Abstract
Antibiotics have been overused and misused for preventive and therapeutic purposes. Specifically, antibiotics are frequently used as growth promoters for improving productivity and performance of food-producing animals such as pigs, cattle, and poultry. The increasing use of antibiotics has been of great concern worldwide due to the emergence of antibiotic resistant bacteria. Food-producing animals are considered reservoirs for antibiotic resistance genes (ARGs) and residual antibiotics that transfer from the farm through the table. The accumulation of residual antibiotics can lead to additional antibiotic resistance in bacteria. Therefore, this review evaluates the risk of carriage and spread of antibiotic resistance through food chain and the potential impact of antibiotic use in food-producing animals on food safety. This review also includes in-depth discussion of promising antibiotic alternatives such as vaccines, immune modulators, phytochemicals, antimicrobial peptides, probiotics, and bacteriophages.
Similar content being viewed by others
Introduction
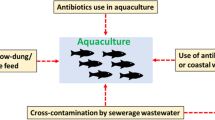
Antibiotics, the secondary metabolites produced by microorganisms such as bacteria, fungi, and plants, have been used to kill or inhibit foodborne pathogens. Antibiotics are structurally divided into several classes, including β-lactams, quinolones, fluoroquinolones, macrolides, aminoglycosides, and tetracyclines (Coates et al., 2011). Ever since the discovery of penicillin, the use of antibiotics has been extended from the treatment of infectious diseases caused by pathogens to the growth promoter in animal husbandry, agriculture, fishery, and aquaculture industries (Roca et al., 2015). Over the past few decades, the global meat production has increased with increasing the demand for meat, which can correspond to the increase in antibiotic use. The global antibiotic consumption can be increased up to 110,000 tons by 2030 (Van Boeckel et al., 2015). Antibiotics used in veterinary medicines are about twice as high as those used in humans. In specific, animal husbandry including pigs, cattle, and poultry accounts for the majority of agriculture.
The appropriate use of antibiotics is essential to effectively treat infectious diseases and promote animal growth. However, the residual antibiotics in foods and environments have been increased due to the overuse and misuse of antibiotics, leading to the rapid spread and emergence of antibiotic-resistant bacteria (Ben et al., 2019). A study reported that 700,000 people die from antibiotic-resistant bacterial infections each year, which can be increased to 10 million by 2050 (O'Neill, 2016). The emergence of antibiotic-resistant bacteria, especially multidrug resistance, has become a serious problem in the fields of medical care, animal husbandry, food industry, and public health (Monger et al., 2021). Moreover, the antibiotic prevention and treatment for infectious diseases are limited because the discovery and development of new antibiotics are lagged behind the spread of multidrug resistant bacteria. The new antibiotics require significant investment in research and development. Therefore, understanding the impact of antibiotic use and residues in food animals is essential to prevent misuse and overuse of antibiotics. This review discusses the influence of antibiotic resistance and residual antibiotics on food safety from farm to table.
Mechanisms of bacterial resistance to antibiotics
The antibiotic resistance in bacteria occurs through self-protection mechanism which is evolved under natural conditions to acquire resistance against harmful environments. Antibiotics can be commonly classified according to the inhibitory mechanisms, including inhibition of cell wall synthesis, disruption of the cytoplasmic membrane, inhibition of protein synthesis, inhibition of nucleic acid synthesis, and induction of alternative metabolic pathway (Culp et al., 2020; Kapoor et al., 2017) (Fig. 1). Gram-positive bacteria are sensitive to macrolides, cephalosporins, β-lactamase inhibitors, penicillins, and lincosamides, which are mostly bactericidals that inhibit the cell wall synthesis. Gram-negative bacteria are sensitive to aminoglycosides, polymyxins, and quinolones, which are mainly bactericidal through the inhibition of protein synthesis. Bacteria can develop antibiotic resistance mechanisms including antibiotic efflux pump systems, alteration in drug target sites, disruption of membrane permeability, and development of metabolic bypass (Kapoor et al., 2017; Lin et al., 2015).
Schematic illustration of antibiotic resistance mechanisms in bacteria, including A alteration of membrane permeability (mutated lipoteichoic acid [LTA], mutated porin channel, and lipocalin), B modification of antibiotic target sites (mutated penicillin-binding proteins [PBPs] and modified peptidoglycan), C enzymatic degradation of antibiotics (β-lactamases and transferase), D activation of bacterial efflux pump systems (major facilitator superfamily [MFS], small multidrug resistance [SMR], multidrug and toxic compound extrusion [MATE], ATP binding cassette [ABC], and resistance nodulation division [RND]), and E bypass of metabolic pathway inhibited by antibiotics (alternative folic acid synthesis)
Alteration of membrane permeability
The limiting uptake of a drug is responsible for bacterial resistance to antibiotics by reducing the envelope permeability, known as intrinsic resistance. Gram-negative bacteria have the outer membrane that acts as a robust barrier against antimicrobial agents. The outer membrane, a unique asymmetric lipid bilayer, consists of phospholipids and polysaccharides (Reygaert, 2018). The hydrophobicity of the outer membrane is attributed to the lipopolysaccharide (LPS) or lipooligosaccharide (LOS), showing strong lateral interactions with divalent cations. The outer membrane can prevent the access antibiotics and bile salts into the cell (Delcour, 2009). Gram-negative bacteria contain β-barrel proteins, called porin channels, in the outer membrane that is permeable to hydrophilic molecules such as ampicillin and amoxicillin (Danelon et al., 2006; Delcour, 2009; Nestorovich et al., 2002). The porin channels are less developed in the outer membrane of antibiotic-resistant bacteria (Delcour, 2009; Khameneh et al., 2016). For example, 44% of β-lactam-resistant Enterobacter aerogenes isolated from French hospitals were deficient in the porin channels, and other Enterobacteriaceae also showed a low number of porin channels, leading to carbapenem resistance (Charrel et al., 1996; Cornaglia et al., 1996). The porin-deficient Klebsiella pneumoniae exhibited the enhanced resistance to β-lactams and fluoroquinolones (Khalid et al., 2020). The lipocalins, BcnA, in the outer membrane of Burkholderia cenocepacia can capture antibiotics, resulting in antibiotic resistance (El-Halfawy et al., 2017). In addition, BcnA induces the resistance of Pseudomonas aeruginosa PAO1 to polymyxin B (El-Halfawy et al., 2017). Th hydrophobic block of lipid layer covalently linked to arabinogalactan-peptidoglycan polymer in Mycobacteria contributed toward the development of resistance to hydrophilic antibiotics (Nasiri et al., 2017). Unlike Gram-negative bacteria, Gram-positive bacteria lack an outer membrane and have the cell wall consisting of a thick peptidoglycan layer that facilitates the penetration of hydrophobic antimicrobials (Karaman et al., 2020). However, anionic lipoteichoic acid (LTA) embedded in peptidoglycan can restrict the penetration of positively charged antibiotics, leading to antibiotic resistance (Abachin et al., 2002; Malanovic and Lohner, 2016; Peschel et al., 1999).
Modification of antibiotic target sites
The modification of target sites for antibiotics is a self-resistance mechanism under selection pressure of antibiotics (Reygaert, 2018). The β-lactam antibiotics is structurally similar to the penicillin-binding proteins (PBPs) that play an important role in the biosynthesis of peptidoglycan (Sauvage et al., 2008). The structural analogs, penicillin and cephalosporin, irreversibly acylate an active site of PBPs, leading to the inhibition of bacterial growth (Zapun et al., 2008). In this context, Streptomyces species and Streptococcus pneumoniae are highly resistant to penicillin by overproducing low-affinity PBPs for β-lactams (Beceiro et al., 2013; Blair et al., 2015; Watts et al., 2017). Glycopeptides such as vancomycin and teicoplanin bind to peptidoglycan precursors (D-Ala-D-Ala) and inhibit cell wall transpeptidation and transglycosylation (Kang and Park, 2015). The alteration in peptidoglycan precursor from D-Ala-D-Ala to D-Ala-D-Lac or D-Ala-D-Ser cause results in a significant decrease in affinity for the glycopeptide (Peterson and Kaur, 2018). The resistance to antibiotics targeting bacterial ribosome can be induced by the methylation of ribosomal subunits, known as erythromycin ribosome methylase (erm) (Reygaert, 2018). For example, the resistance to macrolide, lincosamide, and streptogramin B (MLSB) were due to the methylation of ribosomal subunits (Lioy et al., 2014; Reygaert, 2018; Roberts, 2004). The resistance to quinolone and fluoroquinolones targeting DNA gyrase and topoisomerase IV is caused by the structural changes in DNA gyrase and topoisomerase IV, (GryA or ParC), responsible for the reduced binding ability to the DNA gyrase-DNA complex (Hawkey, 2003; Hooper and Jacoby, 2016; Redgrave et al., 2014).
Enzymatic degradation of antibiotics
The hydrolase-type enzymes can cleave substrates such as β-lactams, aminoglycosides, phenicols, and macrolides, leading to antibiotic resistance in bacteria (Blair et al., 2015; Reygaert, 2018). In general, β-lactamases can hydrolyze β-lactam antibiotics such as penicillins, cephalosporins, clavams, carbapenems, and monobactams. Moreover, extended-spectrum β-lactamases (ESBLs) can confer resistance to most β-lactam antibiotics, including oxyimino-cephalosporins (Livermore, 2008). Recently, the emergence and spread of carbapenemase-producing bacteria, including Klebsiella pneumoniae and Enterobacteriaceae, have been a global health challenge due to high morbidity and mortality (Pitout et al., 2015; Reygaert, 2018). The steric hindrance of the target sites for antibiotics can lead to antibiotic resistance (Blair et al., 2015). The antibiotic-modifying enzymes such as transferases can confer antibiotic resistance by transferring functional groups (acly, phosphate, nucleotidyl and ribitoyl) to aminoglycosides, chloramphenicol, streptogramins, and fluoroquinolones (Blair et al., 2015; Ramirez and Tolmasky, 2010; Reygaert, 2018; Robicsek et al., 2006). In addition, the rifamycin phosphotransferases are directly associated with the rifamycin resistance in pathogens (Spanogiannopoulos et al., 2014).
Activation of bacterial efflux pump system
Bacterial efflux transporters are classified into five superfamilies, including ATP-binding cassette (ABC) superfamily, major facilitator superfamily (MFS), drug and metabolite transporter (DMT) superfamily containing small multidrug resistance (SMR) family, multidrug and oligosaccharidyl-lipid/polysaccharide (MOP) exporter superfamily (multidrug and toxic compound extrusion (MATE) family), and resistance-nodulation-cell division (RND) superfamily (Begić and Josić, 2020). These superfamilies are involved in the outer membrane permeability which can render antibiotic ineffective against bacteria. The efflux pump-associated genes are overexpressed in the presence of antibiotics, which confers multidrug resistance (Reygaert, 2018; Van Bambeke et al., 2000).
The ABC transport systems form one of the largest protein families, found in all living organisms (Rees et al., 2009). The ABC transport systems are essential for bacterial survival, involved in the uptake of essential nutrients and the efflux of toxic molecules (Davidson et al., 2008; Szakács et al., 2008). The common ABC transport systems share a conserved core of four domains including two transmembrane domains (TMD) and two nucleotide-binding domains (NBD) (Lewis et al., 2012). The ABC transport systems are able to export antibiotics, for instance, VcaM can transport fluoroquinolones and tetracyclines in Vibrio cholera (De, 2021). The ABC transport systems include DrrAB that secretes daunorubicin and doxorubicin in Streptomyces peucetius and OleC4-OleC5 oleandomycin transporter in Streptomyces antibiotics (Lewis et al., 2012).
