Abstract
We investigated the positivity rate, the detection rates for non-covered pathogens and the therapeutic impact of microbiological samples (MS) in community-acquired pneumonia (CAP), nursing home-acquired pneumonia (NHAP) and hospital-acquired pneumonia (HAP) in elderly hospitalised patients. Patients aged 75 years and over with pneumonia and hospitalised between 1/1/2013 and 30/6/2013 in the departments of medicine (5) and intensive care (1) of our university hospital were included. Microbiological findings, intra-hospital mortality and one-year mortality were recorded. Among the 217 patients included, there were 138 CAP, 56 NHAP and 23 HAP. MS were performed in 89.9, 91.1 and 95.6 % of CAP, NHAP and HAP, respectively. Microbiological diagnosis was made for 29, 11.8 and 27.3 % of patients for CAP, NHAP and HAP, respectively (p = 0.05). Non-covered pathogens were detected for 8 % of CAP, 2 % of NHAP and 13.6 % of HAP (p = 0.1). The antimicrobial spectrum was significantly more frequently reduced when the MS were positive (46.7 % vs. 10.8 % when MS were negative, p = 10−7). The MS positivity rate was significantly lower in NHAP than in CAP and HAP. MS revealed non-covered pathogens in only 2 % of NHAP. These results show the poor efficiency and weak clinical impact of MS in the management of pneumonia in hospitalised older patients and suggest that their use should be rationalised.
Similar content being viewed by others
Introduction
Pneumonia is the most common cause of hospitalisation in nursing home residents [1]. Its mortality rate among older individuals is 30 %, and even higher in institutions [2].
Microbiological diagnosis of pneumonia is difficult. Because multidrug-resistant bacteria are often suspected, microbiological samples (MS) are recommended in patients hospitalised for nursing home-acquired pneumonia (NHAP) and hospital-acquired pneumonia (HAP) [3]. For community-acquired pneumonia (CAP), MS are optional in American recommendations [4], but European guidelines recommend systematic blood cultures, sputum samples and pneumococcal (PUA) and Legionella urinary antigen (LUA) [5]. However, few studies have considered the usefulness and efficiency of MS for pneumonia in real hospital conditions, especially among elderly patients and in NHAP.
Thus, we compared the efficiency and clinical impact of MS in the hospital management of CAP, NHAP and HAP.
Methods
Participants
The clinical records of patients aged 75 years and over hospitalised for pneumonia in five departments of medicine [geriatrics (GMD), pneumology, infectious diseases (IDD), two internal medicine (IMD)] and one intensive care unit (ICU) of our university hospital between 1/1/2013 and 30/06/2013 were retrospectively reviewed.
The following criteria were required: (1) two or more of the following signs: new cough, sputum production, dyspnoea, pleuritic pain, abnormal temperature (<35.6 °C or > 37.8 °C), altered breathing sounds on auscultation and (2) a new infiltrate on chest imaging. Ventilator-associated pneumonia was not included. Pneumonia was considered CAP or NHAP if the first clinical signs appeared at home or at the nursing home. Pneumonia was considered late-onset HAP if the first clinical signs appeared at least 5 days after admission [6].
The study was conducted in accordance with the Declaration of Helsinki and national standards. Because this was an observational study, no written consent or approval from the Ethics Committee was necessary.
Recorded data
For each subject, we recorded age, sex, residential status, World Health Organization (WHO) performance status score [7], underlying diseases, Charlson comorbidity index (CCI) [8], age-adjusted CCI (ACCI) [9], history of hospitalisation in the past 6 months, Pneumonia Severity Index (PSI) [10], CURB-65 score [11], MS collected at admission, probabilistic antibiotic treatment (PAT) at admission, antibiotic modification during hospitalisation, in-hospital mortality, one-year mortality, hospitalisation duration and rehospitalisation rate at 6 months.
Microbiological criteria
Criteria defining positive microbiological diagnosis were as follows and in accordance with the thresholds defined elsewhere [12]: (1) positive bacterial blood culture in the absence of an apparent extrapulmonary focus, (2) positive PUA and LUA, (3) positive culture of a protected specimen brush, bronchoalveolar lavage culture or fibroaspiration sample, defined as invasive procedures (IP), (4) predominant bacteria isolated from cultures of a purulent sputum sample, (5) positive serology against Chlamydia pneumoniae, Mycoplasma pneumoniae or Legionella pneumophila, and (6) positive immunofluorescence assay or positive polymerase chain reaction (PCR) for respiratory viruses, i.e. influenza viruses A and B, parainfluenza viruses, respiratory syncytial virus (RSV), adenovirus, metapneumovirus (MPV), defined as virological samples.
