Abstract
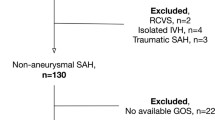
Subarachnoid hemorrhage as bleeding pattern occurs rarely in ruptured arteriovenous malformations (AVM). The aim of the present study is to evaluate different bleeding patterns in hemorrhages due to an AVM and their impact on outcome in terms of risk and treatment stratification. We evaluated 158 patients with ruptured AVMs who were admitted to our neurosurgical department from 2002 to 2017. We compared different bleeding patterns, such as intracerebral hemorrhage (ICH), subarachnoid hemorrhage (SAH), or both (ICH + SAH) and evaluated predictive variables for outcome in the last follow-up. ICH was found in 48.7% of patients, isolated SAH in 20.9% of patients, and both in 30.4% of patients. The mean parenchymal blood volume was 34.5cm3. 38.6% of the patients had AVM-associated aneurysms, mostly located pre-nidal (77%). AVMs with ruptured aneurysms often resulted in ICH with SAH component (p < 0.001) and SAH pattern occurred more often infratentorial (p = 0.003). In a multivariate logistic regression model, poor clinical state on admission (WFNS IV-V) (p < 0.01), eloquence, infratentorial location (p = 0.05), and presence of ICH with SAH component (p = 0.02) were the most relevant predictors of a poor outcome after AVM rupture. Bleeding pattern in AVM hemorrhage depends on angioarchitectural and hemodynamic features and SAH component predicts outcome negatively. AVM-associated pre-nidal aneurysms may harbor a higher risk for rupture and SAH pattern when located infratentorial. Treatment decisions and risk stratifications should be considered in view of these findings.


Similar content being viewed by others
References
Hillman J (2001) Population-based analysis of arteriovenous malformation treatment. J Neurosurg 95(4):633–637. https://doi.org/10.3171/jns.2001.95.4.0633
Kuhmonen J, Piippo A, Väärt K et al (2005) Early surgery for ruptured cerebral arteriovenous malformations. Acta Neurochir Suppl 94:111–114 http://www.ncbi.nlm.nih.gov/pubmed/16060249
Rahme R, Weil AG, Bojanowski MW (2011) Outcome of severe arteriovenous malformation-related intracranial hemorrhage: the importance of cisternal subarachnoid hemorrhage and early seizures. Acta Neurochir 153(4):897–903. https://doi.org/10.1007/s00701-010-0927-8
van Beijnum J, Lovelock CE, Cordonnier C, Rothwell PM, Klijn CJM, al-Shahi Salman R, on behalf of the SIVMS Steering Committee and the Oxford Vascular Study (2009) Outcome after spontaneous and arteriovenous malformation-related intracerebral haemorrhage: population-based studies. Brain. 132(Pt 2):537–543. https://doi.org/10.1093/brain/awn318
Dinc N, Platz J, Tritt S, Quick-Weller J, Eibach M, Wolff R, Berkefeld J, Seifert V, Marquardt G (2018) Posterior fossa AVMs: increased risk of bleeding and worse outcome compared to supratentorial AVMs. J Clin Neurosci 53:171–176. https://doi.org/10.1016/j.jocn.2018.04.010
Fults D, Kelly DL (1984) Natural history of arteriovenous malformations of the brain: a clinical study. Neurosurgery. 15(5):658–662 http://www.ncbi.nlm.nih.gov/pubmed/6504280
Choi JH, Mast H, Sciacca RR, Hartmann A, Khaw AV, Mohr JP, Sacco RL, Stapf C (2006) Clinical outcome after first and recurrent hemorrhage in patients with untreated brain arteriovenous malformation. Stroke. 37(5):1243–1247. https://doi.org/10.1161/01.STR.0000217970.18319.7d
