Abstract
Picosecond lasers have a very short pulse duration and a high peak power density. When fractional optical delivery systems are attached to picosecond lasers, they generate an array of concentrated microspots with a high fluence surrounded by areas with a low fluence. This article discusses the histologic characteristics and clinical applications of fractional picosecond laser treatment. Fractional picosecond laser produces laser-induced optical breakdown (LIOB) and laser-induced cavitation (LIC) in the epidermis and dermis respectively, and can encourage skin regeneration and dermal remodeling. It has been shown that fractional picosecond laser has a positive effect on facial photoaging, enlarged facial pores, dyspigmentation, wrinkles, and atrophic scars. Further research is still needed to confirm the benefits of fractional picosecond lasers.
Similar content being viewed by others
Introduction
Laser treatment has long been used in dermatology. The wavelength governs the energy of the photons, while the pulse duration governs the time during which the laser delivers energy to the tissue, and the thermal relaxation time refers to the time required for the heated target tissue to reduce its absorbed energy by 50% through thermal diffusion. The target tissue undergoes specific thermal damage when the pulse duration is shorter than the thermal relaxation time [1]. Picosecond lasers can provide pulse durations between 300 and 900 picoseconds (10–12 s) [2]. In 2012, the FDA approved the first picosecond laser for skin applications (Picosure, Cynosure, Westford, Massachusetts) [1].
Regarding the wavelength, picosecond lasers include the picosecond alexandrite laser (755 nm) and the picosecond neodymium: yttrium‐aluminum‐garnet (Nd:YAG) laser (1064 nm), which delivers 730-nm and 785-nm laser light when used with a laser‐pumped handpiece, or 532 nm if frequency doubled [3].
For skin cosmetology, laser-tissue interactions include photothermolysis, photomechanical (photoacoustic) effect, photochemistry, and photobiomodulation (biostimulation). Photothermolysis involves tissue vaporization or melting through heating by lasers, including the carbon dioxide (CO2) laser or the erbium: yttrium–aluminum-garnet (Er:YAG) laser [1]. The photomechanical or photoacoustic effect occurs when an ultrafast temperature increase generated by a picosecond pulse causes a powerful acoustic shock wave after absorption by a tissue chromophore, producing a tensile stress beyond the tissue fracture threshold [2]. Photochemistry occurs when laser energy is absorbed by the tissue and triggers chemical reactions, which leads to the breaking of chemical bonds between the molecules, and then weakens and destroys the tissue [1]. Photobiomodulation refers to delivering energy to mitochondria, changing the permeability of cell membranes, stimulating fibroblasts to synthesize more collagen and elastin, or regulating the cell signal transduction pathway to upregulate or downregulate the expression of certain genes, rather than producing skin rejuvenation by the effects of tissue heating. Picosecond laser therapy differs from nanosecond laser therapy in that the pulse width is shorter and the peak power density is higher [4]. Nanosecond laser treatment relies mainly on photothermolysis rather than photomechanical effects; however, picosecond lasers rely mainly on photoacoustic destruction [5, 6]. This approach can enhance the energy transmitted to target cells within the lesion, and avoid thermal damage to surrounding tissues[6].
A variety of holographic or diffractive lens arrays can be used to produce fractional picosecond laser energy. These arrays allow the energy to be concentrated within laser microbeams, while neighboring tissue between the microspots is unharmed [2]. Commercially available fractional optical delivery technologies include, diffractive lens arrays (DLA), micro-lens arrays (MLA), and holographic optical arrays [7]. Different optical arrays with different spot sizes have been applied in various picosecond laser devices. DLA technology is employed in the 755-nm alexandrite picosecond laser, and involves closely packed individual hexagonal lenses with a 500 μm pitch [8]. The DLA produces a hexagonal pattern of high-intensity spots surrounded by low-intensity background [8]. The 532-nm and 1064-nm picosecond Nd:YAG laser employ a MLA with a spot size of 4 mm to produce high-intensity zones of tissue damage while preserving the remainder of the surrounding tissue unaffected [9]. This holographic optical array (PicoWay Resolve, Candela) delivers an array of 100 microbeams over a 6 mm × 6 mm area [10].
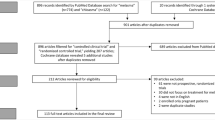
These systems all employ fractional optical delivery devices attached to picosecond lasers [11]. In this article, we review the histological characteristics and clinical applications of fractional picosecond laser treatment (Table 1).