The MFS consists of uniporters, symporters, and antiporters, referred to the uniporter-symporter-antiporter (USA) family (Kumar et al., 2013) and are involved in the transport of anions, antibiotics, metabolites, and sugars (Reygaert, 2018). To export specific substrates, the MFS-type efflux pumps generate energy using an ion concentration gradient across the membrane (Kumar et al., 2020). The MFS-type efflux pumps can specifically export erythromycin (SmvA) and chloramphenicol (CraA and CmlA) in Acinetobacter baumannii and macrolides (MefB), fluoroquinolones (QepA) and trimethoprim (Fsr) in Escherichia coli (Kumar et al., 2020; Reygaert, 2018). The SMR-type efflux pumps are small integral inner membrane proteins that use the proton-motive force (Bay et al., 2008). The hydrophobic property of SMR-type efflux pumps contributes to a narrow range of substrates (Bay et al., 2008; Reygaert, 2018). Few SMR families are involved in antibiotic resistance, including Sau-Smr in Staphylococcus epidermidis and Eco-EmrE in E. coli (Bay et al., 2008; Nishino and Yamaguchi, 2001). The SMR-type efflux pumps confer the resistance to β-lactam, some aminoglycosides, and glycopeptides (Bay et al., 2008). In addition, the SMR-associated genes are found in chromosomes, plasmids, and transposable elements (Kumar and Schweizer, 2005; Reygaert, 2018).
The MATE-type efflux pumps are classified into three subfamilies, including NorM, DinF, and eukaryotic MATE (eMATE) (Kusakizako et al., 2020; Reygaert, 2018). Bacterial MATE, NorM and DinF, are composed of 12 membrane helices (Kusakizako et al., 2020). The bacterial MATE-type efflux pumps in bacteria have been found in Vibrio cholerae, V. parahaemolyticus, Neisseria gonorrhoeae, and N. meningitidis (Kuroda and Tsuchiya, 2009). The substrates of the MATE-type multidrug efflux pumps include fluoroquinolones and aminoglycosides.The RND-type efflux pumps are mostly found extensively in Gram-negative bacteria and have a broad substrate specificity conferring resistance to multiple antibiotics (Khameneh et al., 2016; Kumar et al., 2020; Reygaert, 2018). The major RND-type efflux pumps include proton-driven tripartite systems across the inner membrane, the periplasm, and the outer membrane of Gram-negative bacteria (Li et al., 2015). The AcrAB-TolC system consists of AcrB in the inner membrane, AcrA in the periplasm, and TolC in the outer membrane in E. coli, conferring the resistance to penicillin, chloramphenicol, macrolides, fluoroquinolones, and tetracycline (Kourtesi et al., 2013). The MexAB-OprM system confers the resistance of Pseudomonas aeruginosa to β-lactam, chloramphenicol, tetracycline, trimethoprim, sulfamethoxazole, and fluoroquinolones (Kumar et al., 2013; Li et al., 2015; Reygaert, 2018).
Change in metabolic pathway
Bacteria can also resist to antibiotics by modifying the metabolic pathway or developing alternate metabolic pathways (Saha and Sarkar, 2021). For example, there are several mechanisms that can produce an additional DNA gyrase subunit for novobiocin resistance, an alternative resistant RNA polymerase for rifamycin resistance, and an alternative fatty acid synthase for platensimycin resistance (Fujimoto-Nakamura et al., 2005; Goldstein, 2014; Peterson et al., 2014). The srrAB is a two-component system that is involved in the overall transcriptional regulation of virulence factors in small colony variants (SCVs) of Staphylococcus aureus and survival in anaerobic environments (Cao et al., 2017). The srrAB mutation of SCVs introduces an alternative transcriptional pathway against kanamycin and increasing ATP production in an anaerobic environment, thereby enhancing both resistance to kanamycin and viability (Cao et al., 2017; Saha and Sarkar, 2021). In addition, an antibiotic resistant mechanism can furthers activate metabolic pathways targeted by antibiotics (Munita and Arias, 2016). The trimethoprim-sulfamethoxazole (TMP-SMX) inhibits dihydropteroic acid synthase (DHPS) and dihydrofolate reductase (DHFR) in the folate pathway (Munita and Arias, 2016). The TMP-SMX-resistant bacteria mutate the promoters of the genes encoding DHPS and DHFR to overproduce two enzymes that enhance the antimicrobial activity of TMP-SMX, and also acquires pathways that uses external folates (Eliopoulos and Huovinen, 2001; Flensburg and Skold, 1987).
Acquisition and spreading of antibiotic resistance in food animals
Antibiotics have commonly been used to control the infectious diseases and promote animal growth in husbandry and veterinary care. However, the spread of antibiotic-resistant pathogens has accelerated due to the misidentification of antibiotic-treated animals and misunderstanding of antibiotic use (Oliveira et al., 2020).
Antibiotic used in pig
Pigs are one of the most important farm animals in terms of both numbers and biomass (Delsart et al., 2020). The largest pork producers include China and the United States, followed by Germany, Spain, and Vietnam (Núñez-Espinoza et al., 2022). These countries represent nearly 65% of global production (Zalewska et al., 2021). Pig husbandry is expected to continue increase up to 8.6% by 2030 and 12.7% by 2050 (Monger et al., 2021). In recent years the use of antibiotics has been restricted worldwide, but antibiotics are commonly used during the suckling period and post-weaning period (Lekagul et al., 2019). The antibiotics used in pig husbandry include amoxicillin, fluoroquinolones, penicillin, tetracyclines, cephalosporins, lincosamides, tulathromycin, polymyxin (colistin) and macrolid (tylosin) (Coyne et al., 2019; Lekagul et al., 2019). Among these antibiotics, the most commonly used antibiotics are relatively inexpensive and cost-effective antibiotics such as penicillin and the tetracycline (Coyne et al., 2019). The bacterial infections in pig are caused by Salmonella spp., Escherichia coli, Actinobacillus pleuropneumoniae, Actinobacillus suis, Pasteurella multocida, Mycoplasma hyopneumoniae, and Streptococcus suis. The increase in sepsis caused by S. suis resistant to penicillin, tetracycline, and macrolide significantly affects pig production (Monger et al., 2021). The use of performance-enhancing antibiotics such as chlortetracycline, sulfamethazine, and penicillin can change gut microbiota that include various antibiotic resistance genes (ARGs) (Looft et al., 2012; Zalewska et al., 2021). The most widespread ARGs in the pig husbandry are tetracycline resistance genes, showing 71% of tetracycline resistance in Enterococcus spp. (Haack and Andrews, 2000). The tetracycline resistance genes were widespread in pig feces, farm soil, and wastewater (Kang et al., 2018). More than 400 of ARGs were identified in 181 pig herds and 178 poultry farms in European countries and 146 ARGs were identified in 7 Chinese pig farms (Munk et al., 2018; Zhao et al., 2018). In addition, the residual antibiotics can carry over from pig to pork (Monger et al., 2021). The use of antibiotics in animal farms can lead to the deposition of residues in meat that can spread from animals to humans (Chen et al., 2019) (Fig. 2).
Antibiotics used in cattle
The largest beef producers include Brazil, Canada, the USA, Argentina, the EU and Australia. The beef and dairy industries use a variety of antibiotics, including aminoglycosides, β-lactams, chloramphenicol, fluoroquinolones, glycolipid, ionophores, macrolides, quinolones, streptogramins, sulfonamides, and tetracyclines (Zalewska et al., 2021). Chlortetracycline, tylosin, ceftiofur and sulfamethoxazole have commonly been used for cattle in North America (Aust et al., 2008). In Europe, macrolides and lincosamides are commonly used for the treatment of various infectious diseases in cattle. In particular, tetracyclines are widely used to treat respiratory, gastrointestinal, and skin disease in cattle (Zalewska et al., 2021). Major infectious diseases in cattle are caused by Pasteurella multocida, Mannheimia haemolytica, Escherichia coli, Salmonella spp., Staphylococcus aureus, and Streptococcus spp. (Andres-Lasheras et al., 2022; Awosile et al., 2018). With increasing the consumption of beef, the use of antibiotics has been increased in cattle, causing serious antibiotic resistance problem. In addition, cattle manure used as soil fertilizer significantly contributes the dissemination of antibiotic-resistant bacteria and ARGs (Chen et al., 2019; Sachi et al., 2019). The microbial community in the cattle treated with antibiotics contains various transferable genes conferring resistance to MLSB, tetracyclines, and sulfonamides (Alexander et al., 2011; Chen et al., 2008). The excessive use of ceftiofur in cattle plays an important role in the spread of ARGs and multidrug-resistant bacteria (Chambers et al., 2015). The potential transmission of ARGs from cattle to beef and human can be a serious problem (Zalewska et al., 2021).
Antibiotics used in poultry
The poultry consumption is high in the Asia–Pacific region, and the global poultry market has been increased. The largest poultry producers in 2019 was the USA (19,710,000 tons), followed by Brazil, the EU, and China (Zalewska et al., 2021). Recently, the use of antibiotics in meat and poultry products has been restricted in the USA and EU. However, the use of antibiotics is essential for disease prevention and growth promotion in poultry. The most commonly used antibiotics in poultry are virginiamycin, bacitracin, salinomycin, and tilmicosin (Zalewska et al., 2021). These antibiotics have been used to treat infectious poultry diseases caused by avian pathogenic E. coli (APEC), Salmonella Pullorum, S. Gallinarum, Pasteurella multocida, Avibacterium paragallinarum, Gallibacterium anatis, Ornitobacterium rhinotracheale, Bordetella avium, Clostridium perfringens, Mycoplasma spp., Erysipelothrix rhusiopathiae, and Riemerella anatipestifer (Porter, 1998). The frequent use of antibiotics for disease prevention and growth promotion has inevitably caused the emergence of antibiotic-resistant bacteria (Fletcher, 2015). In particular, APEC has developed resistance to ampicillin, amoxicillin, and tetracycline (Nhung et al., 2017). In addition, O. rhinotracheale showed significantly high levels of phenotypic resistance to co-trimoxazole, enrofloxacin, gentamicin, amoxixillin, and ceftiofur (Nhung et al., 2017). The antibiotics used in food animals were tetracyclines in 71% of the United States and 37% of Europe, which remain in meat (Gonzalez Ronquillo and Angeles Hernandez, 2017). The residual antibiotics are contaminated in the laying eggs of poultry, posing a risk to human (Idowu et al., 2010). Furthermore, poultry had the high prevalence of ciprofloxacin-resistant bacteria. Genes resistant to chloramphenicol, quinolones, tetracyclines, and sulfonamides have been detected in poultry (Amador et al., 2019; Zalewska et al., 2021).
Prevalence and transmission of antibiotic resistance from farm to fork
The Center for Disease Control and Prevention (CDC) estimates that 48 million people suffer from foodborne illness each year. Common foodborne pathogens including Campylobacter spp., Bacillus cereus, pathogenic Escherichia coli, Salmonella spp., Staphylococcus spp., Enterococcus spp., and ESBL-producing Gram-negative bacteria can cause diarrhea, fever, vomiting and other symptoms, and even severe cases can be life-threatening or fatal (Economou and Gousia, 2015). Foodborne pathogens that acquire antibiotic resistance through horizontal or vertical gene transfer cause difficult-to-treat infectious diseases (Table 1). Thus, understanding the antibiotic resistance transmission is essential for reducing the occurrence of antibiotic resistance from the animal food sources.
