Abstract
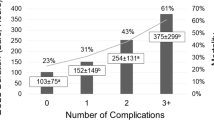
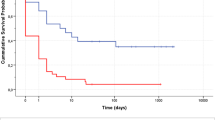
Out-of-hospital extracorporeal membrane oxygenation (ECMO) implantation and ECMO transport have become a growing field useful for emergent treatment of heart or lung failure with increasing number of centers launching such service. This study was designed to present risk factors predicting 30-day mortality for patients receiving ECMO support in a newly launched ECMO retrieval service. From 01/2015 till 01/2017 28 consecutive patients received ECMO support in peripheral hospitals using a miniaturized portable Cardiohelp System® (Maquet, Rastatt Germany) for heart, lung or heart/lung failure as a bridge-to-decision as a part of our newly launched ECMO retrieval service. Outcomes and predictors for 30-day mortality were presented. The mean age was 56 ± 15 (maximum 78) years. The mean ECMO support duration was 97 ± 100 h, whereas 11 patients (40%) were weaned off support and discharged from hospital. Presence of hemolysis (p = 0.041), renal failure (p = 0.016), lower platelet count before ECMO implantation (p = 0.001), and higher lactate 24 h after initiation of support (p = 0.006) were factors associated with 30-day mortality. Initial success of an ECMO retrieval service depends on logistic organization and clinical management. Taking into consideration highly deleterious effects of hemodynamic malperfusion of end organs, rapid initiation of ECMO support is a vital factor for survival. This is highlighted by predictive factors of early mortality that are associated with peripheral organ failure or complications.

Similar content being viewed by others
References
Gray BW, Haft JW, Hirsch JC, Annich GM, Hirschl RB, Bartlett RH. Extracorporeal life support: experience with 2,000 patients. ASAIO J. 2015;61:2–7.
Raspe C, Ruckert F, Metz D, Hofmann B, Neitzel T, Stiller M, et al. Inter-hospital transfer of ECMO-assisted patients with a portable miniaturized ECMO device: 4 years of experience. Perfusion. 2015;30:52–9.
Forrest P, Cheong JY, Vallely MP, Torzillo PJ, Hendel PN, Wilson MK, et al. International retrieval of adults on extracorporeal membrane oxygenation support. Anaesth Intensive Care. 2011;39:1082–5.
Edelman J, Wilson MK, Vallely MP, Bannon PG, McKay G, Robertson SJ, et al. The expanding role of extracorporeal membrane oxygenation retrieval services in Australia. Anaesth Intensive Care. 2017;45:92–3.
Aubin H, Petrov G, Dalyanoglu H, Saeed D, Akhyari P, Paprotny G, et al. A suprainstitutional network for remote extracorporeal life support: a retrospective cohort study. JACC Heart Fail. 2016;4:698–708.
Bryner B, Cooley E, Copenhaver W, Brierley K, Teman N, Landis D, et al. Two decades’ experience with interfacility transport on extracorporeal membrane oxygenation. Ann Thorac Surg. 2014;98:1363–70.
Beurtheret S, Mordant P, Paoletti X, Marijon E, Celermajer DS, Leger P, et al. Emergency circulatory support in refractory cardiogenic shock patients in remote institutions: a pilot study (the cardiac-RESCUE program). Eur Heart J. 2013;34:112–20.
Leick J, Liebetrau C, Szardien S, Fischer-Rasokat U, Willmer M, van Linden A, et al. Door-to-implantation time of extracorporeal life support systems predicts mortality in patients with out-of-hospital cardiac arrest. Clin Res Cardiol. 2013;102:661–9.
Haneya A, Philipp A, Diez C, Schopka S, Bein T, Zimmermann M, et al. A 5-year experience with cardiopulmonary resuscitation using extracorporeal life support in non-postcardiotomy patients with cardiac arrest. Resuscitation. 2012;83:1331–7.
Guenther S, Theiss HD, Fischer M, Sattler S, Peterss S, Born F, et al. Percutaneous extracorporeal life support for patients in therapy refractory cardiogenic shock: initial results of an interdisciplinary team. Interact Cardiovasc Thorac Surg. 2014;18:283–91.