Histological characteristics and mechanisms
Intradermal laser-induced cavitation (LIC) and laser-induced optical breakdown (LIOB) both produce tiny lesions within the dermis and the epidermis [12]. The mechanism of tissue breakdown induced by picosecond laser relies on free electrons, generated by either thermionic emission or chromophore-independent multiphoton absorption [12, 13]. Subsequently in the focus region, the electron density increases to form a plasma, which can more effectively absorb the remaining energy of the laser pulses. The plasma then expands driving the shock wave, and finally the expansion of the vaporized material creates cavitation bubbles, which spread outward into the nearby tissue, resulting in a microcavitation structural response [8, 11].
LIOB and LIC both appear to encourage local skin regeneration and skin remodeling. Habbema et al. [14] observed new collagen production close to the sites of optical breakdown. Similarly, in a study by Brauer [15], increased density and elongation of elastin fibers in the dermis, as well as mucin and collagen III deposition, were observed during the 3-month follow-up in patients treated with 755-nm picosecond laser using a DLA. In response to the LIOB damage in the epidermis, the keratinocytes release a variety of cytokines, chemokines, and growth factors [16]. The rapid development of vacuoles associated with the creation of a LIOB can produce skin pressure fluctuations, which could alter cell signaling and result in dermal remodeling [8]. A study by Ahn et al. has also shown that extravasation of red blood cells could be observed in the papillary dermis after treatment with 1064-nm picosecond laser with MLA, and it was suggested that LIOB could disrupt the neighboring blood vessels to produce a dermal remodeling effect [17]. A similar phenomenon was observed after treatment with a 755-nm picosecond laser with DLA [8].
One study compared the skin thermal effects of laser treatment with fractional or flat optics, and the results showed that compared with flat optics, treatment with fractional optics resulted in more obvious localized epidermal necrosis, which produced significant thermal and clinical effects [18].
It has been found that the depth of a laser-induced lesion and the corresponding laser energy level show an inverse correlation [12]. Higher energy levels result in more superficial intraepidermal LIOBs, whereas lower energy settings result in deeper intradermal LICs [12]. The explanation for this phenomenon is that in intradermal LICs, the low-energy laser beam cannot trigger the threshold for the formation of LIOBs, instead when the high-energy laser beam is greater than the threshold, the energy is focused into LIOBs [12, 19].
The number and size of LIOBs in the epidermis appears to be correlated with the fluence and the number of passes, according to a study by Chang [7]. Similarly, another study showed that the size and number of LIOBs in the epidermis increased as the fluence or the amount of melanin in the skin increased. It was also shown that treatment with higher energy settings produced larger numbers and sizes of LIOBs [8].
Skin rejuvenation
Long-term exposure to ultraviolet radiation can cause facial photoaging (Fig. 1). Irregularities in skin texture, skin laxity, dyspigmentation, wrinkles, and enlarged pores are all signs of skin photoaging [20]. Effective skin rejuvenation is becoming more popular as a clinical treatment, and some studies have used fractional picosecond laser for facial rejuvenation.
Wat et al. reported the first prospective trial to assess the safety and effectiveness of a 755-nm picosecond laser coupled DLA in Chinese patients with photoaging [20]. After six treatment sessions, the skin texture and dyspigmentation scores showed statistically significant improvement; however, there was no significant improvement in pore size or wrinkles [20]. Similarly, in a study by Lin, 755-nm picosecond laser with DLA was used in Asian patients, and the result showed pores and pigmentation had improved at 12 and 20 week follow-up, while at the 1-year follow-up, the improvement in pores had regressed, although pigmentation showed 38% improvement, and wrinkles also improved significantly [21].
Yu et al. treated patients with facial photoaging with 755 nm picosecond alexandrite laser coupled DLA using a fluence of 0.4 J/cm2, an 8-mm spot, and 10 Hz pulse rate for 10 sessions at 2-week intervals. At the 6-month follow-up, there was no significant improvement in wrinkles, while the improvement in pigmentation reached statistical significance compared with the control side [22]. In another study in 46 Asian patients, all patients showed statistically significant improvement in wrinkles, and the pore size improved in more than half the patients after one session of 755 nm picosecond laser with DLA [23]. Ross et al. found that fractional picosecond laser was well tolerated, and wrinkles and improvement in pigmentation were scored as mild to moderate after treatment with the 532- and 1064-nm picosecond laser equipped with a fractional handpiece [24].
