto S, Akasu T, Moriya Y (2009) Risk factors of lateral pelvic lymph node metastasis in advanced rectal cancer. Int J Colorectal Dis 24(9):1085–1090
Kobayashi H, Kikuchi A, Okazaki S et al (2015) Diagnostic performance of multidetector row computed tomography for assessment of lymph node metastasis in patients with distal rectal cancer. Ann Surg Oncol 22(1):203–208
Hatano S, Ishida H, Ishiguro T et al (2015) Prediction of metastasis to mesorectal, internal iliac and obturator lymph nodes according to size criteria in patients with locally advanced lower rectal cancer. Jpn J Clin Oncol 45(1):35–42
Brown G, Richards CJ, Bourne MW et al (2003) Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology 227(2):371–377
Bassi MC, Turri L, Sacchetti G et al (2008) FDG-PET/CT imaging for staging and target volume delineation in preoperative conformal radiotherapy of rectal cancer. Int J Radiat Oncol Biol Phys 70(5):1423–1426
Gearhart SL, Frassica D, Rosen R, Choti M, Schulick R, Wahl R (2006) Improved staging with pretreatment positron emission tomography/computed tomography in low rectal cancer. Ann Surg Oncol 13(3):397–404
Kwak JY, Kim JS, Kim HJ, Ha HK, Yu CS, Kim JC (2012) Diagnostic value of FDG-PET/CT for lymph node metastasis of colorectal cancer. World J Surg 36(8):1898–1905
Ozis SE, Soydal C, Akyol C et al (2014) The role of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in the primary staging of rectal cancer. World J Surg Oncol 12:26
Wolthuis AM, Penninckx F, Haustermans K et al (2012) Impact of interval between neoadjuvant chemoradiotherapy and TME for locally advanced rectal cancer on pathologic response and oncologic outcome. Ann Surg Oncol 19(9):2833–2841
Funding
This research is supported by Grants-in-Aid for Scientific Research (A: Grant Number; 16H02672, C: Grant Number; 16K07143, and C: Grant Number; 16K07161) from Japan Society for the Promotion of Science. This research is supported by the Project for Cancer Research and Therapeutic Evolution (P-CREATE, Grant Number: 16cm0106502h0001) from the Japan Agency for Medical Research and Development (AMED).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Toshiaki Watanabe serves as an adviser to Taiho and received a research grant and lecture fees from Taiho. The remaining authors declare that they have no conflict of interest.
Ethical approval
The research was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was given by all patients.
Rights and permissions
About this article
Cite this article
Ishihara, S., Kawai, K., Tanaka, T. et al. Diagnostic value of FDG-PET/CT for lateral pelvic lymph node metastasis in rectal cancer treated with preoperative chemoradiotherapy. Tech Coloproctol 22, 347–354 (2018). https://doi.org/10.1007/s10151-018-1779-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-018-1779-0