Abstract
Purpose
This study evaluated the effects of advanced platelet-rich fibrin (A-PRF +) on the healing of upper third molar post-extraction sockets.
Methods
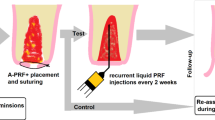
Sixteen patients who underwent extractions of the upper third molars (18 and 28) were included in this randomized split-mouth study. The alveoli on the test side were filled with A-PRF + , while the control side was maintained with blood clot. The side that received treatment was randomly defined. Alveolar bone regeneration was evaluated by CBCT scans to assess healing stage, bone density, and fractal analysis 1 week and 90 days post-extraction. Additionally, pain, edema, bleeding, and soft tissue alveolar repair were evaluated by clinical analyses 3, 7, 14, 30, and 90 days after the surgical procedure using a visual analog scale.
Results
There were no clinical differences regarding treatments in any experimental period. In the tomographic evaluation, at 7 days, the alveoli treated with A-PRF + presented a suggestive sign of higher bone density than the control alveoli, which was not confirmed 90 days after the surgical procedure.
Conclusion
Thus, the use of A-PRF + does not demonstrate a clinical advantage in the repair of post-extraction sockets of upper third molars.





Similar content being viewed by others
References
Contar CM, de Oliveira P, Kanegusuku K, Berticelli RD, Azevedo-Alanis LR, Machado MA (2010) Complications in third molar removal: a retrospective study of 588 patients. Med Oral Patol Oral Cir Bucal 15:e74–e78. https://doi.org/10.4317/medoral.15.e74
Kiencalo A, Jamka-Kasprzyk M, Panas M, Wyszynska-Pawelec G (2021) Analysis of complications after the removal of 339 third molars. Dent Med Probl 58:75–80. https://doi.org/10.17219/dmp/127028
Bui CH, Seldin EB, Dodson TB (2003) Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg 61:1379–1389. https://doi.org/10.1016/j.joms.2003.04.001
Claudia A, Barbu HM, Adi L, Gultekin A, Reiser V, Gultekin P, Mijiritsky E (2018) Relationship between third mandibular molar angulation and distal cervical caries in the second molar. J Craniofac Surg 29:2267–2271. https://doi.org/10.1097/SCS.0000000000004505
Patil S, Halgatti V, Khandelwal S, Santosh BS, Maheshwari S (2014) Prevalence of cysts and tumors around the retained and unerupted third molars in the Indian population. J Oral Biol Craniofac Res 4:82–87. https://doi.org/10.1016/j.jobcr.2014.07.003
Phillips C, White RP Jr, Shugars DA, Zhou X (2003) Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J Oral Maxillofac Surg 61:1436–1448. https://doi.org/10.1016/j.joms.2003.08.003
Hassan B, Al-Khanati NM, Bahhah H (2020) Effect of lingual-based flap design on postoperative pain of impacted mandibular third molar surgery: Split-mouth randomized clinical trial. Med Oral Patol Oral Cir Bucal 25:e660–e667. https://doi.org/10.4317/medoral.23666
Chaparro-Avendano AV, Perez-Garcia S, Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C (2005) Morbidity of third molar extraction in patients between 12 and 18 years of age. Med Oral Patol Oral Cir Bucal 10:422–431
Avellaneda-Gimeno V, Figueiredo R, Valmaseda-Castellon E (2017) Quality of life after upper third molar removal: a prospective longitudinal study. Med Oral Patol Oral Cir Bucal 22:e759–e766. https://doi.org/10.4317/medoral.21781
Daugela P, Grimuta V, Sakavicius D, Jonaitis J, Juodzbalys G (2018) Influence of leukocyte- and platelet-rich fibrin (L-PRF) on the outcomes of impacted mandibular third molar removal surgery: a split-mouth randomized clinical trial. Quintessence Int 49:377–388. https://doi.org/10.3290/j.qi.a40113
Kahraman SA, Cetiner S, Strauss RA (2017) The effects of transcutaneous and intraoral low-level laser therapy after extraction of lower third molars: a randomized single blind, placebo controlled dual-center study. Photomed Laser Surg 35:401–407. https://doi.org/10.1089/pho.2016.4252
Crisci A, Marotta G, Licito A, Serra E, Benincasa G, Crisci M (2018) Use of leukocyte platelet (L-PRF) rich fibrin in diabetic foot ulcer with osteomyelitis (three clinical cases report). Diseases 24;6(2):30. https://doi.org/10.3390/diseases6020030
Durmuslar MC, Balli U, Ongoz Dede F, Bozkurt Dogan S, Misir AF, Baris E, Yilmaz Z, Celik HH, Vatansever A (2016) Evaluation of the effects of platelet-rich fibrin on bone regeneration in diabetic rabbits. J Craniomaxillofac Surg 44:126–133. https://doi.org/10.1016/j.jcms.2015.11.009
Temmerman A, Vandessel J, Castro A, Jacobs R, Teughels W, Pinto N, Quirynen M (2016) The use of leucocyte and platelet-rich fibrin in socket management and ridge preservation: a split-mouth, randomized, controlled clinical trial. J Clin Periodontol 43(11):990–999. https://doi.org/10.1111/jcpe.12612
Clark D, Rajendran Y, Paydar S, Ho S, Cox D, Ryder M, Dollard J, Kao RT (2018) Advanced platelet-rich fibrin and freeze-dried bone allograft for ridge preservation: a randomized controlled clinical trial. J Periodontol 89:379–387. https://doi.org/10.1002/JPER.17-0466
Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part V: histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:299–303. https://doi.org/10.1016/j.tripleo.2005.07.012
Varghese MP, Manuel S, Kumar LKS (2017) Potential for osseous regeneration of platelet-rich fibrin-a comparative study in mandibular third molar impaction sockets. J Oral Maxillofac Surg 75:1322–1329. https://doi.org/10.1016/j.joms.2017.01.035