Teasdale GM, Drake CG, Hunt W, Kassell N, Sano K, Pertuiset B, de Villiers JC (1988) A universal subarachnoid hemorrhage scale: report of a committee of the World Federation of Neurosurgical Societies. J Neurol Neurosurg Psychiatry 51(11):1457 http://www.ncbi.nlm.nih.gov/pubmed/3236024
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 19(5):604–607 http://www.ncbi.nlm.nih.gov/pubmed/3363593
Stapf C, Mast H, Sciacca RR, Choi JH, Khaw AV, Connolly ES, Pile-Spellman J, Mohr JP (2006) Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. Neurology. 66(9):1350–1355. https://doi.org/10.1212/01.wnl.0000210524.68507.87
Fennell VS, Martirosyan NL, Atwal GS, Kalani MYS, Ponce FA, Lemole GM Jr, Dumont TM, Spetzler RF (2017) Hemodynamics associated with intracerebral arteriovenous malformations: the effects of treatment modalities. Neurosurgery 83:611–621. https://doi.org/10.1093/neuros/nyx560
Dinc N, Eibach M, Quick-Weller J, Tritt S, Konczalla J, Seifert V, Marquardt G (2017) Special features in AVMs . Impact of Draining Veins on Hemorrhagic Presentation;4
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg 65(4):476–483. https://doi.org/10.3171/jns.1986.65.4.0476
Arnaout OM, Gross BA, Eddleman CS, Bendok BR, Getch CC, Batjer HH (2009) Posterior fossa arteriovenous malformations. Neurosurg Focus:E12. https://doi.org/10.3171/2009.2.FOCUS0914
Batjer H, Samson D (June 1986) Arteriovenous malformations of the posterior fossa. J Neurosurg 64:849–856. https://doi.org/10.3171/jns.1986.64.6.0849
Abla AA, Nelson J, Rutledge WC, Young WL, Kim H, Lawton MT (2014) The natural history of AVM hemorrhage in the posterior fossa: comparison of hematoma volumes and neurological outcomes in patients with ruptured infra- and supratentorial AVMs. Neurosurg Focus:E6. https://doi.org/10.3171/2014.7.FOCUS14211
Locksley HB, Sahs AL, Knowler L (1966) Report on the cooperative study of intracranial aneurysms and subarachnoid hemorrhage. Section II. General survey of cases in the central registry and characteristics of the sample population. J Neurosurg 24(5):922–932. https://doi.org/10.3171/jns.1966.24.5.0922
Perret G, Nishioka H (1966) Report on the cooperative study of intracranial aneurysms and subarachnoid hemorrhage. Section VI. Arteriovenous malformations. An analysis of 545 cases of cranio-cerebral arteriovenous malformations and fistulae reported to the cooperative study. J Neurosurg 25(4):467–490. https://doi.org/10.3171/jns.1966.25.4.0467
Takayama M, Kashiwagi M, Hara K, Matsusue A, Waters B, Ikematsu N, Kubo SI (2017) Basal subarachnoid hemorrhage by rupture of arteriovenous malformation at the cerebellopontine angle. Neuropathology 37(5):441–445. https://doi.org/10.1111/neup.12383
Platz J, Berkefeld J, Singer OC, Wolff R, Seifert V, Konczalla J, Güresir E (2014) Frequency, risk of hemorrhage and treatment considerations for cerebral arteriovenous malformations with associated aneurysms. Acta Neurochir 156(11):2025–2034. https://doi.org/10.1007/s00701-014-2225-3
Stein K-P, Wanke I, Forsting M, Zhu Y, Moldovan AS, Dammann P, Sandalcioglu IE, Sure U (2015) Associated aneurysms in supratentorial arteriovenous malformations: impact of aneurysm size on haemorrhage. Cerebrovasc Dis 39(2):122–129. https://doi.org/10.1159/000369958
Stein K-P, Wanke I, Forsting M, Oezkan N, Huetter BO, Sandalcioglu IE, Sure U (2016) Associated aneurysms in infratentorial arteriovenous malformations: role of aneurysm size and comparison with supratentorial lesions. Cerebrovasc Dis 41(5–6):219–225. https://doi.org/10.1159/000443540