Microbiological identification and susceptibility testing to antibiotics were performed by standard methods for blood, sputum and IP sample cultures [12]. Cases with positive PUA were considered sensitive, except for macrolides (unknown sensitivity). Cases with positive LUA or positive intracellular bacteria serology were considered resistant, except for macrolides and fluoroquinolones (considered sensitive).
Bacteria resistant to the PAT were considered non-covered pathogens, as were all pathogens for which a curative treatment exists but was not given, including non-treated influenza viruses.
Data analysis
The three groups (CAP, NHAP and HAP) were compared for all recorded data. Continuous variables were expressed as means and interquartile ranges, and categorical variables as numbers and percentages. Continuous variables were compared using the Mann–Whitney U-test, and categorical variables using the Chi-square and Fisher’s tests, when appropriate. Statistical significance was defined for p < 0.05.
Results
Patient characteristics
A total of 217 patients were included. There were 218 admissions to departments of medicine: 89 to IMDs, 80 to GMD, 32 to the pneumology department and 17 to IDD; 39 patients were admitted to the ICU. Among these 217 patients, 138 suffered from CAP, 56 had NHAP and 23 HAP. Patients with NHAP were significantly older than those with CAP or HAP (mean ages 88.9, 83.9 and 86.9 years, respectively, p = 0.0007) and WHO performance status scores were significantly worse (WHO score ≥3 in. respectively, 94.4, 53.4 and 82.6 % of patients, p = 10−8). The CCI, ACCI and CURB-65 severity score were not significantly different in the three groups. The PSI was similar in the NHAP and CAP groups but significantly higher in the HAP group (respective mean scores 134.6, 130.8 and 148.4, p = 0.05). Admission to the ICU was less frequent for NHAP than for CAP and HAP (p = 0.04) (Table 1).
The PAT was more frequently monotherapy for NHAP (96.5 %) compared with HAP (85.7 %) or CAP (77.9 %) (p = 0.003). Amoxicillin–clavulanate was the most frequent PAT in all groups (51.8 % of NHAP, 44.1 % of CAP and 42.9 % of HAP), followed by third-generation cephalosporins (3GC).
Microbiological diagnosis
MS were taken for 90.8 % of patients. The most frequent MS were blood cultures (81.6 %), LUA (60.4 %) and PUA (58.1 %). The sampling rates were similar in the three groups except for PUA, virological samples and bacterial serologies. Altogether, MS were taken in 89.9 % of CAP, 91.1 % of NHAP and 95.7 % of HAP (p = 0.8), and were positive in 29, 11.8 and 27.3 %, respectively (p = 0.05) (Table 2).
Streptococcus pneumoniae was the most frequently detected pathogen (8.7 %), followed by enterobacteria (8.1 %, not extended-spectrum beta-lactamase). Gram-negative bacilli (GNB) were significantly less frequent in NHAP (2 %) than in CAP (16.3 %) and HAP (13.6 %) (p = 0.01) (Table 3).
Antibiotic sensitivity
There was a trend towards greater sensitivity to antibiotics in the NHAP group. The difference was significant for amoxicillin (83.3 % of pathogens vs. 26.7 % and 25 % for the CAP and HAP groups, respectively, p = 0.03) (Table 4).
A total of 52.8 % of the documented pathogens of CAP, 83.3 % of NHAP and 60 % of HAP were covered by the PAT. Non-covered pathogens were mostly GNB (n = 11, including three Legionella pneumophila, three Enterobacter sp., two Pseudomonas aeruginosa, two Morganella morganii, one Stenotrophomonas maltophilia), two coagulase-negative methicillin-resistant staphylococci, one Aspergillus fumigatus and one influenza A virus.
For all of the patients with MS, the detection of non-covered pathogens concerned 8 % of the CAP, 2 % of the NHAP and 13.6 % of the HAP (p = 0.1).
Comparative effectiveness of microbiological samples
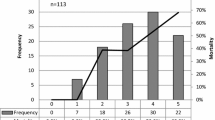
The positivity rates of MS were as follows: 40 % for IP, 39.4 % for sputum samples, 14 % for virological samples, 8.7 % for PUA, 7.9 % for blood cultures, 3.1 % for LUA and 0 % for bacterial serologies (Table 2).
Non-covered pathogens were revealed by four blood cultures (2.3 %), four sputum samples (12.1 %), three LUA (2.3 %), three IP (12 %), one virological sample (2.3 %) and no PUA or bacterial serologies.
Impact of microbiological samples on antibiotic therapy and outcome
In the total population and for the three types of pneumonia, MS positivity had no significant impact on the PAT (modification or broadening).
