Abstract
Purpose
This study aims to identify whether dental implants placed using a flapless technique have a higher early failure rate, defined as failure within 6 months of placement, compared to implants placed with flap elevation when a surgical guide is not used.
Methods
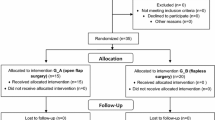
A retrospective cohort study was conducted to evaluate implants placed with either flapless (FL) or mucoperiosteal flap (MF) surgery between 2006 and 2012 at the Philadelphia VA Medical Center (PVAMC). Implant status after FL or MF surgery was assessed using dental encounter and radiographs at subsequent follow-up appointments to assess for early implant failures within 6 months of implant placement.
Results
The FL technique was used to place 89 implants in 38 subjects, while the MF technique was used to place 381 implants in 139 subjects. Early failure occurred in 37 implants, of which 13 occurred in the FL group and 24 occurred in the MF group. FL surgery was found to be associated with a 265% increase in early implant failure (OR 2.653; 95% CL 1.287–5.469) and was statistically significant (p = 0.0064). Residents were over 200% more likely to have an early implant failure when using the FL technique (OR 2.314; 95% CL 1.112–4.816),
Conclusions
Analysis revealed flapless implant placement was associated with higher early implant failure rates. In addition, early failures were more likely to occur when residents placed an implant using the flapless technique. While FL surgery can result in long-term success, it is a more technique-sensitive approach that requires greater clinical skill and stricter case selection to perform.
Similar content being viewed by others
Data Availability
The datasets used and analyzed during this study are available from the corresponding author on reasonable request.
Code availability
The datasets used and analyzed during this study are available from the corresponding author on reasonable request.
References
Jeong SM, Choi BH, Kim J, Xuan F, Lee DH, Mo DY, Lee CU (2011) A 1-year prospective clinical study of soft tissue conditions and marginal bone changes around dental implants after flapless implant surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111(1):41–46. https://doi.org/10.1016/j.tripleo.2010.03.037
Kim JI, Choi BH, Li J, Xuan F, Jeong SM (2009) Blood vessels of the peri-implant mucosa: a comparison between the flap and flapless procedures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:508–512
You TM, Choi BH, Li J, Xuan F, Jeong SM, Jang SO (2009) Morpho- genesis of the peri-implant mucosa: a comparison between flap and flapless procedures in the canine mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:66–70
Van Steenberghe D, Glauser R, Blomback U, Andersson M, Schutyser F, Pettersson A et al (2005) A computed tomographic scan-derived customized surgical template and fixed pros- thesis for flapless surgery and immediate loading of implants in fully edentulous max- illae: a prospective multicenter study. Clin Implant Dent Relat Res 7(Suppl 1):111–120
Marra R, Acocella A, Rispoli A, Sacco R, Ganz SD, Blasi A (2013) Full-mouth rehabilitation with immediate loading of implants inserted with computer-guided flap-less surgery: a 3- year multicenter clinical evaluation with oral health impact profile. Implant Dent 22:444–452
Barone A, Toti P, Piatelli A, Lezzi G, Derchi G, Covani U (2014) Extraction socket healing in humans after ridge preservation techniques: a comparison between flapless and flapped procedure in a randomized clinical trial. J Periodontol 85:14–23
Lemos CAA, Verri FR, Cruz RS, Gomes JML, Dos Santos DM, Goiato MC, Pellizzer EP (2020) Comparison between flapless and open-flap implant placement: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 49(9):1220–1231
Chrcanovic BR, Albrektsson T, Wennerberg A. Flapless versus conventional flapped dental implant surgery: a meta-analysis. PLoS One 2014;9(6)e100624.
Sunitha RV, Sapthagiri E (2013) Flapless implant surgery: a 2-year follow-up study of 40 implants. Oral Surg Oral Med Oral Pathol Oral Radiol 116(4):e237–e243
Lin GH, Chan HL, Bashutski JD, Oh TJ, Wang HL (2014) The effect of flapless surgery on implant survival and marginal bone level: a systematic review and meta-analysis. J Periodontol 85:e91-103
Albrektsson T, Zarb G, Worthington P, Eriksson AR (1986) The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1(1):11–25
Do TA, Le HS, Shen YW, Huang HL, Fuh LJ (2020) Risk factors related to late failure of dental implant—a systematic review of recent studies. Int J Environ Res 17(11):3931
Golub LM, Lee HM, Greenwald RA, Ryan ME, Sorsa T, Salo T, Giannobile WV (1997) A matrix metalloproteinase inhibitor reduces bone-type collagen degradation fragments and specific collagenases in gingival crevicular fluid during adult periodontitis. Inflamm Res 46(8):310–319
Cannizzaro G, Felice P, Leone M, Checchi V, Esposito M (2011) Flapless versus open flap implant surgery in partially edentulous patients subjected to immediate loading: 1-year results from a split-mouth randomised con- trolled trial. Eur J Oral Implantol 4(3):177–188
Wang F, Huang W, Zhang Z, Wang H, Monje A, Wu Y. Minimally invasive flapless vs. flapped approach for single implant placement: a 2-year randomized controlled clinical trial. Clin Oral Implants Res 2017;28 (6):757–64.