Macro-level determinants of antibiotic resistance transmission
The antibiotic-resistant foodborne pathogens continue to multiply and transfer antibiotic resistance to offspring, and eventually become the main flora (Founou et al., 2016). This phenomenon occurs not only in humans and animals, but also in the natural environment. Food animals, crops, and aquatic products are considered to be a large pool of antibiotic-resistant bacteria because the food production chain is recognized as the major reservoirs of ARGs (Founou et al., 2016). Human-animal-environment is a whole of mutual influence and interaction, and antibiotic resistance can be spread through direct or indirect contact between humans and animals (Fig. 2). For example, methicillin-resistant Staphylococcus aureus (MRSA) is quickly disseminated from infected animals to farmers worldwide (Aarestrup, 2015; Lewis et al., 2008; Price et al., 2012). Furthermore, the bovine S. aureus CC97 strain was transferred from livestock to humans. The epidemic community-associated MRSA (CA-MRSA) was also spread after host adaptation (Aires-de-Sousa, 2017). Since 1997, the occurrence of vancomycin-resistant Enterococcus faecium (VREF) has been decreased because vancomycin analogue (Avoparcin) was banned in Europe (Gouliouris et al., 2018). In case of Salmonella strains, fluoroquinolone and cephalosporin resistance cause the biggest global health problem, and these strains pose a major threat to human through feeding animal foods (Aslam et al., 2021; Dutil et al., 2010; Helms et al., 2004). Besides, multidrug-resistant E. coli, which can be a source of infection for humans and animals due to contaminated drinking water and food, is a leading cause of public health problems in developing countries (Aslam et al., 2021; Lazarus et al., 2015). Although foodborne pathogens are controlled by physical and chemical interventions, their ARGs are still transferable and infectious (Table 1).
The consumption of food animals that are contaminated with pathogens or ARGs can cause imbalance of the intestinal flora, leading to allergic hypersensitivity, toxic effects, liver toxicity, nephropathy, mutagenesis, carcinogenesis, and antibiotic resistance (Aslam et al., 2021; Malik et al., 2019). Human excrement carrying ARGs may also be passed to animals and environments. The antibiotic resistant bacteria and genes contaminate soil and groundwater or other water resources through feces and water cycle, and then cross-contaminate crops and aquatic products, and eventually reach the table and infect humans (Thanner et al., 2016). However, it is practically difficult to manage the risks of wastewater treatment plants, drinking water, and coastal waters that can be the reservoir of the ARGs (Leonard et al., 2018; Ma et al., 2017). Animal-eating grass containing ARGs or contaminated drinking water can also increase the risk of resistance. In addition, the physical and chemical stresses in food processing, such as acids, oxidants, osmosis, heating, freezing, can also cause resistance to foodborne pathogens (Liao et al., 2020). Therefore, during food processing and transportation, the contamination caused by antibiotic-resistant pathogens needs to be reduced for making sure that safe and reliable foods come to the table. Antibiotics are used for the treatment of infectious diseases and growth promoter for directly humans and animals (Fig. 2). Residual antibiotics are present in water, soil, and animal foods, which can further contaminate various food products. Bacteria exposed to the residual antibiotics can be mutated and directly or indirectly infect humans through ARGs and/or antibiotic-contaminated food products.
Micro-level determinants of antibiotic resistance transmission
ARGs are prevalent in humans, animals, and environments through the farm to the fork at the macro-level and also widespread through genetic elements at the micro-level. There are two main biological pathways, including vertical transmission and horizontal transmission. First, when pathogenic bacteria are mutated under the selective pressure of antibiotics and acquire ARGs that can be passed onto progeny during proliferation, resulting in innate resistance in offspring. The other pathway is to acquire antibiotic resistance through horizontal gene transfer (HGT) so that mobile genetic elements transfer through transformation, transduction, and conjugation within and between bacterial species (Founou et al., 2016). The gene transfer from donor to recipient bacteria through cell-to-cell contact is the main transmission, termed as bacterial conjugation (Leclerc et al., 2019). After contact, the bacterial cells transfer plasmid DNA through a conjugative pilus (Kelly et al., 2009). Bacteria can also actively secrete DNA through membrane vesicles. In natural environment, many bacteria can spontaneously become competent and absorb foreign DNA, which is called transformation. DNAs are prevented from being degraded and integrated into the host genome. This technique has commonly been used in the laboratories for genetic transformation. Mobile genetic elements such as plasmids, integrons, transposons, and phage-mediated gene transfer, are involved in the resistance gene transfer (Hughes and Andersson, 2017).
Plasmids play a pivotal role in the transmission of ARGs from bacteria to bacteria (Vrancianu et al., 2020). Vancomycin-resistant Enterococcus (VRE) contains vancomycin resistance genes encoded in mobile genetic elements (Miller et al., 2014; Ray et al., 2003). The broad-host range plasmid, pAMβ1, can transfer from Lactococcus lactis donor strains to Enterococcus spp. present in the microbiota of human biota-associated (HBA) rats (Tuohy et al., 2002). The transposons can cause the antibiotic resistance transfer from one plasmid to the other, or DNA chromosome to plasmid (Babakhani and Oloomi, 2018). Tetracycline resistance determinants, tet(M) and tet(L), are located in the genome of Lactobacillus ingluviei DSM 15946 T, and upstream of tet(M) are conjugation transfer elements. Integrons are important genetic elements encoding ARGs, acting as a vehicle for disseminating multidrug resistance (Arango-Argoty et al., 2019). The integrons are classified into two major groups; chromosomal integrons (CIs) and mobile integrons (MIs). The MIs are a broad genetic platform that allows bacteria to regulate the expression of antibiotic resistance cassettes by shuffling positions in a common promoter (Souque et al., 2021; Stalder et al., 2012). Class 1 integrons are detected in a significant fraction of isolates of Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter baumannii (Souque et al., 2021). The phage-mediated gene transfer, known as transduction, occurs in nature due to abundant bacteriophages that are highly specific for hosts. The genes encoding shiga toxins, stx1 and stx2, are transferable to E. coli by bacteriophage-mediated transduction (Wick et al., 2005). Salmonella Typhimurium DT104 containing cam, amp, and tet genes conferring chloramphenicol, ampicillin and tetracycline resistance, respectively, was transduced by phage PDT17 and phage ES18 (Colavecchio et al., 2017). ES18 could co-transduce sul and str, conferring sulfonamide and streptomycin resistance, respectively (Schmieger and Schicklmaier, 1999).
Treatment and preventive strategies to combat antibiotic resistance
Antibiotics have been utilized by treating disease, controlling infection, or promoting productivity and growth of livestock, enhancing feed efficiency. In reality, it is known that 40% of all antibiotics currently produced are used as feed additives. According to estimates, the global average annual consumption of antibiotics per kilogram of food animals is to be 45, 148, and 172 mg/kg for cattle, chicken, and pigs, respectively (Van Boeckel et al., 2015). However, since the wide spreading of antibiotic-resistant bacteria and ARGs caused by the increase in the use of antibiotics in food-producing animals, the discovery and development of antibiotic alternatives are essential to improve food safety. Antibiotic alternatives suggested or used in food animals are bacteriophages, antimicrobial peptides, probiotics, vaccines, immune modulators, and phytochemicals (Table 2).
Vaccines
Vaccines for food-producing animals are currently used to effectively control bacterial infections as antibiotic alternatives. The use of vaccines on pig farms provides cost-effectiveness, antibiotic consumption reduction, and production improvement (Postma et al., 2017; Rojo-Gimeno et al., 2016). For example, vaccination prevented pig from Laesonia intracellularis infection causing ileitis and also reduced the consumption of oxytetracyline in the treatment of ileitis (Bak and Rathkjen, 2009). In poultry, vaccination also confers more advantages than other treatments such as antibiotics. As a result, the antibiotic consumption was significantly reduced by the increased use of vaccination against avian colibacillosis (Dalloul and Lillehoj, 2006; Mombarg et al., 2014). In cattle industry, the vaccination is used for the prevention of respiratory infections caused by bacteria and viruses (Richeson et al., 2015, 2019). However, veterinary vaccinations have limitations on efficacy, duration of immunity, and side effect. For instance, vaccine was not effective against Mycoplasma mycoides that causes contagious bovine pleuropneumonia with varied duration of protective immunity and serious adverse effects in cattle (Jores et al., 2013). Salmonella vaccines are most effective against homologous Salmonella but least effective against heterologous serotypes (Barrow, 2007; Hoelzer et al., 2018). Moreover, since vaccine efficacy is associated with active immunity, young animals may not properly respond to vaccines (Hoelzer et al., 2018). In addition, vaccine is not effective against pathogens that can avoid the host are resistant to host immune. Nevertheless, the vaccination is still one promising method to reduce the antibiotic use for food-producing animals.
Immune modulators
Immune modulators such as cytokines, pharmaceuticals, microbial products, nutraceuticals, and traditional medicinal plants play an important role in the prevention of diseases and improvement of production efficiency (Blecha, 2001). These immune modulators are more effective against a wide range of pathogens than vaccines due to the stimulation of animal immune system (Koo et al., 2006). The egg-yolk antibodies (IgY) effectively prevented the diarrhea in food-producing animals and reduced necrotic enteritis in poultry (Diraviyam et al., 2014). Although the IgY in swine gut is not stable and has a narrow host spectrum, the antibodies can be used as alternative over antibiotics because of the potential ability to prevent and treat diarrhea in piglets (Diraviyam et al., 2014). In addition, the immunity of swine fed a fodder containing vitamin C and β-glucan was improved and showed effective resistance against bacterial toxins (Eicher et al., 2006). Specific drugs such as avridine, diethyldithiocarbamate, and Isoprinosine have also been used as immune modulators. Interestingly, drugs such as thiabendazole and levamisole are used as immune modulators because they enhance the immune system of food animals with positive side effects (Blecha, 2001). However, immune modulators are highly dependent on the immune system of food animals and are greatly affected by the acquired environment in which food animals are grown (Cheng et al., 2014). For example, immune modulators are ineffective against young animals, whose immune systems are not fully developed, and in animals under extreme environmental stress, and can negatively affect normal immune development (Bricknell and Dalmo, 2005; Cheng et al., 2014). The immune modulators used as adjuvants can effectively reduce the use of antibiotics (Cheng et al., 2014).
Phytochemicals
Phytochemicals such as essential oils and tannins are natural bioactive compounds that are added to animal feed for improving the productivity of food animals (Lillehoj et al., 2018). Recently, phytochemicals have been commonly used as natural growth promoters in the poultry and ruminant industry (Gadde et al., 2017; Lillehoj et al., 2018). In particular, the phytochemicals are used in commercial poultry operations for growth promotion and disease prevention. European Medicines Authority (EMA) and European Food Safety Authority (EFSA) suggested that phytochemicals are effective in promoting growth in chickens. For example, cinnamaldehyde ((2E)-3-phenylprop-2-enal) extracted from cinnamon (Cinnamomum cassia) increased the chicken immunity by proliferating chicken spleen lymphocytes (Lee et al., 2011). In addition, Curcuma longa (turmeric), Capsicum annuum and C. frutescens (hot pepper), and Lentinus edodes (shiitake mushroom) induced weight gain, reduced fecal oocyst shedding in E. acervuline–infected birds, and increased serum antibody titers against profilin (Lee et al., 2009). Capsicum oleoresin, garlic botanical, or turmeric oleoresin fed to E. coli-infected pigs improved the intestinal health of the pigs and reduced the adverse effects of E. coli. Moreover, phytochemicals relieved the stimulation of immune response and enhanced the physiological defense mechanism in pig (Liu et al., 2014). Capsicum oleoresin in beef cattle feeding improved milk production and immune indicators with increasing neutrophils and decreasing lymphocytes (Oh et al., 2015). However, the use of phytochemicals as alternatives still has a safety concern when used in animal feeding (Lillehoj et al., 2018).
