Abstract
Background
Psoas muscle mass is a surrogate marker for sarcopenia: a depletion of skeletal muscle mass. This study was conducted to elucidate the prognostic significance of the psoas muscle index (PMI: cross-sectional area of the bilateral psoas muscle at the umbilical level on computed tomography/height2 [cm2/m2]) in patients undergoing surgery for lung squamous cell carcinoma (SCC) and lung adenocarcinoma (ADC).
Methods
One hundred and sixty-five patients with SCC and 556 patients with ADC who underwent R0 resection between 2007 and 2014 were reviewed for analysis. In SCC patients, the mean value (standard deviation) of the PMI was 6.15 (1.49) in men and 4.65 (1.36) in women. Among ADC patients, the PMI was 7.12 (1.60) in men and 5.29 (1.22) in women. Clinicopathological characteristics as well as the survival were evaluated.
Results
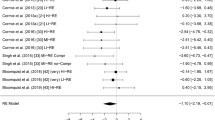
The PMI was associated with the age, body mass index (BMI), and serum albumin. In the multivariable Cox regression analysis, after adjusting for age, BMI, serum albumin, sex, pathological stage, and diffusing capacity for carbon monoxide, the PMI showed a significant association with the overall survival (OS) and disease-free survival (DFS) in SCC patients (hazard ratios 0.50 and 0.56, 95% confidence intervals 0.39–0.65 and 0.45–0.71, respectively). On the other hand, in ADC patients, the PMI had no impact on the OS or DFS.
Conclusions
The PMI was significantly associated with the survival of lung SCC patients, but not of lung ADC patients, suggesting the presence of a previously unidentified relationship between skeletal muscle and lung SCC progression.


Similar content being viewed by others
References
Rosenberg IH (1989) Summary comments. Am J Clin Nutr 50:1231–1233
Okumura S, Kaido T, Hamaguchi Y et al (2015) Impact of preoperative quality as well as quantity of skeletal muscle on survival after resection of pancreatic cancer. Surgery 157:1088–1098
Onesti JK, Wright GP, Kenning SE et al (2016) Sarcopenia and survival in patients undergoing pancreatic resection. Pancreatology 16:284–289
Yaguchi Y, Kumata Y, Horikawa M et al (2017) Clinical significance of area of psoas major muscle on computed tomography after gastrectomy in gastric cancer patients. Ann Nutr Metab 71:145–149
Cornet M, Lim C, Salloum C et al (2015) Prognostic value of sarcopenia in liver surgery. J Visc Surg 152:297–304
Smith AB, Deal AM, Yu H et al (2014) Sarcopenia as a predictor of complications and survival following radical cystectomy. J Urol 191:1714–1720
Park SY, Yoon JK, Lee SJ et al (2017) Prognostic value of preoperative total psoas muscle area on long-term outcome in surgically treated oesophageal cancer patients. Interact CardioVasc Thorac Surg 24:13–19
Yoshikawa T, Takano M, Miyamoto M et al (2017) Psoas muscle volume as a predictor of peripheral neurotoxicity induced by primary chemotherapy in ovarian cancers. Cancer Chemother Pharmacol 80:555–561
Suzuki Y, Okamoto T, Fujishita T et al (2016) Clinical implications of sarcopenia in patients undergoing complete resection for early non-small cell lung cancer. Lung Cancer 101:92–97
Hervochon R, Bobbio A, Guinet C et al (2017) Body mass index and total psoas area affect outcomes in patients undergoing pneumonectomy for cancer. Ann Thorac Surg 103:287–295
Nakamura R, Inage Y, Tobita R et al (2018) Sarcopenia in resected NSCLC: effect on postoperative outcomes. J Thorac Oncol 13:895–903
Sun C, Anraku M, Karasaki T et al (2018) Low truncal muscle area on chest computed tomography: a poor prognostic factor for the cure of early-stage non-small-cell lung cancer. Eur J Cardiothorac Surg 55:414–420
Ozeki N, Fukui T, Taniguchi T et al (2014) Significance of the serum carcinoembryonic antigen level during the follow-up of patients with completely resected non-small-cell lung cancer. Eur J Cardiothorac Surg 45:687–692
Brierley JD, Gospodarowicz MK, Wittekind C (2016) TNM classification of malignant tumours, 8th edn. Wiley-Blackwell, New York
Travis WD, Brambilla E, Burke AP et al (2015) WHO classification of tumours of the lung, pleura, thymus and heart. IARC Press, Lyon
Kurokawa T, Matsuno Y, Noguchi M et al (1994) Surgically curable “early” adenocarcinoma in the periphery of the lung. Am J Surg Pathol 18:431–438
Ozeki N, Kawaguchi K, Fukui T et al (2017) The diffusing capacity of the lung for carbon monoxide is associated with the histopathological aggressiveness of lung adenocarcinoma. Eur J Cardiothorac Surg 52:969–974
Ozeki N, Kawaguchi K, Okasaka T et al (2017) Marginal pulmonary function is associated with poor short- and long-term outcomes in lung cancer surgery. Nagoya J Med Sci 79:37–42
Attaran S, McShane J, Whittle I et al (2012) A propensity-matched comparison of survival after lung resection in patients with a high versus low body mass index. Eur J Cardiothorac Surg 42:653–658
Ozeki N, Fukui T, Kawaguchi K et al (2018) A survival analysis using physique-adjusted tumor size of non-small cell lung cancer. Int J Clin Oncol 23:266–274
Miura K, Hamanaka K, Koizumi T et al (2017) Clinical significance of preoperative serum albumin level for prognosis in surgically resected patients with non-small cell lung cancer: comparative study of normal lung, emphysema, and pulmonary fibrosis. Lung Cancer 111:88–95
Pedersen BK, Febbraio MA (2012) Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat Rev Endocrinol 8:457–465
Takamori S, Toyokawa G, Okamoto T et al (2018) Clinical impact and risk factors for skeletal muscle loss after complete resection of early non-small cell lung cancer. Ann Surg Oncol 25:1229–1236
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ozeki, N., Kawaguchi, K., Fukui, T. et al. Psoas muscle mass in patients undergoing lung cancer surgery: a prognostic difference between squamous cell carcinoma and adenocarcinoma. Int J Clin Oncol 25, 876–884 (2020). https://doi.org/10.1007/s10147-020-01624-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01624-x