Katsoulis J, Avrampou M, Spycher C, Stipic M, Enkling N et al (2012) Comparison of implant stability by means of resonance frequency analysis for flapless and conventionally inserted implants. Clin Implant Dent Relat Res 14:915–923
Rousseau P (2010) Flapless and traditional dental implant surgery: an open, retrospective comparative study. J Oral Maxillofac Surg 68:2299–2306
Campelo LD, Camara JR. Flapless implant surgery: a 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants. 2002 Mar-Apr;17(2):271–6.
Eriksson AR, Albrektsson T (1983) Temperature threshold levels for heat-induced bone tissue injury: a vital-microscopic study in the rabbit. J Prosthet Dent 50(1):101–107
Chiapasco M, Zaniboni M (2009) Clinical outcomes of GBR procedures to correct peri-implant dehiscences and fenestrations: a systematic review. Clin Oral Implants Res 20(Suppl 4):113–123
Venza I, Visalli M, Cucinotta M et al (2010) Proinflammatory gene expression at chronic periodontitis and peri-implantitis sites in patients with or without type 2 diabetes. J Periodontal 81:99
Al-Askar M, Ajlan S, Alomar N, Al-Daghri NM (2018) Clinical and radiographic peri-implant parameters and whole salivary interleukin-1b and interleukin-6 levels among type-2 diabetic and nondiabetic patients with and without peri-implantitis. Med Principles Pract 27:133
Halpern LR, Adams DR (2021) Medically complex dental implant patients: controversies about systemic disease and dental implant success/survival. Dent Clin North Am 65(1):1–19
Eber RM. Increasing levels of smoking may increase the relative risk of dental implant failure. J Evid Based Dent Pract. 2020 Dec;20(4):101493.
Chrcanovic BR, Albrektsson T, Wennerberg A (2015) Smoking and dental implants: a systematic review and meta-analysis. J Dent 43(5):487–498
Wang F, Wang Q, Zhang J (2021) Role of dynamic navigation systems in enhancing the accuracy of implant placement: a systematic review and meta-analysis of clinical studies. J Oral Maxillofac Surg 79(10):2061–2070
Van Doorne L, De Kock L, De Moor A, Shtino R, Bronkhorst E, Meijer G, De Bruyn H. Flaplessly placed 2.4-mm mini-implants for maxillary overdentures: a prospective multicentre clinical cohort study. Int J Oral Maxillofac Surg. 2020 Mar;49(3):384–391.
Arisan V, Karabuda CZ, Ozdemir T (2010) Implant surgery using bone- and mucosa-supported stereolithographic guides in totally edentulous jaws: surgical and post-operative outcomes of computer-aided vs. standard techniques. Clin Oral Implants Res 21:980–988
Sunitha RV, Sapthagiri E (2013) Flapless implant surgery: a 2-year follow-up study of 40 implants. Oral Surg Oral Med Oral Pathol Oral Radiol 116:e237–e243
Wood DL, Hoag PM, Donnenfeld OW, Rosenfeld LD (1972) Alveolar crest reduction following full and partial thickness flaps. J Periodontol 42:141–144
De Bruyn H, Atashkadeh M, Cosyn J, van de Velde T (2011) Clinical outcome and bone preservation of single TiUnit implants installed with flapless or flap surgery. Clin Implant Dent Relat Res 13:175–183
Covani U, Cornelini R, Barone A (2008) Buccal bone augmentation around immediate implants with and without flap elevation: a modified approach. Int J Oral Maxillofac Implants 23:841–846
Van de Velde T, Sennerby L, De Bruyn H (2010) The clinical and radiographic outcome of implants placed in the posterior maxilla with a guided flapless approach and immediately restored with a provisional rehabilitation: a randomized clinical trial. Clin Oral Implants Res 21:1223–1233
Acknowledgements
This material is the result of work supported with resources and the use of facilities at the Corporal Michael J. Crescenz VA Medical Center, Philadelphia, PA. The contents do not represent the view of the United States Department of Veterans Affairs or the US Government.
Author information
Authors and Affiliations
Contributions
BC, WB, JG, PR, and JC were major contributors in gathering and organizing the data for the dataset. SC and BC were major contributors in analyzing the dataset. NP and BF oversaw the data collection and data analysis, in addition to helping set up the database. BC was a major contributor in writing the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research on dental implants has been approved by Human Studies Subcommittee (IRB I) and all relevant Research & Development (R&D) committees and subcommittees at the Philadelphia Veterans Affairs Medical Center (ID: 01732 Prom#:0001).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Carr, B.R., Rekawek, P., Gulko, J.A. et al. Does implant placement using a minimally invasive technique increase early failures among trainees at an academic center?. Oral Maxillofac Surg 27, 245–250 (2023). https://doi.org/10.1007/s10006-022-01057-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-022-01057-y