Antimicrobial peptides
Antimicrobial peptides (AMPs) are known as promising antibiotic alternatives because of their strong specificity and high molecular stability. AMPs are mainly classified based on the structural composition and amino acid sequence, including defensins, cathelicidins, hepcidins, histone-derived peptides, and fish specific piscidins (Fasina et al., 2021). Proline-Arginine-39 (PR-39) is a small cationic cathelicidin that has antibacterial activity against Enterococcus faecalis, E. coli, and Bacillus subtilis and relieve intestinal inflammation and diarrhea in pigs (Holani et al., 2016). β-defensin plays an essential role in innate and adaptive immunity of vertebrates and has inhibitory effects against pathogenic bacteria, fungi, mycobacteria, and enveloped viruses (Auvynet and Rosenstein, 2009; Jiao et al., 2017). Pigs fed with fodder supplemented with a specific amino acid and cation mixtures showed the increase in expression of β-defensin genes. These results indicate that AMPs helped improve gut health in pig (Mao et al., 2012). Cecropins are peptides produced in the small intestine of pigs, which show the antimicrobial activity against Gram-negative and Gram-positive bacteria, fungi, and viruses (Song and Lee, 2014). The cecropins also improved the performance of piglets infected with E. coli and increased the population of Lactobacilli strains that have a beneficial effect on the gut health (Wu et al., 2012). Bovine myeloid antimicrobial peptides (BMAP), bovine cathelicidins, are synthetic host defense peptides, showing antibacterial activity against S. aureus, B. megaterium, E. coli, P. aeruginosa, and S. enterica serotype Typhimurium (Skerlavaj et al., 1996). Ovodefensins expressed in the oviducts of chickens and ducks show strong antibacterial activity against E. coli, avian pathogenic E. coli, and S. aureus (Whenham et al., 2015). In addition, as avian β-defensins show broad antimicrobial activity against Gram-negative and Gram-positive bacteria and fungi (van Dijk et al., 2008; Whenham et al., 2015). AMPs are one of the most promising antibiotic alternatives applicable to food animals as immune modulators (Pasupuleti et al., 2012).
Bacteriophages
Bacteriophages have been used to treat acute and chronic infections due to their strong host specificity and less adverse effects (Wittebole et al., 2014). Recently, bacteriophages have regained attention as antibiotic alternatives with increasing the emergence of multidrug-resistant bacteria and decreasing the discovery of novel antibiotics (Principi et al., 2019). In particular, bacteriophages can effectively control zoonotic bacterial pathogens such as Salmonella spp., E. coli, Campylobacter spp., and Listeria spp., that cause infection of food animals and contamination of food (Gambino and Brondsted, 2021; Gigante and Atterbury, 2019). Broilers infected by E. coli were treated with bacteriophages, resulting in the significant reduction in mortality (Huff et al., 2004). The inhibitory effect of bacteriophages was also observed in pigs infected by Salmonella enterica in the ileum and cecum (Wall et al., 2010). The US Food and Drug Administration (FDA) and/or the US Department of Agriculture (USDA) has approved the use of bacteriophages to control pathogens in food animals, food crops, and meat (O'Flaherty et al., 2009). For example, FDA has approved the use of 6-cocktails for controlling Listeria monocytogenes contamination in ready-to-eat meat (Lang, 2006). Recently, bacteriophage-encoding enzymes such as endolysin, holin, and hydrolases have been used to overcome phage resistance. (Cheng et al., 2014; Loc-Carrillo and Abedon, 2011; Pirnay et al., 2011; Roach and Donovan, 2015). Endolysins are responsible for attacking and disrupting bacterial cell wall peptidoglycan that enables bacteria to withstand turgor and maintains cell shape (Roach and Donovan, 2015; Vollmer et al., 2008). These muralytic enzymes have effective antibacterial activity against MRSA and other Gram-positive bacterial pathogens such as Staphylococcus, Bacillus anthracis, L. monocytogenes, Clostridium butyricum, Enterococcus faecalis, C. perfringens, and Group B Streptococcus (Fenton et al., 2010; Low et al., 2005; O'Flaherty et al., 2005).
Probiotics
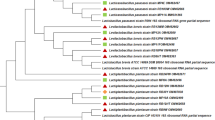
Probiotics are living bacteria and yeasts that have beneficial effects on humans and animals (Nagpal et al., 2012). Food and Agriculture Organization of the United Nations (FAO)/World Health Organization (WHO) defined probiotics as “live microorganisms confer a health effect on the host when consumed in adequate amount”. Most probiotics are present in the gastrointestinal (GI) tract of humans and animals, and they beneficially affect host animals by improving the host’s intestinal microbial balance or improving the properties of the indigenous microflora (Delia et al., 2012). In addition, probiotics have various beneficial effects on food animals, including the improvement of nutrient absorption ability and milk (or egg) production (Delia et al., 2012; Perdigón et al., 2001). Probiotics effectively prevented diarrhea and reduced mortality in pig infected by E. coli. Bifidobacterium lactis HN019 also relieved weanling diarrhea of piglets caused by rotavirus and E. coli by enhancing the immune system (Shu et al., 2001). Probiotic administration reduced the mortality rate of broilers by 22% and increased the production efficiency (Dersjant-Li et al., 2014). In addition, the broilers treated with probiotics containing Lactobacillus, Bifidobacterium, Enterococcus, and Pediococcus strains improved the growth compared to avilamycin-treated broilers (Markowiak and Slizewska, 2018; Mountzouris et al., 2007). In the cattle, probiotics are widely used for preventing disease and improving productivity (Frola et al., 2012; Nader-Macias et al., 2008). For example, when Lactobacillus perolens CRL 1724 was used to treat bovine mastitis in dairy farms instead of antibiotic therapy (Frola et al., 2012). Moreover, probiotic added in the calf diet significantly reduced the incidence of diarrhea and beneficially affected the lactic acid bacteria (Signorini et al., 2012).
Probiotics has been considered as alternatives over antibiotics in food industry, medical field, and agriculture (Reininghaus et al., 2020; Varankovich et al., 2015). However, the use of probiotics is limited due to their potential reservoirs for ARGs. Therefore, probiotics may not be excluded from the transfer of ARGs (Imperial and Ibana, 2016). In general, the antibiotic resistance in bacteria includes inherent and acquired resistance. Antibiotic resistance in bacteria can occur through the mutation of an endogenous gene and the acquisition of exogeneous ARGs (Liu et al., 2009). The inhered resistance occurs naturally in all bacterial species, known as nontransferable (Teuber, 1999). The tet(W) in B. animalis subsp. lactis is intrinsic resistance gene that are not transferable (Nøhr-Meldgaard et al., 2021). The acquired resistance confers ARGs through HGT (Lokesh et al., 2019). The mechanisms of acquired resistance in bacteria include membrane permeability modification, efflux pump system, enzymatic degradation, target-site variation, and metabolic rearrangement (Courvalin, 2006; Tóth et al., 2021). The acquired antibiotic resistance in probiotics is involved in the transfer of ARGs in the gastrointestinal tract (GIT) (Selvin et al., 2020). The transferable genes conferring the acquired resistance have been observed in lactobacilli, including tet(M) responsible for tetracycline resistance, erm(B) for erythromycin resistance, and cat for chloramphenicol resistance (Ammor et al., 2007). Therefore, the genetic exchanges and health risk of ARGs need to be assessed based on whether intrinsic or acquired resistance genes (van Reenen and Dicks, 2011).
In conclusion, the risk of antibiotic resistance has been a global problem in food system. Antibiotics are known as effective therapeutic agents for the treatment of bacterial infectious diseases of food-producing animals. However, as the double-edged sword of antibiotics, the possible carry-over of residual antibiotics and the potential reservoir of ARGs through the food chain from farm to table are the high priority health issues. The residual antibiotics in food animals can affect the evolution of antibiotic resistance in foodborne pathogens. Furthermore, the transfer of ARGs can accelerate the emergence and spread of antibiotic-resistant pathogens. The use of antibiotics in farming animals should not be underestimated in terms of food safety and public health. Therefore, other than the regulations that passively restrict the use of antibiotics in farm animals, the discovery and development of effective prevention, control, and treatment strategies are needed to reduce the risk of residual antibiotics and ARGs.
References
Aarestrup FM. The livestock reservoir for antimicrobial resistance: a personal view on changing patterns of risks, effects of interventions and the way forward. Philosophical Transactions of the Royal Society of London Series B Biological Sciences. 370: 20140085 (2015)
Abachin E, Poyart C, Pellegrini E, Milohanic E, Fiedler F, Berche P, Trieu-Cuot P. Formation of D-alanyl-lipoteichoic acid is required for adhesion and virulence of Listeria monocytogenes. Molecular Microbiology.. 43: 1-14 (2002)
Abriouel H, Casado Muñoz MDC, Lavilla Lerma L, Pérez Montoro B, Bockelmann W, Pichner R, Kabisch J, Cho GS, Franz C, Gálvez A, Benomar N. New insights in antibiotic resistance of Lactobacillus species from fermented foods. Food Research International. 78: 465-481 (2015)
Adak GK, Cowden JM, Nicholas S, Evans HS. The Public Health Laboratory Service national case-control study of primary indigenous sporadic cases of campylobacter infection. Epidemiology and Infection. 115: 15-22 (1995)
Ahmed AM, Shimamoto T. Molecular analysis of multidrug resistance in Shiga toxin-producing Escherichia coli O157:H7 isolated from meat and dairy products. International Journal of Food Microbiology. 193: 68-73 (2015)
Aires-de-Sousa M. Methicillin-resistant Staphylococcus aureus among animals: current overview. Clinical Microbiology and Infection 23: 373-380 (2017)
Alexander TW, Yanke JL, Reuter T, Topp E, Read RR, Selinger BL, McAllister TA. Longitudinal characterization of antimicrobial resistance genes in feces shed from cattle fed different subtherapeutic antibiotics. BMC Microbiology. 11: 1-12 (2011)