The above studies have shown that the fractional laser systems have overall good effects on facial photoaging, while the benefits observed in wrinkles, dyspigmentation, and pore size are considered promising.
Wrinkles
Dierickx et al. used a 755-nm alexandrite picosecond laser with DLA to treat seven cases of facial wrinkles in a split face study [25]. One half of the face received the standard protocol number of pulses while the other side received a higher number of pulses, and both sides showed comparable facial rejuvenation [25]. In another study by Weiss, a picosecond 755-nm alexandrite laser with DLA (fluence of 0.71 J/cm2, 6 mm spot size, 4 treatments at 1 month intervals) was used to treat forty patients with perioral and ocular wrinkles attributed to chronic photodamage [26]. At the 6-month follow-up, the average Fitzpatrick wrinkle score improved from 5.48 at baseline to 3.47, and most patients reported satisfaction with the improvement in wrinkles [26]. Therefore, the 755-nm alexandrite picosecond laser with DLA seems a good choice for treating wrinkles.
Dyspigmentation disorders
Melasma is a pigmentation disorder related to photoaging. Chen et al. used a 755-nm alexandrite picosecond laser with DLA to treat 20 Asian patients with Fitzpatrick skin type IV with melasma. After treatment, the MASI scores showed a significant reduction and an improvement in the skin condition [27]. Wong et al. used fractional 1064-nm picosecond laser to treat melasma, and 70% patients showed moderate to marked improvement [28]. These results suggested the fractional picosecond laser with a DLA could be an effective treatment for melasma.
Post-inflammatory hyperpigmentation (PIH) is a common complication of inflammatory skin diseases [4]. In a study by Ren, they treated PIH patients with a 755-nm picosecond laser with DLA, and the pigmented lesions showed 50–75% improvement at the 3-year follow-up [4]. The results suggested the 755-nm picosecond laser with DLA could be a long-term effective treatment for PIH in Asian skin [4].
Enlarged facial pores
One study from Thailand used the 1064-nm picosecond laser with MLA to treat patients with enlarged pores. The results showed that after a single fractional picosecond 1064-nm laser treatment, the number of enlarged pores was 15.13% lower, while the diameter of the facial pores was unchanged [29]. In another study in Asians with enlarged pores treated with three monthly sessions of 1064-nm picosecond laser with MLA, there was a 30% decrease in average pore size at the 6-month follow-up [30]. The efficacy of fractional picosecond laser in the treatment of enlarged pores seems to need further study.
Treatment for atrophic skin lesions
Atrophic acne scars
Hypertrophic, atrophic, and keloid scars are the three different types of acne scars [15]. There are now several approaches to treat atrophic acne scars. Brauer et al. reported the efficacy of the 755-nm picosecond laser with DLA to treat atrophic acne scars [15]. They treated patients with a 755-nm picosecond laser with DLA (fluence of 0.71 J/cm2, 6 mm spot size, six sessions at 4- to 8-week intervals), and reported a mean scar improvement of 24.3% after the final treatment [15]. In a study by Dierickx et al., they treated 3 patients using the 755-nm picosecond laser with DLA, and they randomly assigned half of the face to be treated with the standard pulse coverage, while the other half of the face received 1.7 times more pulses [25]. The standard pulse side showed good to excellent improvement, while the high pulse side had very good to excellent improvement [25]. Huang reported that the 755-nm picosecond laser with DLA over several sessions was successful in treating atrophic acne scars in Asian patients [31]. A study by Zhang et al. [32] reported similar effects. Zhang treated 20 Chinese patients with a picosecond alexandrite laser with DLA over 3 treatment sessions, and suggested it effectively improved scar appearance and texture, without any serious adverse effects.
In Asian patients, a 1064-nm picosecond laser with MLA was used for treating atrophic acne scars. The skin surface roughness and the scars showed significant improvement, with the erythematous and hyperpigmented appearance improving at the same time [33]. Similarly, in patients from Thailand, the 1064-nm picosecond laser with MLA has also shown good results. All the patients’ acne scars were reduced significantly after one treatment session [29]. These clinical studies suggest that the fractional picosecond laser has a good effect on acne scars.