In the total population, the antimicrobial spectrum was more frequently narrowed in patients with a positive MS (46.7 % of patients with a positive MS vs. 10.8 % with a negative MS, p = 10−7) and in the CAP group (50 % vs. 11.3 %, p = 10−6). There was no significant difference in the other two groups.
Positivity of MS was significantly associated with increased hospital mortality in the CAP group (31.4 % if positive MS vs. 15.5 % if negative, p = 0.04) and with increased one-year mortality in the total population (47.8 % if positive MS vs. 30.4 % if negative, p = 0.03) and the NHAP group (50 % vs. 11.4 %, p = 0.04).
For the three groups, there was no association between MS positivity and the rehospitalisation rate at 6 months or hospitalisation duration; however, the association for the latter was significant in the total population (median hospitalisation length: 27.9 days if positive MS vs. 19 days if negative, p = 0.05) (Table 5).
Discussion
Our main results are as follows: even though the clinical presentation in hospitalised NHAP patients tended to be less severe than that in CAP and HAP patients, with a narrower-spectrum PAT, MS were done with the same frequency despite lower detection rates for resistant pathogens.
NHAP patients were significantly older and had a lower WHO performance status than CAP or HAP patients, as previously reported [13–15]. Interestingly, NHAP patients received a narrower-spectrum PAT [monotherapy for 96.5 % of NHAP, 85.7 % of HAP and 77.9 % of CAP (p = 0.003)] and the clinical presentation tended to be less severe than that in CAP and HAP patients, according to the PSI score, ICU requirement and in-hospital mortality rates. Hospital mortality after NHAP is usually described as lower than after HAP [14] but as greater than after CAP [11, 16]. The less severe clinical presentation and the lower mortality in our study could be explained by an earlier diagnosis and PAT in NHAP than in CAP.
We report a low positivity rate of MS, especially for NHAP, despite the high proportion of samples taken. In a large multi-centre prospective study [16], positivity rates of MS were similar for NHAP and CAP, at up to 27.7 %, but antimicrobial treatment was rarely started before admission (14.5 %), which was not the case in our hospital. One cause of false-negative MS, which contributes to a low detection rate, is, indeed, the prior initiation of PAT [17]. However, delays in the initiation of antibiotic therapy can increase mortality and should not be justified for diagnostic purposes in frail patients [18].
Our microbiological results are consistent with recent studies. NHAP pathogens seem to be closer to those in CAP than in HAP [13, 16, 19]. The most frequent pathogen was Streptococcus pneumoniae. A greater frequency of enterobacteria and Staphylococcus aureus [20, 21] has been reported in NHAP than in CAP. In our study, these pathogens were frequently found in HAP, as reported in the literature [3], but not in NHAP. This could be explained, in part, by the negativation of bacterial cultures caused by the PAT. This bias does not concern HAP, for which MS are usually taken before PAT.
In our study, MS were taken in 91 % of cases. However, the comparison between the PAT and targeted (according to the microbiological results) treatment in adults hospitalised for pneumonia did not reveal any significant outcome-related benefits [22], especially for blood cultures [23], LUA, PUA [24] and bronchoalveolar lavage [25]. In order to improve MS efficiency, we suggest: (1) limiting MS to those that will change the PAT, if positive [4] (e.g. suppressing PUA in patients with beta-lactam PAT), (2) taking MS before introducing PAT [17], or only in patients whose condition is worsening under the PAT, (3) developing more efficient alternative MS (e.g. transthoracic fine-needle aspiration [26]) and molecular biology tools.
MS positivity was significantly associated with increased mortality, probably related to greater initial severity. The reduction of the antibiotic spectrum was the only significant clinical effect of microbiological detection in our study. However, this is debatable because of the imperfect specificity of the microbiological tests and the frequency of co-infections [5, 27].
This study has some limitations. First, the single-centre status makes it difficult to extrapolate the results; however, this choice was made deliberately to ensure the homogeneity of clinical practices, and the implementation and analysis of MS. Second, it was a retrospective study. Third, data concerning the PAT before MS were not collected, despite its impact on MS results.
To conclude, low MS positivity rates and the rare detection of PAT-resistant pathogens do not support systematic microbiological sampling for the in-hospital management of pneumonia in elderly patients, particularly for NHAP. Prospective studies could try to identify predictive factors of resistance to the PAT in order to optimise detection policy and its therapeutic impact.