Amador P, Fernandes R, Prudencio C, Duarte I. Prevalence of antibiotic resistance genes in multidrug-resistant Enterobacteriaceae on portuguese livestock manure. Antibiotics. 8: 23 (2019)
Ammor MS, Flórez AB, Mayo B. Antibiotic resistance in non-enterococcal lactic acid bacteria and bifidobacteria. Food Microbiology. 24: 559-570 (2007)
Andres-Lasheras S, Jelinski M, Zaheer R, McAllister TA. Bovine respiratory disease: Conventional to culture-independent approaches to studying antimicrobial resistance in North America. Antibiotics. 11: 487 (2022)
Anee IJ, Alam S, Begum RA, Shahjahan RM, Khandaker AM. The role of probiotics on animal health and nutrition. The Journal of Basic and Applied Zoology. 82: 1-16 (2021)
Arango-Argoty GA, Dai D, Pruden A, Vikesland P, Heath LS, Zhang L. NanoARG: a web service for detecting and contextualizing antimicrobial resistance genes from nanopore-derived metagenomes. Microbiome. 7: 88 (2019)
Aslam B, Khurshid M, Arshad MI, Muzammil S, Rasool M, Yasmeen N, Shah T, Chaudhry TH, Rasool MH, Shahid A, Xueshan X, Baloch Z. Antibiotic resistance: one health one world outlook. Frontiers in Cellular and Infection Microbiology. 11: 771510 (2021)
Aust MO, Godlinski F, Travis GR, Hao X, McAllister TA, Leinweber P, Thiele-Bruhn S. Distribution of sulfamethazine, chlortetracycline and tylosin in manure and soil of Canadian feedlots after subtherapeutic use in cattle. Environmental Pollution. 156: 1243-1251 (2008)
Auvynet C, Rosenstein Y. Multifunctional host defense peptides: antimicrobial peptides, the small yet big players in innate and adaptive immunity. The FEBS Journal. 276: 6497-6508 (2009)
Awosile BB, Heider LC, Saab ME, McClure J. Antimicrobial resistance in mastitis, respiratory and enteric bacteria isolated from ruminant animals from the Atlantic Provinces of Canada from 1994–2013. The Canadian Veterinary Journal. 59: 1099 (2018)
Babakhani S, Oloomi M. Transposons: the agents of antibiotic resistance in bacteria. Journal of Basic Microbiology. 58: 905-917 (2018)
Bak H, Rathkjen PH. Reduced use of antimicrobials after vaccination of pigs against porcine proliferative enteropathy in a Danish SPF herd. Acta Veterinaria Scandinavica. 51: 1-4 (2009)
Barrow PA. Salmonella infections: immune and non-immune protection with vaccines. Avian Pathology. 36: 1-13 (2007)
Bay DC, Rommens KL, Turner RJ. Small multidrug resistance proteins: a multidrug transporter family that continues to grow. Biochim Biophys Acta. 1778: 1814-1838 (2008)
Beceiro A, Tomás M, Bou G. Antimicrobial resistance and virulence: a successful or deleterious association in the bacterial world? Clinical Microbiology Reviews. 26: 185-230 (2013)
Begić M, Josić D. Biofilm formation and extracellular microvesicles—The way of foodborne pathogens toward resistance. Electrophoresis. 41: 1718-1739 (2020)
Ben Y, Fu C, Hu M, Liu L, Wong MH, Zheng C. Human health risk assessment of antibiotic resistance associated with antibiotic residues in the environment: A review. Environmental Research. 169: 483-493 (2019)
Blair JMA, Webber MA, Baylay AJ, Ogbolu DO, Piddock LJV. Molecular mechanisms of antibiotic resistance. Nature Reviews Microbiology. 13: 42-51 (2015)
Blecha F. Immunomodulators for prevention and treatment of infectious diseases in food-producing animals. The Veterinary Clinics of North America. Food Animal Practice. 17: 621-633 (2001)
Borges V, Santos A, Correia CB, Saraiva M, Menard A, Vieira L, Sampaio DA, Pinheiro M, Gomes JP, Oleastro M. Helicobacter pullorum isolated from fresh chicken meat: antibiotic resistance and genomic traits of an emerging foodborne pathogen. Applied and Environmental Microbiology. 81: 8155-8163 (2015)
Bricknell I, Dalmo RA. The use of immunostimulants in fish larval aquaculture. Fish and Shellfish Immunology. 19: 457-472 (2005)
Cao S, Huseby DL, Brandis G, Hughes D. Alternative evolutionary pathways for drug-resistant small colony variant mutants in Staphylococcus aureus. mBio. 8: e00358-00317 (2017)
Chambers L, Yang Y, Littier H, Ray P, Zhang T, Pruden A, Strickland M, Knowlton K. Metagenomic analysis of antibiotic resistance genes in dairy cow feces following therapeutic administration of third generation cephalosporin. PLoS One. 10: e0133764 (2015)
Charrel RN, Pagès JM, De Micco P, Mallea M. Prevalence of outer membrane porin alteration in beta-lactam-antibiotic-resistant Enterobacter aerogenes. Antimicrobial Agents and Chemotherapy. 40: 2854-2858 (1996)
Chen J, Fluharty FL, St-Pierre N, Morrison M, Yu Z. Technical note: Occurrence in fecal microbiota of genes conferring resistance to both macrolide-lincosamide-streptogramin B and tetracyclines concomitant with feeding of beef cattle with tylosin. Journal of Animal Science. 86: 2385-2391 (2008)
Chen J, Ying GG, Deng WJ. Antibiotic residues in food: extraction, analysis, and human health concerns. Journal of Agricultural and Food Chemistry. 67: 7569-7586 (2019)
Cheng G, Hao H, Xie S, Wang X, Dai M, Huang L, Yuan Z. Antibiotic alternatives: the substitution of antibiotics in animal husbandry? Frontiers in Microbiology. 5: 217 (2014)
Coates AR, Halls G, Hu Y. Novel classes of antibiotics or more of the same? British Journal of Pharmacology. 163: 184-194 (2011)
Colavecchio A, Cadieux B, Lo A, Goodridge LD. Bacteriophages contribute to the spread of antibiotic resistance genes among foodborne pathogens of the Enterobacteriaceae family - A Review. Frontiers in Microbiology. 8: 1108 (2017)
Cornaglia G, Mazzariol A, Fontana R, Satta G. Diffusion of carbapenems through the outer membrane of enterobacteriaceae and correlation of their activities with their periplasmic concentrations. Microbial Drug Resistance. 2: 273-276 (1996)
Cotter PD, Ross RP, Hill C. Bacteriocins - a viable alternative to antibiotics? Nature Reviews Microbiology. 11: 95-105 (2013)
Courvalin P. Antibiotic resistance: the pros and cons of probiotics. Digestive and Liver Disease. 38: S261-265 (2006)
Coyne LA, Latham SM, Dawson S, Donald IJ, Pearson RB, Smith RF, Williams NJ, Pinchbeck GL. Exploring perspectives on antimicrobial use in livestock: A mixed-methods study of UK pig farmers. Frontiers in Veterinary Science. 6: 257 (2019)
Culp EJ, Waglechner N, Wang W, Fiebig-Comyn AA, Hsu Y-P, Koteva K, Sychantha D, Coombes BK, Van Nieuwenhze MS, Brun YV, Wright GD. Evolution-guided discovery of antibiotics that inhibit peptidoglycan remodelling. Nature. 578: 582-587 (2020)
da Silva AC, Rodrigues MX, Silva NCC. Methicillin-resistant Staphylococcus aureus in food and the prevalence in Brazil: a review. Brazilian Journal of Microbiology. 51: 347-356 (2020)
Dalloul RA, Lillehoj HS. Poultry coccidiosis: recent advancements in control measures and vaccine development. Expert Review of Anti-infective Therapy. 5: 143-163 (2006)
Danelon C, Nestorovich EM, Winterhalter M, Ceccarelli M, Bezrukov SM. Interaction of zwitterionic penicillins with the OmpF channel facilitates their translocation. Biophysical Journal. 90: 1617-1627 (2006)
Davidson AL, Dassa E, Orelle C, Chen J. Structure, function, and evolution of bacterial ATP-binding cassette systems. Microbiology and Molecular Biology Reviews. 72: 317-364 (2008)
De R. Mobile genetic elements of Vibrio cholerae and the evolution of its antimicrobial resistance. Frontiers in Tropical Diseases. 2: 691604 (2021)
del Castillo FJ, del Castillo I, Moreno F. Construction and characterization of mutations at codon 751 of the Escherichia coli gyrB gene that confer resistance to the antimicrobial peptide microcin B17 and alter the activity of DNA gyrase. Journal of Bacteriology. 183: 2137-2140 (2001)
Delcour AH. Outer membrane permeability and antibiotic resistance. Biochim Biophys Acta. 1794: 808-816 (2009)
Delia E, Tafaj M, Manner K. Efficiency of probiotics in farm animals. Probiotic in Animals. 247–272 (2012)
Delsart M, Pol F, Dufour B, Rose N, Fablet C. Pig farming in alternative systems: Strengths and challenges in terms of animal welfare, biosecurity, animal health and pork safety. Agriculture. 10: 261 (2020)
Dersjant-Li Y, Awati A, Kromm C, Evans C. A direct fed microbial containing a combination of three-strain Bacillus sp. can be used as an alternative to feed antibiotic growth promoters in broiler production. Journal of Applied Animal Nutrition. 2 (2014)
Diraviyam T, Zhao B, Wang Y, Schade R, Michael A, Zhang X. Effect of chicken egg yolk antibodies (IgY) against diarrhea in domesticated animals: a systematic review and meta-analysis. PLoS One. 9: e97716 (2014)
Dutil L, Irwin R, Finley R, Ng LK, Avery B, Boerlin P, Bourgault AM, Cole L, Daignault D, Desruisseau A, Demczuk W, Hoang L, Horsman GB, Ismail J, Jamieson F, Maki A, Pacagnella A, Pillai DR. Ceftiofur resistance in Salmonella enterica serovar Heidelberg from chicken meat and humans, Canada. Emerging Infectious Diseases. 16: 48-54 (2010)
Economou V, Gousia P. Agriculture and food animals as a source of antimicrobial-resistant bacteria. Infection and Drug Resistance. 8: 49-61 (2015)
Eicher SD, McKee CA, Carroll JA, Pajor EA. Supplemental vitamin C and yeast cell wall beta-glucan as growth enhancers in newborn pigs and as immunomodulators after an endotoxin challenge after weaning. Journal of Animal Science. 84: 2352-2360 (2006)
El-Halfawy OM, Klett J, Ingram RJ, Loutet SA, Murphy ME, Martín-Santamaría S, Valvano MA. Antibiotic capture by bacterial lipocalins uncovers an extracellular mechanism of intrinsic antibiotic resistance. mBio. 8: e00225-00217 (2017)
Eliopoulos GM, Huovinen P. Resistance to trimethoprim-sulfamethoxazole. Clinical Infectious Diseases. 32: 1608-1614 (2001)
Emond-Rheault JG, Hamel J, Jeukens J, Freschi L, Kukavica-Ibrulj I, Boyle B, Tamber S, Malo D, Franz E, Burnett E, Daigle F, Arya G, Sanderson K, Wiedmann M, Slawson RM, Weadge JT, Stephan R, Bekal S, Gruenheid S, Goodridge LD, Levesque RC. The Salmonella enterica plasmidome as a reservoir of antibiotic resistance. Microorganisms. 8: 1016 (2020)
Endtz HP, Ruijs GJ, van Klingeren B, Jansen WH, van der Reyden T, Mouton RP. Quinolone resistance in Campylobacter isolated from man and poultry following the introduction of fluoroquinolones in veterinary medicine. Journal of Antimicrobial Chemotherapy. 27: 199-208 (1991)
Engberg J, Aarestrup FM, Taylor DE, Gerner-Smidt P, Nachamkin I. Quinolone and macrolide resistance in Campylobacter jejuni and C. coli: resistance mechanisms and trends in human isolates. Emerging Infectious Diseases. 7: 24-34 (2001)