Striae distensae
Striae distensae (or stretch marks) is another type of atrophic dermal scar, and is often caused by rapid changes in body weight, long-term exposure to steroids, or other endocrine conditions [34]. In a prospective study by Kaewkes, they treated twenty female patients with abdominal striae alba using a 1064-nm picosecond laser with a MLA handpiece using a fluence of 0.6 J/cm2, 8 mm spot size, over four sessions [34]. The results showed significant improvement in skin texture and striae, and only two patients developed PIH [34]. Fractional 1064-nm picosecond laser could be effective in treating striae distensae in dark skin types.
Comparison of picosecond laser with other laser treatments
Tanghetti et al. compared the clinical and histological characteristics of skin lesions produced by a picosecond 532-nm and 1064-nm Nd:YAG laser with a holographic optic, or by a 755-nm picosecond laser with a DLA [35] (Table 2). Their study revealed that both devices caused skin vacuoles. The fractional 532-nm and 1064-nm picosecond laser caused cutaneous hemorrhages by damaging and heating the superficial blood vessels, while the 755-nm laser was absored by melanin and showed superior safety by avoiding any damage to the vasculature [35].
A prospective split face study compared the 755-nm picosecond laser with DLA and the same laser used in a fullbeam mode for treating melasma. They found that all patients showed significant pigment clearance without any significant difference between the treatment sides. Compared to the fractional laser, the full-beam 755-nm picosecond laser showed a lower incidence of PIH, less downtime, and less pain during treatment [36].
A controlled study compared the effectiveness and safety of a non-ablative fractional laser (NAFL) or a 1064-nm Nd:YAG picosecond laser with a diffractive optical element (P-DOE) for treating acne scars [37]. In the treatment of acne scars in Asian patients, the P-DOE provided better clinical results, fewer side effects, and more improvement at the follow-up visit [37].
Similarly, another study compared the fractional Nd:YAG 1064-nm picosecond laser with a fractional lens array (FLA) with the fractional 1550-nm erbium fiber laser for treating acne scars [38]. The clinical scores with both devices showed significant improvement from baseline; however, there was no significant difference between the two devices. More pinpoint bleeding as a side effect was observed with the picosecond laser, whereas more pain was reported with the erbium laser [38].
Fractional carbon dioxide laser (FxCO2) was compared with fractional picosecond 1064-nm laser in a study to treat acne scars [39]. The results showed that FxCO2 was as effective as fractional picosecond 1064-nm laser, but the latter was accompanied by a lower incidence of PIH [39].
Combinations of picosecond laser with other treatments
Combination treatment for facial rejuvenation
Theoretically, soft tissue inflammation following laser treatment could affect the diffusion of botulinum neurotoxim to undesirable locations. Therefore, Wang et al. designed a study to test the combination of 755-nm picosecond laser with DLA plus botulinum toxin applied for facial rejuvenation [40]. There were no reported side effects from neurotoxin spreading, and the combined therapy could improve the efficacy with possible synergistic effects [40].
The 755-nm picosecond laser with DLA could treat wrinkles and fine lines, while the 1060-nm laser has been used for non-invasive lipolysis, and could improve the appearance of lax tissue [41]. Wang et al. combined the 755-nm picosecond laser with DLA with the 1,060-nm laser for submental lipolysis to treat patients with facial aging. Their results demonstrated that the combination of 1,060-nm laser submental lipolysis plus 755-nm picosecond laser with DLA could improve the overall clinical aesthetic effects [41].
Soft tissue fillers and laser treatments are frequently employed for facial rejuvenation [42]. Because laser treatment may change the filler properties, patient safety and filler efficacy could be a concern. Therefore, Wang et al. designed a retrospective study and found that there were no recorded adverse effects among 406 single-session treatments in patients receiving 755-nm picosecond laser with DLA combined with fillers [42].
Combination treatments for benign pigmented lesions
In a split face study by Chalermchai, they treated melasma patients with fractional picosecond 1064-nm laser plus 4% hydroquinone on the intervention side, and 4% hydroquinone cream alone on the control side[43]. The intervention side showed greater reductions in melasma area severity index scores compared to 4% hydroquinone cream alone, and it was suggested that fractional picosecond 1064-nm laser could be an effective treatment for melasma.
Various methods have been tested to remove unwanted tattoos, and there was a study to compare tattoo removal results with fractionated 1064-nm picosecond laser plus unfractional 1064-nm picosecond laser, with unfractional 1064-nm picosecond laser alone [44]. The combination side showed greater clearance scores and fewer adverse events than the unfractional 1064-nm picosecond laser alone; as a result, they suggested that combination therapy may be a good method for tattoo removal [44].