Norholt SE, Hartlev J (2016) Surgical treatment of osteonecrosis of the jaw with the use of platelet-rich fibrin: a prospective study of 15 patients. Int J Oral Maxillofac Surg 45:1256–1260. https://doi.org/10.1016/j.ijom.2016.04.010
Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T (2014) Classification of platelet concentrates (platelet-rich plasma-PRP, platelet-rich fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J 4:3–9
Fujioka-Kobayashi M, Miron RJ, Hernandez M, Kandalam U, Zhang Y, Choukroun J (2017) Optimized platelet-rich fibrin with the low-speed concept: growth factor release, biocompatibility, and cellular response. J Periodontol 88:112–121. https://doi.org/10.1902/jop.2016.160443
Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, Landes C, Sader R, Kirkpatrick C, Choukroun J (2014) Advanced platelet-rich fibrin: a new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implantol 40:679–689. https://doi.org/10.1563/aaid-joi-D-14-00138
Heo MS, Park KS, Lee SS, Choi SC, Koak JY, Heo SJ, Han CH, Kim JD (2002) Fractal analysis of mandibular bony healing after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 94:763–767. https://doi.org/10.1067/moe.2002.128972
White SC, Rudolph DJ (1999) Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88:628–635. https://doi.org/10.1016/s1079-2104(99)70097-1
Franchini M, Cruciani M, Mengoli C, Masiello F, Marano G, D’Aloja E, Dell’Aringa C, Pati I, Veropalumbo E, Pupella S, Vaglio S, Liumbruno GM (2019) The use of platelet-rich plasma in oral surgery: a systematic review and meta-analysis. Blood Transfus 7:357–367. https://doi.org/10.2450/2019.0177-19
Kim TH, Kim SH, Sandor GK, Kim YD (2014) Comparison of platelet-rich plasma (PRP), platelet-rich fibrin (PRF), and concentrated growth factor (CGF) in rabbit-skull defect healing. Arch Oral Biol 59:550–558. https://doi.org/10.1016/j.archoralbio.2014.02.004
Lektemur Alpan A, Torumtay Cin G (2020) PRF improves wound healing and postoperative discomfort after harvesting subepithelial connective tissue graft from palate: a randomized controlled trial. Clin Oral Investig 24:425–436. https://doi.org/10.1007/s00784-019-02934-9
Andreone A, den Hollander D (2019) A retrospective study on the use of dermis micrografts in platelet-rich fibrin for the resurfacing of massive and chronic full-thickness burns. Stem Cells Int 15:8636079. https://doi.org/10.1155/2019/8636079
Pichotano EC, de Molon RS, de Souza RV, Austin RS, Marcantonio E, Zandim-Barcelos DL (2019) Evaluation of L-PRF combined with deproteinized bovine bone mineral for early implant placement after maxillary sinus augmentation: a randomized clinical trial. Clin Implant Dent Relat Res 21:253–262. https://doi.org/10.1111/cid.12713
Andrade C, Camino J, Nally M, Quirynen M, Martinez B, Pinto N (2020) Combining autologous particulate dentin, L-PRF, and fibrinogen to create a matrix for predictable ridge preservation: a pilot clinical study. Clin Oral Investig 24:1151–1160. https://doi.org/10.1007/s00784-019-02922-z
Aravena PC, Sandoval SP, Pizarro FE, Simpson MI, Castro-Adams N, Serandour G, Rosas C (2021) Leukocyte and platelet-rich fibrin have same effect as blood clot in the 3-dimensional alveolar ridge preservation. A split-mouth randomized clinical trial. J Oral Maxillofac Surg 79:575–584. https://doi.org/10.1016/j.joms.2020.10.006
Lei L, Yu Y, Han J, Shi D, Sun W, Zhang D, Chen L (2020) Quantification of growth factors in advanced platelet-rich fibrin and concentrated growth factors and their clinical efficacy as adjunctive to the GTR procedure in periodontal intrabony defects. J Periodontol 91:462–472. https://doi.org/10.1002/JPER.19-0290
Giudice A, Antonelli A, Muraca D, Fortunato L (2020) Usefulness of advanced-platelet rich fibrin (A-PRF) and injectable-platelet rich fibrin (i-PRF) in the management of a massive medication-related osteonecrosis of the jaw (MRONJ): a 5-years follow-up case report. Indian J Dent Res 31:813–818. https://doi.org/10.4103/ijdr.IJDR_689_19
Funding
This study was funded by the National Council for Scientific and Technological Development (CNPq—Conselho Nacional de Desenvolvimento Científico e Tecnológico) (Project 426954–2018-1).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Davisson Alves Pereira, Pedro Gomes Junqueira Mendes, Nuryê Rezende Prisinoto, Gabriella Lopes de Rezende Barbosa, and Priscilla Barbosa Ferreira Soares. The first draft of the manuscript was written by Davisson Alves Pereira and Guilherme José Pimentel Lopes de Oliveira and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Research Ethics Committee of the Federal University of Uberlândia under protocol number CAAE: 37924720.3.0000.5152 and it was registered in the Brazilian Registry of Clinical Trials (REBEC) under number U1111-1263–9675.
Consent to participate
All individuals who participated in this study signed an informed consent form.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pereira, D.A., Mendes, P.G.J., Prisinoto, N.R. et al. Advanced platelet-rich-fibrin (A-PRF +) has no additional effect on the healing of post-extraction sockets of upper third molars. A split mouth randomized clinical trial. Oral Maxillofac Surg 27, 411–419 (2023). https://doi.org/10.1007/s10006-022-01075-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-022-01075-w