Fasina YO, Obanla T, Dosu G, Muzquiz S. Significance of endogenous antimicrobial peptides on the health of food animals. Frontiers in Veterinary Science. 8: 585266 (2021)
Fenton M, McAuliffe O, O’Mahony J, Coffey A. Recombinant bacteriophage lysins as antibacterials. Bioengineered Bugs. 1: 9-16 (2010)
Flensburg J, Skold O. Massive overproduction of dihydrofolate reductase in bacteria as a response to the use of trimethoprim. European Journal of Biochemistry. 162: 473-476 (1987)
Fletcher S. Understanding the contribution of environmental factors in the spread of antimicrobial resistance. Environmental Health and Preventive Medicine. 20: 243-252 (2015)
Founou LL, Founou RC, Essack SY. Antibiotic resistance in the food chain: A developing country-perspective. Frontiers in Microbiology. 7: 1881 (2016)
Frola ID, Pellegrino MS, Espeche MC, Giraudo JA, Nader-Macias ME, Bogni CI. Effects of intramammary inoculation of Lactobacillus perolens CRL1724 in lactating cows' udders. Journal of Dairy Research. 79: 84-92 (2012)
Fujimoto-Nakamura M, Ito H, Oyamada Y, Nishino T, Yamagishi J. Accumulation of mutations in both gyrB and parE genes is associated with high-level resistance to novobiocin in Staphylococcus aureus. Antimicrobial Agents and Chemotherapy. 49: 3810-3815 (2005)
Gadde U, Kim WH, Oh ST, Lillehoj HS. Alternatives to antibiotics for maximizing growth performance and feed efficiency in poultry: a review. Animal Health Research Reviews. 18: 26-45 (2017)
Gambino M, Brondsted L. Looking into the future of phage-based control of zoonotic pathogens in food and animal production. Current Opinion in Biotechnology. 68: 96-103 (2021)
Ghosh S, Mehla RK, Sirohi SK, Tomar SK. Performance of crossbred calves with dietary supplementation of garlic extract. Journal of Animal Physiology and Animal Nutrition. 95: 449-455 (2011)
Gigante A, Atterbury RJ. Veterinary use of bacteriophage therapy in intensively-reared livestock. Virology Journal. 16: 1-9 (2019)
Goldstein BP. Resistance to rifampicin: a review. Journal of Antibiotics. 67: 625-630 (2014)
Gonzalez Ronquillo M, Angeles Hernandez JC. Antibiotic and synthetic growth promoters in animal diets: review of impact and analytical methods. Food Control. 72: 255-267 (2017)
Gouliouris T, Raven KE, Ludden C, Blane B, Corander J, Horner CS, Hernandez-Garcia J, Wood P, Hadjirin NF, Radakovic M, Holmes MA, de Goffau M, Brown NM, Parkhill J, Peacock SJ. Genomic surveillance of Enterococcus faecium reveals limited sharing of strains and resistance genes between livestock and humans in the United Kingdom. mBio. 9: e01780-01718 (2018)
Haack BJ, Andrews RE, Jr. Isolation of Tn916-like conjugal elements from swine lot effluent. Canadian Journal of Microbiology. 46: 542-549 (2000)
Hawkey PM. Mechanisms of quinolone action and microbial response. Journal of Antimicrobial Chemotherapy. 51 Suppl 1: 29-35 (2003)
Helms M, Simonsen J, Mølbak K. Quinolone resistance is associated with increased risk of invasive illness or death during infection with Salmonella serotype Typhimurium. Journal of Infectious Diseases. 190: 1652-1654 (2004)
Hoelzer K, Bielke L, Blake DP, Cox E, Cutting SM, Devriendt B, Erlacher-Vindel E, Goossens E, Karaca K, Lemiere S, Metzner M, Raicek M, Collell Surinach M, Wong NM, Gay C, Van Immerseel F. Vaccines as alternatives to antibiotics for food producing animals. Part 1: challenges and needs. Veterinary Research. 49: 1-15 (2018)
Holani R, Shah C, Haji Q, Inglis GD, Uwiera RRE, Cobo ER. Proline-arginine rich (PR-39) cathelicidin: Structure, expression and functional implication in intestinal health. Comparative Immunology, Microbiology and Infectious Diseases. 49: 95-101 (2016)
Hooper DC, Jacoby GA. Topoisomerase inhibitors: Fluoroquinolone mechanisms of action and resistance. Cold Spring Harbor Perspectives in Medicine. 6: a025320 (2016)
Huff W, Huff G, Rath N, Balog J, Donoghue A. Therapeutic efficacy of bacteriophage and Baytril (enrofloxacin) individually and in combination to treat colibacillosis in broilers. Poultry Science. 83: 1944-1947 (2004)
Hughes D, Andersson DI. Environmental and genetic modulation of the phenotypic expression of antibiotic resistance. FEMS Microbiology Reviews. 41: 374-391 (2017)
Idowu F, Junaid K, Paul A, Gabriel O, Paul A, Sati N, Maryam M, Jarlath U. Antimicrobial screening of commercial eggs and determination of tetracycline residue using two microbiological methods. International Journal of Poultry Science. 09: 959-962 (2010)
Imperial ICVJ, Ibana JA. Addressing the antibiotic resistance problem with probiotics: Reducing the risk of its double-edged sword effect. Frontiers in Microbiology. 7: 1983-1983 (2016)
Iovine NM. Resistance mechanisms in Campylobacter jejuni. Virulence. 4: 230-240 (2013)
Jiao W, Ma Q, Lv X, Shan A, Li Z. Gene expression and tissue distribution of β-defensins in Chinese Min pigs and Landrace pigs. Czech Journal of Animal Science. 62: 178-183 (2017)
Jores J, Mariner JC, Naessens J. Development of an improved vaccine for contagious bovine pleuropneumonia: an African perspective on challenges and proposed actions. Veterinary Research. 44: 1-5 (2013)
Kang H-K, Park Y. Glycopeptide antibiotics: Structure and mechanisms of action. Journal of Bacteriology and Virology. 45: 67-78 (2015)
Kang Y, Li Q, Yin Z, Shen M, Zhao H, Bai Y, Mei L, Hu J. High diversity and abundance of cultivable tetracycline-resistant bacteria in soil following pig manure application. Scientific Reports. 8: 1489 (2018)
Kapoor G, Saigal S, Elongavan A. Action and resistance mechanisms of antibiotics: A guide for clinicians. Journal of Anaesthesiology, Clinical Pharmacology. 33: 300-305 (2017)
Karaman R, Jubeh B, Breijyeh Z. Resistance of Gram-positive bacteria to current antibacterial agents and overcoming approaches. Molecules. 25: 2888 (2020)
Kelly BG, Vespermann A, Bolton DJ. Horizontal gene transfer of virulence determinants in selected bacterial foodborne pathogens. Food and Chemical Toxicology. 47: 969-977 (2009)
Khalid A, Lubián AF, Ma L, Lin RCY, Iredell JR. Characterizing the role of porin mutations in susceptibility of beta lactamase producing Klebsiella pneumoniae isolates to ceftaroline and ceftaroline-avibactam. International Journal of Infectious Diseases. 93: 252-257 (2020)
Khameneh B, Diab R, Ghazvini K, Fazly Bazzaz BS. Breakthroughs in bacterial resistance mechanisms and the potential ways to combat them. Microbial Pathogenesis. 95: 32-42 (2016)
Komora N, Bruschi C, Magalhães R, Ferreira V, Teixeira P. Survival of Listeria monocytogenes with different antibiotic resistance patterns to food-associated stresses. International Journal of Food Microbiology. 245: 79-87 (2017)
Koo H, Ryu SH, Ahn HJ, Jung WK, Park YK, Kwon NH, Kim SH, Kim JM, Yoo BW, Choi SI, Davis WC, Park YH. Immunostimulatory effects of the anionic alkali mineral complex Barodon on equine lymphocytes. Clinical and Vaccine Immunology. 13: 1255-1266 (2006)
Kourtesi C, Ball AR, Huang Y-Y, Jachak SM, Vera DMA, Khondkar P, Gibbons S, Hamblin MR, Tegos GP. Microbial efflux systems and inhibitors: Approaches to drug discovery and the challenge of clinical implementation. The Open Microbiology Journal. 7: 34-52 (2013)
Kramer NE, van Hijum SA, Knol J, Kok J, Kuipers OP. Transcriptome analysis reveals mechanisms by which Lactococcus lactis acquires nisin resistance. Antimicrobial Agents and Chemotherapy. 50: 1753-1761 (2006)
Kumar A, Schweizer HP. Bacterial resistance to antibiotics: active efflux and reduced uptake. Advanced Drug Delivery Reviews. 57: 1486-1513 (2005)
Kumar S, Lekshmi M, Parvathi A, Ojha M, Wenzel N, Varela MF. Functional and structural roles of the major facilitator superfamily bacterial multidrug efflux pumps. Microorganisms. 8: 266 (2020)
Kumar S, Mukherjee MM, Varela MF. Modulation of bacterial multidrug resistance efflux pumps of the major facilitator superfamily. International Journal of Bacteriology. 2013: 1-15 (2013)
Kuroda T, Tsuchiya T. Multidrug efflux transporters in the MATE family. Biochim Biophys Acta. 1794: 763-768 (2009)
Kusakizako T, Miyauchi H, Ishitani R, Nureki O. Structural biology of the multidrug and toxic compound extrusion superfamily transporters. Biochimica et Biophysica Acta. Biomembranes. 1862: 183154 (2020)
Lang LH. FDA approves use of bacteriophages to be added to meat and poultry products. Gastroenterology. 131: 1370 (2006)
Lazarus B, Paterson DL, Mollinger JL, Rogers BA. Do human extraintestinal Escherichia coli infections resistant to expanded-spectrum cephalosporins originate from food-producing animals? A systematic review. Clinical Infectious Diseases. 60: 439-452 (2015)
Leclerc QJ, Lindsay JA, Knight GM. Mathematical modelling to study the horizontal transfer of antimicrobial resistance genes in bacteria: current state of the field and recommendations. Journal of the Royal Society Interface. 16: 20190260 (2019)
Lee SH, Jang SI, Kim DK, Ionescu C, Bravo D, Lillehoj HS. Effect of dietary curcuma, capsicum, and lentinus on enhancing local immunity against Eimeria acervulina infection. The Journal of Poultry Science. 47: 89-95 (2009)
Lee SH, Lillehoj HS, Jang SI, Lee KW, Park MS, Bravo D, Lillehoj EP. Cinnamaldehyde enhances in vitro parameters of immunity and reduces in vivo infection against avian coccidiosis. The British Journal of Nutrition. 106: 862-869 (2011)
Lekagul A, Tangcharoensathien V, Yeung S. Patterns of antibiotic use in global pig production: A systematic review. Veterinary and Animal Science. 7: 100058 (2019)
Leonard AFC, Zhang L, Balfour AJ, Garside R, Hawkey PM, Murray AK, Ukoumunne OC, Gaze WH. Exposure to and colonisation by antibiotic-resistant E. coli in UK coastal water users: Environmental surveillance, exposure assessment, and epidemiological study (Beach Bum Survey). Environment International. 114: 326-333 (2018)
Lewis HC, Molbak K, Reese C, Aarestrup FM, Selchau M, Sorum M, Skov RL. Pigs as source of methicillin-resistant Staphylococcus aureus CC398 infections in humans, Denmark. Emerging Infectious Diseases. 14: 1383-1389 (2008)
Lewis VG, Ween MP, McDevitt CA. The role of ATP-binding cassette transporters in bacterial pathogenicity. Protoplasma. 249: 919-942 (2012)
Li XZ, Plesiat P, Nikaido H. The challenge of efflux-mediated antibiotic resistance in Gram-negative bacteria. Clinical Microbiology Reviews. 28: 337-418 (2015)
Liao X, Ma Y, Daliri EB-M, Koseki S, Wei S, Liu D, Ye X, Chen S, Ding T. Interplay of antibiotic resistance and food-associated stress tolerance in foodborne pathogens. Trends in Food Science and Technology. 95: 97-106 (2020)