Combination treatments for scars
Kim combined the 1064-nm picosecond laser with MLA and hyaluronic acid fillers (HAF) to treat acne scars and achieved good results. Their histological findings suggested that the laser did not disrupt the pre‐injected HAF, and also induced significant neocollagenesis [45].
In a study by Feng et al., an intense pulsed light (IPL) device was used on its own to treat one-half of the face, while the other half was treated by fractional 1064-nm Nd:YAG picosecond laser (FxPico) combined with IPL. The combination showed greater pore count reduction and scar improvement, and they suggested that FxPico combined with IPL could be a better treatment option for atrophic acne scars [46].
Rho et al. reported a patient with a full-thickness laceration scar who was treated with 1064-nm Nd:YAG laser with MLA combined with polynucleotide gel injection, and reported a significant clinical improvement [47].
Conclusion
Clinical studies have reported that the high-intensity micro-injury zones caused by fractional picosecond laser can improve atrophic scars, enlarged facial pores, dyspigmentation, and wrinkles (Fig. 2). Combination therapy with fractional picosecond laser does not affect the efficay of other treatments, and may show additive or synergistic benefits (Table 3). More clinical research on different disorders treated with fractional picosecond laser is needed to improve our understanding of the overall benefits of fractional picosecond laser.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- Nd: YAG :
-
Neodymium: yttrium‐aluminum‐garnet
- CO 2 :
-
Carbon dioxide
- Er: YAG :
-
Erbium: yttrium–aluminum-garnet
- DLA :
-
Diffractive lens arrays
- MLA :
-
Micro-lens arrays
- LIOB :
-
Laser-induced optical breakdown
- LIC :
-
Laser-induced cavitation
- PIH :
-
Post-inflammatory hyperpigmentation
- NAFL :
-
Non-ablative fractional laser
- P-DOE :
-
Picosecond laser with a diffractive optical element
- FLA :
-
Fractional lens array
- FxCO 2 :
-
Fractional carbon dioxide laser
- HAF :
-
Hyaluronic acid fillers
- IPL :
-
Intense pulsed light
- FxPico :
-
Fractional 1064-nm Nd: YAG picosecond laser
References
Freedman JR, Kaufman J, Metelitsa AI, Green JB (2014) Picosecond lasers the next generation of short-pulsed lasers. Sem Cutan Med Surg 33:164–168. https://doi.org/10.12788/j.sder.0117
Wu DC, Goldman MP, Wat H, Chan HHL (2021) A systematic review of picosecond laser in dermatology: evidence and recommendations. Lasers Surg Med 53:9–49. https://doi.org/10.1002/lsm.23244
Lee SJ, Han HS, Hong JK, Park KY, Seo SJ (2020) Successful treatment of pigmentary disorders in asians with a novel 730-nm picosecond laser. Lasers Surg Med 52:923–927. https://doi.org/10.1002/lsm.23261
Ren R, Bao S, Qian W, Zhao H (2021) 755-nm alexandrite picosecond laser with a diffractive lens array or zoom handpiece for post-inflammatory hyperpigmentation: two case reports with a three-year follow-up. Clin Cosmet Investig Dermatol 14:1459–1464. https://doi.org/10.2147/ccid.S323872
Kasai K (2017) Picosecond laser treatment for tattoos and benign cutaneous pigmented lesions (secondary publication). Laser therapy 26:274–281. https://doi.org/10.5978/islsm.17-RE-02
Dong W, Wang N, Yuan X, Zhang W (2021) Treatment of pigmentary disorders using picosecond laser in Asian patients: a meta-analysis and systematic review. Dermatologic therapy 34:e14709. https://doi.org/10.1111/dth.14709
Chang YS, Yang TH, Li CN (2022) Histology changes of in vivo human skin after treatment with fractional 1064 nm Nd:YAG picosecond laser in different energy settings. Lasers Med Sci 37:2087–2092. https://doi.org/10.1007/s10103-021-03396-w
Tanghetti EA (2016) The histology of skin treated with a picosecond alexandrite laser and a fractional lens array. Lasers Surg Med 48:646–652. https://doi.org/10.1002/lsm.22540