Wang CH, Chou NK, Becker LB, Lin JW, Yu HY, Chi NH, et al. Improved outcome of extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest—a comparison with that for extracorporeal rescue for in-hospital cardiac arrest. Resuscitation. 2014;85:1219–24.
Wengenmayer T, Rombach S, Ramshorn F, Biever P, Bode C, Duerschmied D, et al. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit Care. 2017;21:157.
Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014;371:2309–19.
Ruckert F, Steinke T, Flother L, Bucher M, Metz D, Frantz S, et al. Predictors for quality of life of patients with a portable out-of-centre-implanted extracorporeal membrane oxygenation device. Interact Cardiovasc Thorac Surg. 2017;24:542–48.
Debaty G, Babaz V, Durand M, Gaide-Chevronnay L, Fournel E, Blancher M, et al. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation. 2017;112:1–10.
Slottosch I, Liakopoulos O, Kuhn E, Scherner M, Deppe AC, Sabashnikov A, et al. Lactate and lactate clearance as valuable tool to evaluate ECMO therapy in cardiogenic shock. J Crit Care. 2017;42:35–41.
Arlt M, Philipp A, Voelkel S, Camboni D, Rupprecht L, Graf BM, et al. Hand-held minimised extracorporeal membrane oxygenation: a new bridge to recovery in patients with out-of-centre cardiogenic shock. Eur J Cardiothorac Surg. 2011;40:689–94.
Pabst D, El-Banayosy A, Soleimani B, Brehm CE. Predictors of survival for nonhighly selected patients undergoing resuscitation with extracorporeal membrane oxygenation after cardiac arrest. ASAIO J 2017;64:368–374.
Combes A, Leprince P, Luyt CE, Bonnet N, Trouillet JL, Leger P, et al. Outcomes and long-term quality-of-life of patients supported by extracorporeal membrane oxygenation for refractory cardiogenic shock. Crit Care Med. 2008;36:1404–11.
Ravichandran AK, Parker J, Novak E, Joseph SM, Schilling JD, Ewald GA, et al. Hemolysis in left ventricular assist device: a retrospective analysis of outcomes. J Heart Lung Transplant. 2014;33:44–50.
Shimono T, Makinouchi K, Nose Y. Total erythrocyte destruction time: the new index for the hemolytic performance of rotary blood pumps. Artif Organs. 1995;19:571–5.
Murphy DA, Hockings LE, Andrews RK, Aubron C, Gardiner EE, Pellegrino VA, et al. Extracorporeal membrane oxygenation-hemostatic complications. Transfus Med Rev. 2015;29:90–101.
Williams DC, Turi JL, Hornik CP, Bonadonna DK, Williford WL, Walczak RJ, et al. Circuit oxygenator contributes to extracorporeal membrane oxygenation-induced hemolysis. ASAIO J. 2015;61:190–5.
Lehle K, Philipp A, Zeman F, Lunz D, Lubnow M, Wendel HP, et al. Technical-induced hemolysis in patients with respiratory failure supported with veno-venous ECMO—prevalence and risk factors. PLoS One. 2015;10:e0143527.
Dalton HJ, Garcia-Filion P, Holubkov R, Moler FW, Shanley T, Heidemann S, et al. Association of bleeding and thrombosis with outcome in extracorporeal life support. Pediatr Crit Care Med. 2015;16:167–74.
Sy E, Sklar MC, Lequier L, Fan E, Kanji HD. Anticoagulation practices and the prevalence of major bleeding, thromboembolic events, and mortality in venoarterial extracorporeal membrane oxygenation: a systematic review and meta-analysis. J Crit Care. 2017;39:87–96.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Djordjevic, I., Sabashnikov, A., Deppe, A.C. et al. Risk factors associated with 30-day mortality for out-of-center ECMO support: experience from the newly launched ECMO retrieval service. J Artif Organs 22, 110–117 (2019). https://doi.org/10.1007/s10047-019-01092-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-019-01092-9