Lillehoj H, Liu Y, Calsamiglia S, Fernandez-Miyakawa ME, Chi F, Cravens RL, Oh S, Gay CG. Phytochemicals as antibiotic alternatives to promote growth and enhance host health. Veterinary Research. 49: 1-18 (2018)
Lin J, Nishino K, Roberts MC, Tolmasky M, Aminov R, Zhang L. Mechanisms of antibiotic resistance. Frontiers in Microbiology. 6 (2015)
Lioy VS, Goussard S, Guerineau V, Yoon EJ, Courvalin P, Galimand M, Grillot-Courvalin C. Aminoglycoside resistance 16S rRNA methyltransferases block endogenous methylation, affect translation efficiency and fitness of the host. RNA. 20: 382-391 (2014)
Liu C, Zhang Z-Y, Dong K, Yuan J-P, Guo X-K. Antibiotic resistance of probiotic strains of lactic acid bacteria isolated from marketed foods and drugs. Biomedical and Environmental Sciences. 22: 401-412 (2009)
Liu Y, Song M, Che T, Lee J, Bravo D, Maddox C, Pettigrew J. Dietary plant extracts modulate gene expression profiles in ileal mucosa of weaned pigs after an Escherichia coli infection. Journal of Animal Science. 92: 2050-2062 (2014)
Livermore DM. Defining an extended-spectrum beta-lactamase. Clinical Microbiology and Infection. 14 Suppl 1: 3-10 (2008)
Loc-Carrillo C, Abedon ST. Pros and cons of phage therapy. Bacteriophage. 1: 111-114 (2011)
Lokesh D, Rajagopal K, Shin JH. Multidrug resistant probiotics as an alternative to antibiotic probiotic therapy. Journal of Infectiology. 2: 46-49 (2019)
Looft T, Johnson TA, Allen HK, Bayles DO, Alt DP, Stedtfeld RD, Sul WJ, Stedtfeld TM, Chai B, Cole JR, Hashsham SA, Tiedje JM, Stanton TB. In-feed antibiotic effects on the swine intestinal microbiome. Proceedings of the National Academy of Sciences. 109: 1691-1696 (2012)
Low LY, Yang C, Perego M, Osterman A, Liddington RC. Structure and lytic activity of a Bacillus anthracis prophage endolysin. Journal of Biological Chemistry. 280: 35433-35439 (2005)
Ma L, Li B, Jiang XT, Wang YL, Xia Y, Li AD, Zhang T. Catalogue of antibiotic resistome and host-tracking in drinking water deciphered by a large scale survey. Microbiome. 5: 154 (2017)
Ma Y, Lan G, Li C, Cambaza EM, Liu D, Ye X, Chen S, Ding T. Stress tolerance of Staphylococcus aureus with different antibiotic resistance profiles. Microbial Pathogenesis. 133: 103549 (2019)
Maidhof H, Guerra B, Abbas S, Elsheikha HM, Whittam TS, Beutin L. A multiresistant clone of Shiga toxin-producing Escherichia coli O118:[H16] is spread in cattle and humans over different European countries. Applied and Environmental Microbiology. 68: 5834-5842 (2002)
Malanovic N, Lohner K. Gram-positive bacterial cell envelopes: The impact on the activity of antimicrobial peptides. Biochimica et Biophysica Acta (BBA) - Biomembranes. 1858: 936-946 (2016)
Malik AA, Hussain H, Creswell J, Siddiqui S, J FA, Madhani F, Habib A, Khan AJ, Amanullah F. The impact of funding on childhood TB case detection in Pakistan. Tropical Medicine and Infectious Disease. 4: 146 (2019)
Mao X, Qi S, Yu B, Huang Z, Chen H, Mao Q, Han G, Chen D. Dietary L-arginine supplementation enhances porcine β-defensins gene expression in some tissues of weaned pigs. Livestock Science. 148: 103-108 (2012)
Markowiak P, Slizewska K. The role of probiotics, prebiotics and synbiotics in animal nutrition. Gut Pathogens. 10: 1-20 (2018)
Miller WR, Munita JM, Arias CA. Mechanisms of antibiotic resistance in enterococci. Expert Review of Anti-infective Therapy. 12: 1221-1236 (2014)
Mir RA, Kudva IT. Antibiotic-resistant Shiga toxin-producing Escherichia coli: An overview of prevalence and intervention strategies. Zoonoses and Public Health. 66: 1-13 (2019)
Mombarg M, Bouzoubaa K, Andrews S, Vanimisetti HB, Rodenberg J, Karaca K. Safety and efficacy of an aroA-deleted live vaccine against avian colibacillosis in a multicentre field trial in broilers in Morocco. Avian Pathology. 43: 276-281 (2014)
Monger XC, Gilbert AA, Saucier L, Vincent AT. Antibiotic resistance: From pig to meat. Antibiotics. 10: 1209 (2021)
Mountzouris KC, Tsirtsikos P, Kalamara E, Nitsch S, Schatzmayr G, Fegeros K. Evaluation of the efficacy of a probiotic containing Lactobacillus, Bifidobacterium, Enterococcus, and Pediococcus strains in promoting broiler performance and modulating cecal microflora composition and metabolic activities. Poultry Science. 86: 309-317 (2007)
Munita JM, Arias CA. Mechanisms of antibiotic resistance. Microbiology Spectrum. 4: 4-2 (2016)
Munk P, Knudsen BE, Lukjancenko O, Duarte ASR, Van Gompel L, Luiken REC, Smit LAM, Schmitt H, Garcia AD, Hansen RB, Petersen TN, Bossers A, Ruppe E, Group E, Lund O, Hald T, Pamp SJ, Vigre H, Heederik D, Wagenaar JA, Mevius D, Aarestrup FM. Abundance and diversity of the faecal resistome in slaughter pigs and broilers in nine European countries. Nature Microbiology. 3: 898-908 (2018)
Nader-Macias ME, Otero MC, Espeche MC, Maldonado NC. Advances in the design of probiotic products for the prevention of major diseases in dairy cattle. Journal of Industrial Microbiology and Biotechnology. 35: 1387-1395 (2008)
Nagpal R, Kumar A, Kumar M, Behare PV, Jain S, Yadav H. Probiotics, their health benefits and applications for developing healthier foods: a review. FEMS Microbiology Letters. 334: 1-15 (2012)
Nasiri MJ, Haeili M, Ghazi M, Goudarzi H, Pormohammad A, Imani Fooladi AA, Feizabadi MM. New insights in to the intrinsic and acquired drug resistance mechanisms in Mycobacteria. Frontiers in Microbiology. 8 (2017)
Nestorovich EM, Danelon C, Winterhalter M, Bezrukov SM. Designed to penetrate: Time-resolved interaction of single antibiotic molecules with bacterial pores. Proceedings of the National Academy of Sciences. 99: 9789-9794 (2002)
Nhung NT, Chansiripornchai N, Carrique-Mas JJ. Antimicrobial resistance in bacterial poultry pathogens: A review. Frontiers in Veterinary Science. 4: 126 (2017)
Nishino K, Yamaguchi A. Analysis of a complete library of putative drug transporter genes in Escherichia coli. Journal of Bacteriology. 183: 5803-5812 (2001)
Nøhr-Meldgaard K, Struve C, Ingmer H, Agersø Y. The tetracycline resistance gene, tet(W) in Bifidobacterium animalis subsp. lactis follows phylogeny and differs from tet(W) in other species. Frontiers in Microbiology. 12: 658943 (2021)
Núñez-Espinoza JF, Martínez-Castañeda FE, Ávila-Pérez F, Rendón-Rendón MC. A structural approach to some contradictions in worldwide swine production and health research. Sustainability. 14: 4748 (2022)
O'Flaherty S, Coffey A, Meaney WJ, Fitzgerald GF, Ross RP. Inhibition of bacteriophage K proliferation on Staphylococcus aureus in raw bovine milk. Letters in Applied Microbiology. 41: 274-279 (2005)
O'Flaherty S, Ross RP, Coffey A. Bacteriophage and their lysins for elimination of infectious bacteria. FEMS Microbiology Reviews. 33: 801-819 (2009)
O'Neill J. (2016). Tackling drug-resistant infections globally: final report and recommendations: Government of the United Kingdom.
Oh J, Giallongo F, Frederick T, Pate J, Walusimbi S, Elias RJ, Wall EH, Bravo D, Hristov AN. Effects of dietary Capsicum oleoresin on productivity and immune responses in lactating dairy cows. Journal of Dairy Science. 98: 6327-6339 (2015)
Olaimat AN, Al-Holy MA, Shahbaz HM, Al-Nabulsi AA, Abu Ghoush MH, Osaili TM, Ayyash MM, Holley RA. Emergence of antibiotic resistance in Listeria monocytogenes isolated from food products: A comprehensive review. Comprehensive Reviews in Food Science and Food Safety. 17: 1277-1292 (2018)
Oliveira NA, Gonçalves BL, Lee SH, Caf O, Corassin CH. Use of antibiotics in animal production and its impact on human health. Journal of Food Chemistry and Nanotechnology. 06: 40-47 (2020)
Pasupuleti M, Schmidtchen A, Malmsten M. Antimicrobial peptides: key components of the innate immune system. Critical Reviews in Biotechnology. 32: 143-171 (2012)
Perdigón G, Fuller R, Raya R. Lactic acid bacteria and their effect on the immune system. Current Issues in Intestinal Microbiology. 2: 27-42 (2001)
Peschel A, Otto M, Jack RW, Kalbacher H, Jung G, Götz F. Inactivation of the dlt operon in Staphylococcus aureus confers sensitivity to defensins, protegrins, and other antimicrobial peptides. Journal of Biological Chemistry. 274: 8405-8410 (1999)
Peterson E, Kaur P. Antibiotic resistance mechanisms in bacteria: Relationships between resistance determinants of antibiotic producers, environmental bacteria, and clinical pathogens. Frontiers in Microbiology. 9: 2928 (2018)
Peterson RM, Huang T, Rudolf JD, Smanski MJ, Shen B. Mechanisms of self-resistance in the platensimycin- and platencin-producing Streptomyces platensis MA7327 and MA7339 strains. Chemistry and Biology. 21: 389-397 (2014)
Piper C, Draper LA, Cotter PD, Ross RP, Hill C. A comparison of the activities of lacticin 3147 and nisin against drug-resistant Staphylococcus aureus and Enterococcus species. Journal of Antimicrobial Chemotherapy. 64: 546-551 (2009)
Pirnay JP, De Vos D, Verbeken G, Merabishvili M, Chanishvili N, Vaneechoutte M, Zizi M, Laire G, Lavigne R, Huys I, Van den Mooter G, Buckling A, Debarbieux L, Pouillot F, Azeredo J, Kutter E, Dublanchet A, Gorski A, Adamia R. The phage therapy paradigm: pret-a-porter or sur-mesure? Pharmaceutical Research. 28: 934-937 (2011)
Pitout JD, Nordmann P, Poirel L. Carbapenemase-producing Klebsiella pneumoniae, a key pathogen set for global nosocomial dominance. Antimicrobial Agents and Chemotherapy. 59: 5873-5884 (2015)
Porter RE, Jr. Bacterial Enteritides of poultry. Poultry Science. 77: 1159-1165 (1998)
Postma M, Vanderhaeghen W, Sarrazin S, Maes D, Dewulf J. Reducing antimicrobial usage in pig production without jeopardizing production parameters. Zoonoses and Public Health. 64: 63-74 (2017)
Price LB, Stegger M, Hasman H, Aziz M, Larsen J, Andersen PS, Pearson T, Waters AE, Foster JT, Schupp J, Gillece J, Driebe E, Liu CM, Springer B, Zdovc I, Battisti A, Franco A, Zmudzki J, Schwarz S, Butaye P, Jouy E, Pomba C, Porrero MC, Ruimy R, Smith TC, Robinson DA, Weese JS, Arriola CS, Yu F, Laurent F, Keim P, Skov R, Aarestrup FM. Staphylococcus aureus CC398: host adaptation and emergence of methicillin resistance in livestock. mBio. 3 (2012)
Principi N, Silvestri E, Esposito S. Advantages and limitations of bacteriophages for the treatment of bacterial Infections. Frontiers in Pharmacology. 10: 513 (2019)
Ramirez MS, Tolmasky ME. Aminoglycoside modifying enzymes. Drug Resistance Updates. 13: 151-171 (2010)
Ray AJ, Pultz NJ, Bhalla A, Aron DC, Donskey CJ. Coexistence of vancomycin-resistant Enterococci and Staphylococcus aureus in the intestinal tracts of hospitalized patients. Clinical Infectious Diseases. 37: 875-881 (2003)