Oc K, Cho SB, Chung HJ (2021) Wound healing profile after 1064- and 532-nm picosecond lasers with microlens array of in vivo human skin. Lasers Surg Med 53:1059–1064. https://doi.org/10.1002/lsm.23390
Balu M, Lentsch G, Korta DZ, König K, Kelly KM, Tromberg BJ et al (2017) In vivo multiphoton-microscopy of picosecond-laser-induced optical breakdown in human skin. Lasers Surg Med 49:555–562. https://doi.org/10.1002/lsm.22655
Chen SX, Cheng J, Watchmaker J, Dover JS, Chung HJ (2022) Review of lasers and energy-based devices for skin rejuvenation and scar treatment with histologic correlations. Dermatol Surg 48:441–448. https://doi.org/10.1097/dss.0000000000003397
Yeh YT, Peng JH, Peng P (2020) Histology of ex vivo skin after treatment with fractionated picosecond Nd:YAG laser in high and low-energy settings. J Cosmetic Laser Ther 22:43–47. https://doi.org/10.1080/14764172.2019.1710536
Chung HJ, Lee HC, Park J, Childs J, Hong J, Kim H et al (2019) Pattern analysis of 532- and 1064-nm microlens array-type, picosecond-domain laser-induced tissue reactions in ex vivo human skin. Lasers Med Sci 34:1207–1215. https://doi.org/10.1007/s10103-018-02711-2
Habbema L, Verhagen R, Van Hal R, Liu Y, Varghese B (2012) Minimally invasive non-thermal laser technology using laser-induced optical breakdown for skin rejuvenation. J Biophotonics 5:194–199. https://doi.org/10.1002/jbio.201100083
Brauer JA, Kazlouskaya V, Alabdulrazzaq H, Bae YS, Bernstein LJ, Anolik R et al (2015) Use of a picosecond pulse duration laser with specialized optic for treatment of facial acne scarring. JAMA Dermatol 151:278–284. https://doi.org/10.1001/jamadermatol.2014.3045
Werner S, Krieg T, Smola H (2007) Keratinocyte-fibroblast interactions in wound healing. J Invest Dermatol 127:998–1008. https://doi.org/10.1038/sj.jid.5700786
Ahn HJ, Hye Suh D, Kang IH, Jun Lee S, Kyung Shin M, Yong Song K (2021) Interaction of skin with fractional picosecond laser in Asian patients. J Clin Aesthetic Dermatol 14:14–15
Tanghetti EA, Tartar DM (2016) Comparison of the cutaneous thermal signatures over twenty-four hours with a picosecond alexandrite laser using a flat or fractional optic. J Drugs Dermatolo: JDD 15:1347–1352
Qu Y, Wang L, Zhou P, Zhang W (2020) Efficient picosecond laser for tattoo removal in rat models. Med Sci Monit 26:e924583. https://doi.org/10.12659/msm.924583
Wat H, Yee-Nam Shek S, Yeung CK, Chan HH (2019) Efficacy and safety of picosecond 755-nm alexandrite laser with diffractive lens array for non-ablative rejuvenation in Chinese skin. Lasers Surg Med 51:8–13. https://doi.org/10.1002/lsm.23014
Lin ET, Chiang HM, Lin BS, Huang YH, Chang CC (2021) Photoaging reversibility in Asian patients with melasma treated using picosecond lasers with a diffractive lens array: a 1-year prospective observational cohort study. Dermatol Surg 47:e10–e14. https://doi.org/10.1097/dss.0000000000002405
Yu W, Zhu J, Yu W, Shang Y, Lyu D, Lin X et al (2021) Three-year results of facial photoaging in asian patients after alexandrite 755 nm picosecond laser with diffractive lens array: a split-face, single-blinded, randomized controlled comparison. Lasers Surg Med 53:1065–1072. https://doi.org/10.1002/lsm.23393
Sun Y, Yang TT, Chih PL, Chen YC, Lan CE (2022) Favorable effect after single treatment session of 755-nm-picosecond laser with a diffractive optic lens on facial wrinkles and pore size in Asians. J Cosmet Dermatol. https://doi.org/10.1111/jocd.14810
Ross EV, Tidwell WJ, Guss L, Sutton AV (2022) Study of a 532/1064 fractional picosecond laser for facial rejuvenation. Dermatol Surg 48:109–113. https://doi.org/10.1097/dss.0000000000003229