Flores BC, Klinger DR, Rickert KL et al (2014) Management of intracranial aneurysms associated with arteriovenous malformations. Neurosurg Focus 37(3):E11. https://doi.org/10.3171/2014.6.FOCUS14165
Shakur SF, Amin-Hanjani S, Mostafa H, Charbel FT, Alaraj A (2015) Hemodynamic characteristics of cerebral arteriovenous malformation feeder vessels with and without aneurysms. Stroke. 46(7):1997–1999. https://doi.org/10.1161/STROKEAHA.115.009545
Cagnazzo F, Brinjikji W, Lanzino G (2016) Arterial aneurysms associated with arteriovenous malformations of the brain: classification, incidence, risk of hemorrhage, and treatment-a systematic review. Acta Neurochir 158(11):2095–2104. https://doi.org/10.1007/s00701-016-2957-3
Pollock BE, Flickinger JC, Lunsford LD, Bissonette DJ, Kondziolka D (1996) Factors that predict the bleeding risk of cerebral arteriovenous malformations. Stroke 27(1):1–6 http://www.ncbi.nlm.nih.gov/pubmed/8553382
Hung AL, Yang W, Jiang B, Garzon-Muvdi T, Caplan JM, Colby GP, Coon AL, Tamargo RJ, Huang J (2018) The effect of flow-related aneurysms on hemorrhagic risk of intracranial arteriovenous malformations. Neurosurgery. 0(0):1–10. https://doi.org/10.1093/neuros/nyy360
Hartmann A, Mast H, Mohr JP, Koennecke HC, Osipov A, Pile-Spellman J, Duong DH, Young WL (1998) Morbidity of intracranial hemorrhage in patients with cerebral arteriovenous malformation. Stroke. 29(5):931–934 http://www.ncbi.nlm.nih.gov/pubmed/9596237
Lv X, Liu J, Hu X, Li Y (2015) Patient age, hemorrhage patterns, and outcomes of arteriovenous malformation. World Neurosurg 84(4):1039–1044. https://doi.org/10.1016/j.wneu.2015.05.020
Sehba FA, Bederson JB (2006) Mechanisms of acute brain injury after subarachnoid hemorrhage. Neurol Res 28(4):381–398. https://doi.org/10.1179/016164106X114991
Orning J, Amin-Hanjani S, Hamade Y, du X, Hage ZA, Aletich V, Charbel F, Alaraj A (2016) Increased prevalence and rupture status of feeder vessel aneurysms in posterior fossa arteriovenous malformations. J Neurointerv Surg 8(10):1021–1024. https://doi.org/10.1136/neurintsurg-2015-012005
Schmidt NO, Reitz M, Raimund F et al (2011) Clinical relevance of associated aneurysms with arteriovenous malformations of the posterior fossa. Acta Neurochir Suppl 112:131–135. https://doi.org/10.1007/978-3-7091-0661-7_23
Stein K-P, Wanke I, Schlamann M, Dammann P, Moldovan AS, Zhu Y, Sure U, Sandalcioglu IE (2014) Posterior fossa arterio-venous malformations: current multimodal treatment strategies and results. Neurosurg Rev 37(4):619–628. https://doi.org/10.1007/s10143-014-0551-9
Mohr JP, Parides MK, Stapf C, Moquete E, Moy CS, Overbey JR, al-Shahi Salman R, Vicaut E, Young WL, Houdart E, Cordonnier C, Stefani MA, Hartmann A, von Kummer R, Biondi A, Berkefeld J, Klijn CJ, Harkness K, Libman R, Barreau X, Moskowitz AJ, international ARUBA investigators (2014) Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet. 383(9917):614–621. https://doi.org/10.1016/S0140-6736(13)62302-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee (University Hospital Frankfurt) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dinc, N., Won, SY., Quick-Weller, J. et al. Prognostic variables and outcome in relation to different bleeding patterns in arteriovenous malformations. Neurosurg Rev 42, 731–736 (2019). https://doi.org/10.1007/s10143-019-01091-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01091-7