Redgrave LS, Sutton SB, Webber MA, Piddock LJ. Fluoroquinolone resistance: mechanisms, impact on bacteria, and role in evolutionary success. Trends in Microbiology. 22: 438-445 (2014)
Rees DC, Johnson E, Lewinson O. ABC transporters: the power to change. Nature Reviews. Molecular Cell Biology. 10: 218-227 (2009)
Reininghaus EZ, Wetzlmair LC, Fellendorf FT, Platzer M, Queissner R, Birner A, Pilz R, Hamm C, Maget A, Rieger A, Prettenhofer A, Wurm W, Mörkl S, Dalkner N. Probiotic treatment in individuals with euthymic bipolar disorder: A pilot-study on clinical changes and compliance. Neuropsychobiology. 79: 71-79 (2020)
Reygaert WC. An overview of the antimicrobial resistance mechanisms of bacteria. AIMS Microbiology. 4: 482–501 (2018)
Richeson JT, Beck PA, Poe KD, Gadberry MS, Hess TW, Hubbell DS. Effects of administration of a modified-live virus respiratory vaccine and timing of vaccination on health and performance of high-risk beef stocker calves. The Bovine Practitioner. 49: 37-42 (2015)
Richeson JT, Hughes HD, Broadway PR, Carroll JA. Vaccination management of beef cattle: Delayed vaccination and endotoxin stacking. Veterinary Clinics of North America: Food Animal Practice. 35: 575-592 (2019)
Roach DR, Donovan DM. Antimicrobial bacteriophage-derived proteins and therapeutic applications. Bacteriophage. 5: e1062590 (2015)
Roberts MC. Resistance to macrolide, lincosamide, streptogramin, ketolide, and oxazolidinone antibiotics. Molecular Biotechnology. 28: 47-62 (2004)
Robicsek A, Strahilevitz J, Jacoby GA, Macielag M, Abbanat D, Hye Park C, Bush K, Hooper DC. Fluoroquinolone-modifying enzyme: a new adaptation of a common aminoglycoside acetyltransferase. Nature Medicine. 12: 83 (2006)
Roca I, Akova M, Baquero F, Carlet J, Cavaleri M, Coenen S, Cohen J, Findlay D, Gyssens I, Heure OE, Kahlmeter G, Kruse H, Laxminarayan R, Liébana E, López-Cerero L, MacGowan A, Martins M, Rodríguez-Baño J, Rolain JM, Segovia C, Sigauque B, Tacconelli E, Wellington E, Vila J. The global threat of antimicrobial resistance: science for intervention. New Microbes and New Infections 6: 22-29 (2015)
Rojo-Gimeno C, Postma M, Dewulf J, Hogeveen H, Lauwers L, Wauters E. Farm-economic analysis of reducing antimicrobial use whilst adopting improved management strategies on farrow-to-finish pig farms. Preventive Veterinary Medicine. 129: 74-87 (2016)
Sachi S, Ferdous J, Sikder MH, Azizul Karim Hussani SM. Antibiotic residues in milk: Past, present, and future. Journal of Advanced Veterinary and Animal Research. 6: 315-332 (2019)
Saha M, Sarkar A. Review on multiple facets of drug resistance: A rising challenge in the 21st century. Journal of Xenobiotics. 11: 197-214 (2021)
Sauvage E, Kerff F, Terrak M, Ayala JA, Charlier P. The penicillin-binding proteins: structure and role in peptidoglycan biosynthesis. FEMS Microbiology Reviews. 32: 234-258 (2008)
Schmieger H, Schicklmaier P. Transduction of multiple drug resistance of Salmonella enterica serovar typhimurium DT104. FEMS Microbiology Letters. 170: 251-256 (1999)
Selvin J, Maity D, Sajayan A, Kiran GS. Revealing antibiotic resistance in therapeutic and dietary probiotic supplements. Journal of Global Antimicrobial Resistance. 22: 202-205 (2020)
Shu Q, Qu F, Gill HS. Probiotic treatment using Bifidobacterium lactis HN019 reduces weanling diarrhea associated with rotavirus and Escherichia coli infection in a piglet model. Journal of Pediatric Gastroenterology and Nutrition. 33: 171-177 (2001)
Signorini ML, Soto LP, Zbrun MV, Sequeira GJ, Rosmini MR, Frizzo LS. Impact of probiotic administration on the health and fecal microbiota of young calves: a meta-analysis of randomized controlled trials of lactic acid bacteria. Research in Veterinary Science. 93: 250-258 (2012)
Skerlavaj B, Gennaro R, Bagella L, Merluzzi L, Risso A, Zanetti M. Biological characterization of two novel cathelicidin-derived peptides and identification of structural requirements for their antimicrobial and cell lytic activities. Journal of Biological Chemistry. 271: 28375-28381 (1996)
Song KD, Lee WK. Antibacterial activity of recombinant pig intestinal parasite cecropin P4 peptide secreted from Pichia pastoris. Asian Australas Journal of Animal Science. 27: 278-283 (2014)
Souque C, Escudero JA, MacLean RC. Integron activity accelerates the evolution of antibiotic resistance. eLife. 10: e62474 (2021)
Spanogiannopoulos P, Waglechner N, Koteva K, Wright GD. A rifamycin inactivating phosphotransferase family shared by environmental and pathogenic bacteria. Proceedings of the National Academy of Sciences. 111: 7102-7107 (2014)
Srinivasan V, Nguyen LT, Headrick SI, Murinda SE, Oliver SP. Antimicrobial resistance patterns of shiga toxin-producing Escherichia coli O157:H7 and O157:H7- from different origins. Microbial Drug Resistance. 13: 44-51 (2007)
Stalder T, Barraud O, Casellas M, Dagot C, Ploy MC. Integron involvement in environmental spread of antibiotic resistance. Frontiers in Microbiology. 3: 119 (2012)
Szakács G, Váradi A, Ozvegy-Laczka C, Sarkadi B. The role of ABC transporters in drug absorption, distribution, metabolism, excretion and toxicity (ADME-Tox). Drug Discovery Today. 13: 379-393 (2008)
Tang Y, Fang L, Xu C, Zhang Q. Antibiotic resistance trends and mechanisms in the foodborne pathogen, Campylobacter. Animal Health Research Reviews. 18: 87-98 (2017)
Teuber M. Spread of antibiotic resistance with food-borne pathogens. Cellular and Molecular Life Sciences. 56: 755-763 (1999)
Thacker EL. Immunomodulators, immunostimulants, and immunotherapies in small animal veterinary medicine. The Veterinary Clinics of North America. Small Animal Practice. 40: 473-483 (2010)
Thanner S, Drissner D, Walsh F. Antimicrobial resistance in agriculture. mBio. 7: e02227-02215 (2016)
Tóth AG, Csabai I, Judge MF, Maróti G, Becsei Á, Spisák S, Solymosi N. Mobile antimicrobial resistance genes in probiotics. Antibiotics. 10: 1287 (2021)
Tuohy K, Davies M, Rumsby P, Rumney C, Adams MR, Rowland IR. Monitoring transfer of recombinant and nonrecombinant plasmids between Lactococcus lactis strains and members of the human gastrointestinal microbiota in vivo impact of donor cell number and diet. Journal of Applied Microbiology. 93: 954-964 (2002)
Vakili AR, Khorrami B, Mesgaran MD, Parand E. The effects of thyme and cinnamon essential oils on performance, rumen fermentation and blood metabolites in holstein calves consuming high concentrate diet. Asian-Australasian Journal of Animal Sciences. 26: 935-944 (2013)
Van Bambeke F, Balzi E, Tulkens PM. Antibiotic efflux pumps. Biochemical Pharmacology. 60: 457-470 (2000)
Van Boeckel TP, Brower C, Gilbert M, Grenfell BT, Levin SA, Robinson TP, Teillant A, Laxminarayan R. Global trends in antimicrobial use in food animals. Proceedings of the National Academy of Sciences. 112: 5649-5654 (2015)
van Dijk A, Veldhuizen EJ, Haagsman HP. Avian defensins. Veterinary Immunology and Immunopathology. 124: 1-18 (2008)
van Reenen CA, Dicks LM. Horizontal gene transfer amongst probiotic lactic acid bacteria and other intestinal microbiota: what are the possibilities? A review. Archives of Microbiology. 193: 157-168 (2011)
Varankovich NV, Nickerson MT, Korber DR. Probiotic-based strategies for therapeutic and prophylactic use against multiple gastrointestinal diseases. Frontiers in Microbiology. 6: 685 (2015)
Vollmer W, Blanot D, De Pedro MA. Peptidoglycan structure and architecture. FEMS Microbiology Reviews. 32: 149-167 (2008)
Vrancianu CO, Popa LI, Bleotu C, Chifiriuc MC. Targeting plasmids to limit acquisition and transmission of antimicrobial resistance. Frontiers in Microbiology. 11: 761 (2020)
Wall SK, Zhang J, Rostagno MH, Ebner PD. Phage therapy to reduce preprocessing Salmonella infections in market-weight swine. Applied and Environmental Microbiology. 76: 48-53 (2010)
Wang X, Biswas S, Paudyal N, Pan H, Li X, Fang W, Yue M. Antibiotic resistance in Salmonella Typhimurium isolates recovered from the food chain through national antimicrobial resistance monitoring system between 1996 and 2016. Frontiers in Microbiology. 10: 985 (2019)
Watts JEM, Schreier HJ, Lanska L, Hale MS. The rising tide of antimicrobial resistance in aquaculture: Sources, sinks and solutions. Marine Drugs. 15 (2017)
Whenham N, Lu TC, Maidin MB, Wilson PW, Bain MM, Stevenson ML, Stevens MP, Bedford MR, Dunn IC. Ovodefensins, an oviduct-specific antimicrobial gene family, have evolved in birds and reptiles to protect the egg by both sequence and intra-six-cysteine sequence motif spacing. Biology of Reproduction. 92: 154, 151-113 (2015)
Wick LM, Qi W, Lacher DW, Whittam TS. Evolution of genomic content in the stepwise emergence of Escherichia coli O157:H7. Journal of Bacteriology. 187: 1783-1791 (2005)
Windisch W, Schedle K, Plitzner C, Kroismayr A. Use of phytogenic products as feed additives for swine and poultry. Journal of Animal Science. 86: E140-E148 (2008)
Wittebole X, De Roock S, Opal SM. A historical overview of bacteriophage therapy as an alternative to antibiotics for the treatment of bacterial pathogens. Virulence. 5: 226-235 (2014)
Wu S, Zhang F, Huang Z, Liu H, Xie C, Zhang J, Thacker PA, Qiao S. Effects of the antimicrobial peptide cecropin AD on performance and intestinal health in weaned piglets challenged with Escherichia coli. Peptides. 35: 225-230 (2012)
Zalewska M, Blazejewska A, Czapko A, Popowska M. Antibiotics and antibiotic resistance genes in animal manure - consequences of its application in agriculture. Frontiers in Microbiology. 12: 610656 (2021)
Zapun A, Contreras-Martel C, Vernet T. Penicillin-binding proteins and beta-lactam resistance. FEMS Microbiology Reviews. 32: 361-385 (2008)
Zhang W, Sack DA. Progress and hurdles in the development of vaccines against enterotoxigenic Escherichia coli in humans. Expert Review of Vaccines. 11: 677-694 (2012)
Zhao Y, Su JQ, An XL, Huang FY, Rensing C, Brandt KK, Zhu YG. Feed additives shift gut microbiota and enrich antibiotic resistance in swine gut. The Science of the Total Environment. 621: 1224-1232 (2018)
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2016R1D1A3B01008304).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, J., Ahn, J. Emergence and spread of antibiotic-resistant foodborne pathogens from farm to table. Food Sci Biotechnol 31, 1481–1499 (2022). https://doi.org/10.1007/s10068-022-01157-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10068-022-01157-1