Dierickx C (2018) Using normal and high pulse coverage with picosecond laser treatment of wrinkles and acne scarring: long term clinical observations. Lasers Surg Med 50:51–55. https://doi.org/10.1002/lsm.22763
Weiss RA, McDaniel DH, Weiss MA, Mahoney AM, Beasley KL, Halvorson CR (2017) Safety and efficacy of a novel diffractive lens array using a picosecond 755 nm alexandrite laser for treatment of wrinkles. Lasers Surg Med 49:40–44. https://doi.org/10.1002/lsm.22577
Chen YT, Lin ET, Chang CC, Lin BS, Chiang HM, Huang YH et al (2019) Efficacy and safety evaluation of picosecond alexandrite laser with a diffractive lens array for treatment of melasma in Asian patients by VISIA imaging system. Photobiomodulation, Photomed Laser Surg 37:559–566. https://doi.org/10.1089/photob.2019.4644
Wong CSM, Chan MWM, Shek SYN, Yeung CK, Chan HHL (2021) Fractional 1064 nm picosecond laser in treatment of melasma and skin rejuvenation in Asians, a prospective study. Lasers Surg Med 53:1032–1042. https://doi.org/10.1002/lsm.23382
Puaratanaarunkon T, Asawanonda P (2022) Efficacy of a one-session fractional picosecond 1064-nm laser for the treatment of atrophic acne scar and enlarged facial pores. J Cosmet Laser ther 1–5. https://doi.org/10.1080/14764172.2022.2055079
Palawisuth S, Manuskiatti W, Apinuntham C, Wanitphakdeedecha R, Cembrano KAG (2022) Quantitative assessment of the long-term efficacy and safety of a 1064-nm picosecond laser with fractionated microlens array in the treatment of enlarged pores in Asians: a case-control study. Lasers Surg Med 54:348–354. https://doi.org/10.1002/lsm.23449
Huang CH, Hsieh FS, Chang HC, Peng JH, Peng HP (2019) 755 nm picosecond laser for facial atrophic scar-case reports of long-term clinical efficacy following up. J Cosmet Dermatol 18:778–782. https://doi.org/10.1111/jocd.12925
Zhang M, Fang J, Wu Q, Lin T (2020) Evaluation of the safety and efficacy of a picosecond alexandrite laser with DLA for acne scars in Chinese patients. Lasers Surg Med 52:176–181. https://doi.org/10.1002/lsm.23177
Manuskiatti W, Punyaratabandhu P, Tantrapornpong P, Yan C, Cembrano KAG (2021) Objective and long-term evaluation of the efficacy and safety of a 1064-nm picosecond laser with fractionated microlens array for the treatment of atrophic acne scar in Asians. Lasers Surg Med 53:899–905. https://doi.org/10.1002/lsm.23368
Kaewkes A, Manuskiatti W, Cembrano KA, Wanitphakdeedecha R (2022) Treatment of abdominal striae distensae in Fitzpatrick skin types IV to V using a 1064-nm picosecond laser with a fractionated microlens array. Lasers Surg Med 54:129–137. https://doi.org/10.1002/lsm.23471
Tanghetti MdE, Jennings J (2018) A comparative study with a 755 nm picosecond Alexandrite laser with a diffractive lens array and a 532 nm/1064 nm Nd:YAG with a holographic optic. Lasers Surg Med 50:37–44. https://doi.org/10.1002/lsm.22752
Manuskiatti W, Yan C, Tantrapornpong P, Cembrano KAG, Techapichetvanich T, Wanitphakdeedecha R (2021) A prospective, split-face, randomized study comparing a 755-nm picosecond laser with and without diffractive lens array in the treatment of melasma in Asians. Lasers Surg Med 53:95–103. https://doi.org/10.1002/lsm.23312
Kwon HH, Yang SH, Cho YJ, Shin E, Choi M, Bae Y et al (2020) Comparison of a 1064-nm neodymium-doped yttrium aluminum garnet picosecond laser using a diffractive optical element vs. a nonablative 1550-nm erbium-glass laser for the treatment of facial acne scarring in Asian patients: a 17-week prospective, randomized, split-face, controlled trial. J Eur Acad Dermat Venereol: JEADV 34:2907–2913. https://doi.org/10.1111/jdv.16643
Chayavichitsilp P, Limtong P, Triyangkulsri K, Pratumchart N (2020) Comparison of fractional neodymium-doped yttrium aluminum garnet (Nd:YAG) 1064-nm picosecond laser and fractional 1550-nm erbium fiber laser in facial acne scar treatment. Lasers Med Sci 35:695–700. https://doi.org/10.1007/s10103-019-02891-5