References
Gruneir A, Bell CM, Bronskill SE, Schull M, Anderson GM, Rochon PA (2010) Frequency and pattern of emergency department visits by long-term care residents—a population-based study. J Am Geriatr Soc 58:510–517
Janssens JP, Krause KH (2004) Pneumonia in the very old. Lancet Infect Dis 4:112–124
American Thoracic Society; Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Mandell LA, Wunderink RG, Anzueto A et al; Infectious Diseases Society of America; American Thoracic Society (2007) Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 44(Suppl 2):S27–S72
Woodhead M, Blasi F, Ewig S et al; Joint Taskforce of the European Respiratory Society and European Society for Clinical Microbiology and Infectious Diseases (2011) Guidelines for the management of adult lower respiratory tract infections—full version. Clin Microbiol Infect 17:E1–E59
American Thoracic Society (1996) Hospital-acquired pneumonia in adults: diagnosis, assessment of severity, initial antimicrobial therapy, and preventive strategies. A consensus statement, American Thoracic Society, November 1995. Am J Respir Crit Care Med 153:1711–1725
Oken MM, Creech RH, Tormey DC et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Fine MJ, Auble TE, Yealy DM et al (1997) A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 336:243–250
Lim WS, van der Eerden MM, Laing R et al (2003) Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 58:377–382
Murray PR, Baron EJ, Pfaller MA, Tenover FC, Yolken RH (1995) Manual of clinical microbiology, 6th edn. ASM Press, Washington, DC
Lim WS, Macfarlane JT (2001) A prospective comparison of nursing home acquired pneumonia with community acquired pneumonia. Eur Respir J 18:362–368
Maruyama T, Niederman MS, Kobayashi T et al (2008) A prospective comparison of nursing home-acquired pneumonia with hospital-acquired pneumonia in non-intubated elderly. Respir Med 102:1287–1295
Ugajin M, Yamaki K, Hirasawa N, Kobayashi T, Yagi T (2014) Prognostic value of severity indicators of nursing-home-acquired pneumonia versus community-acquired pneumonia in elderly patients. Clin Interv Aging 9:267–274
Ewig S, Klapdor B, Pletz MW et al; CAPNETZ study group (2012) Nursing-home-acquired pneumonia in Germany: an 8-year prospective multicentre study. Thorax 67:132–138
Simonetti AF, Viasus D, Garcia-Vidal C et al (2014) Impact of pre-hospital antibiotic use on community-acquired pneumonia. Clin Microbiol Infect 20:O531–O537
Kollef MH, Sherman G, Ward S, Fraser VJ (1999) Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest 115:462–474
Polverino E, Dambrava P, Cillóniz C et al (2010) Nursing home-acquired pneumonia: a 10 year single-centre experience. Thorax 65:354–359
Garb JL, Brown RB, Garb JR, Tuthill RW (1978) Differences in etiology of pneumonias in nursing home and community patients. JAMA 240:2169–2172
Marrie TJ, Blanchard W (1997) A comparison of nursing home-acquired pneumonia patients with patients with community-acquired pneumonia and nursing home patients without pneumonia. J Am Geriatr Soc 45:50–55
van der Eerden MM, Vlaspolder F, de Graaff CS et al (2005) Comparison between pathogen directed antibiotic treatment and empirical broad spectrum antibiotic treatment in patients with community acquired pneumonia: a prospective randomised study. Thorax 60:672–678
Corbo J, Friedman B, Bijur P, Gallagher EJ (2004) Limited usefulness of initial blood cultures in community acquired pneumonia. Emerg Med J 21:446–448
Falguera M, Ruiz-González A, Schoenenberger JA et al (2010) Prospective, randomised study to compare empirical treatment versus targeted treatment on the basis of the urine antigen results in hospitalised patients with community-acquired pneumonia. Thorax 65:101–106
Rodriguez RM, Fancher ML, Phelps M et al (2001) An emergency department-based randomized trial of nonbronchoscopic bronchoalveolar lavage for early pathogen identification in severe community-acquired pneumonia. Ann Emerg Med 38:357–363
Hernes SS, Hagen E, Tofteland S et al (2010) Transthoracic fine-needle aspiration in the aetiological diagnosis of community-acquired pneumonia. Clin Microbiol Infect 16:909–911
Fernández-Sabé N, Carratalà J, Rosón B et al (2003) Community-acquired pneumonia in very elderly patients: causative organisms, clinical characteristics, and outcomes. Medicine (Baltimore) 82:159–169
Acknowledgements
The authors are grateful to Mr. Philip Bastable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Putot, A., Tetu, J., Perrin, S. et al. Impact of microbiological samples in the hospital management of community-acquired, nursing home-acquired and hospital-acquired pneumonia in older patients. Eur J Clin Microbiol Infect Dis 35, 489–495 (2016). https://doi.org/10.1007/s10096-015-2565-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2565-9