Sirithanabadeekul P, Tantrapornpong P, Rattakul B, Sutthipisal N, Thanasarnaksorn W (2021) Comparison of fractional picosecond 1064-nm laser and fractional carbon dioxide laser for treating atrophic acne scars: a randomized split-face trial. Dermatol Surg 47:e58–e65. https://doi.org/10.1097/dss.0000000000002572
Wang JV, Albornoz CA, Anolik R, Geronemus RG (2021) Single-session treatment with botulinum toxin and 755-nm picosecond laser with diffractive lens array: a 5-year safety review. Dermatol Surg 47:1302–1303. https://doi.org/10.1097/dss.0000000000003112
Wang JV, Christman MP, Feng H, Pomerantz H, Lederhandler M, Geronemus RG (2021) Paired facial treatment with 755nm picosecond laser with diffractive lens array and 1060nm laser lipolysis of the submentum: an open-label prospective trial. J Cosmet Dermatol 20:3492–3497. https://doi.org/10.1111/jocd.14397
Wang JV, Ugonabo N, Anolik R, Geronemus RG (2021) Pairing facial fillers with 755-nm picosecond laser with diffractive lens array: a 5-year safety evaluation of single-session treatments. Dermatol Surg 47:1305–1307. https://doi.org/10.1097/dss.0000000000003109
Chalermchai T, Rummaneethorn P (2018) Effects of a fractional picosecond 1,064 nm laser for the treatment of dermal and mixed type melasma. J Cosmet Laser Ther 20:134–139. https://doi.org/10.1080/14764172.2017.1376098
Sirithanabadeekul P, Vongchansathapat P, Sutthipisal N, Thanasarnaksorn W, Suwanchinda A (2022) Outcomes of 1064-nm picosecond laser alone and in combination with fractional 1064-nm picosecond laser in tattoo removal. J Cosmet Dermatol 21:2832–2839. https://doi.org/10.1111/jocd.15031
Kim JE, Hong JY, Lee HJ, Lee SY, Kim HJ (2020) Picosecond-domain fractional laser treatment over hyaluronic acid fillers: in vivo and clinical studies. Lasers Surg Med 52:928–934. https://doi.org/10.1002/lsm.23254
Feng H, Wu Y, Jiang M, Luo X, Yan S, Lu Z (2021) The efficacy and safety of fractional 1064 nm Nd:YAG picosecond laser combined with intense pulsed light in the treatment of atrophic acne scar: a split-face study. Lasers Surg Med 53:1356–1363. https://doi.org/10.1002/lsm.23428
Rho N, Chung ST (2018) Treatment of a full-thickness laceration scar on the forehead using a 1,064-nm fractional picosecond laser and polynucleotide gel injection. Medical Lasers 7:88–90. https://doi.org/10.25289/ML.2018.7.2.88
Funding
This work was supported by National Natural Science Foundation of China (81903226).
Author information
Authors and Affiliations
Contributions
YanJun Zhou performed the literature search and data analysis, and wrote the first draft of the article. Michael R Hamblin critically revised the manuscript for content and meaning. Xiang Wen had the original idea for the article and critically revised the work.
Corresponding author
Ethics declarations
Ethics approval
This is a review article of compliance with ethical standards.
Competing interests
MRH declares the following potential conflicts of interest. Scientific Advisory Boards: Transdermal Cap Inc, Cleveland, OH; Hologenix Inc. Santa Monica, CA; Vielight, Toronto, Canada; JOOVV Inc, Minneapolis-St. Paul MN; Sunlighten, Kansas City, MO; Consulting; USHIO Corp, Japan; Sanofi-Aventis Deutschland GmbH, Frankfurt am Main, Germany; Klox Asia, Guangzhou, China. Stockholding: Niraxx Light Therapeutics, Inc., Irvine CA; JelikaLite Corp, New York NY. All other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, Y., Hamblin, M.R. & Wen, X. An update on fractional picosecond laser treatment: histology and clinical applications. Lasers Med Sci 38, 45 (2023). https://doi.org/10.1007/s10103-022-03704-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-022-03704-y